Warfarin Dosing Calculator
How This Works
Based on CPIC guidelines, this calculator estimates your initial warfarin dose using your genetic profile. It accounts for CYP2C9 and VKORC1 variants that significantly affect drug metabolism and sensitivity. The tool provides a personalized dose recommendation and bleeding risk assessment.
Results will appear here after calculation
When you’re prescribed warfarin, you’re not just getting a blood thinner-you’re getting a drug that reacts differently in every person’s body. Two genes, CYP2C9 and VKORC1, hold the key to why some people bleed easily on low doses while others need double the amount just to stay safe. This isn’t guesswork. It’s biology. And if you or someone you know is on warfarin, understanding these genes could mean the difference between a stable INR and a trip to the ER.
What Warfarin Does-and Why It’s So Tricky
Warfarin has been around since the 1950s. It works by blocking VKORC1, the enzyme your liver uses to recycle vitamin K. Without that recycling, your blood can’t make clotting factors properly. That’s the goal: slow clotting to prevent strokes or clots. But here’s the catch: the window between too little and too much is razor-thin. A single INR above 4.0 can lead to dangerous bleeding. Below 2.0, and you’re not protected from clots. Most people stay in that narrow range less than two-thirds of the time, even with weekly blood tests.
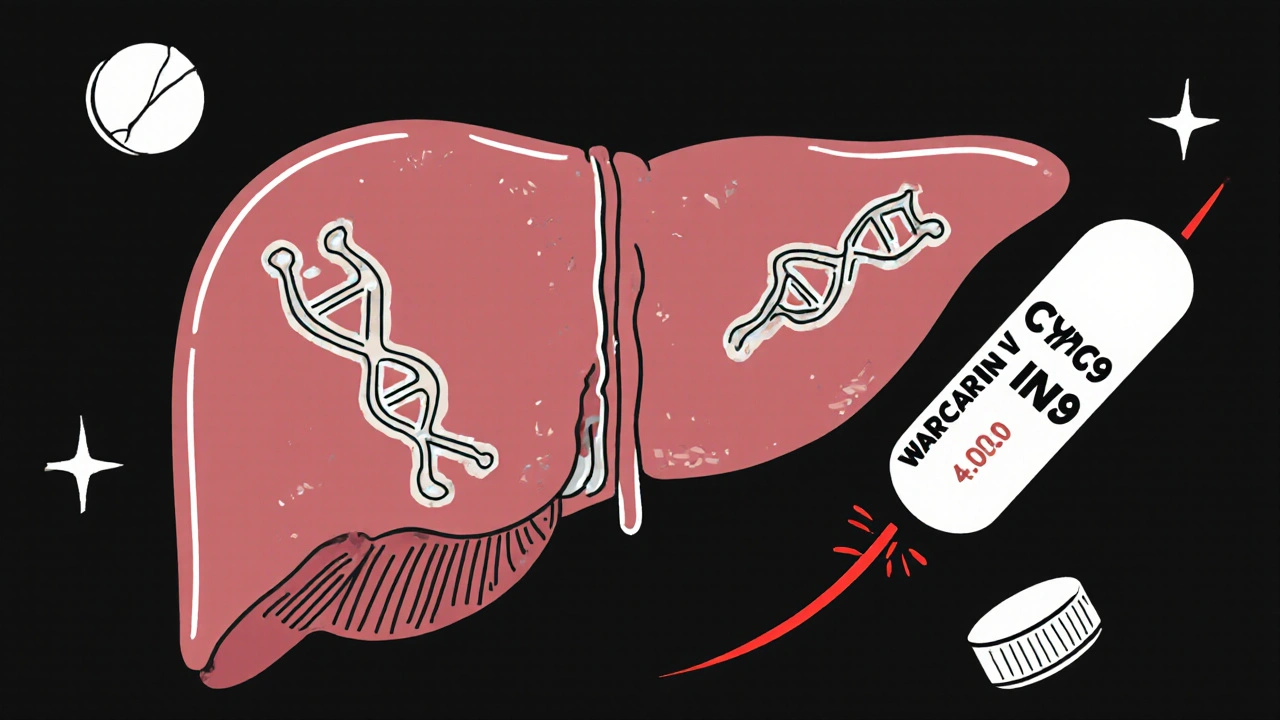
That’s where genetics step in. Two specific genes control how your body handles warfarin: one tells your body how fast it breaks the drug down, and the other tells it how sensitive it is to the drug in the first place.
CYP2C9: The Metabolism Gene
CYP2C9 is the enzyme that breaks down the more powerful half of warfarin-the S-enantiomer. This part is about five times stronger than the R-form. If your CYP2C9 gene has a variant, like *2 or *3, your body slows down this breakdown. That means warfarin builds up faster than expected.
People with the CYP2C9*3 variant clear S-warfarin up to 80% slower than those with the normal gene. That’s not a small difference. It’s enough to push someone into dangerous INR levels within days. In one study, 68% of patients with these variants had an INR above 4 during their first three months, compared to just 42% of those without the variant. That’s nearly 60% higher risk of bleeding that needs medical care.
One Reddit user, u/WarfarinWarrior, shared their story: after genetic testing revealed they carried CYP2C9*3, their dose dropped from 5 mg to 2.5 mg. Their INR, which had been all over the place for six months, finally stabilized. That’s not luck. That’s precision.
VKORC1: The Sensitivity Gene
VKORC1 is the actual target of warfarin. If your VKORC1 gene has a certain variant-specifically the -1639G>A (rs9923231)-your body becomes way more sensitive to the drug. The AA genotype means your enzyme doesn’t work as well, even without warfarin. So when you take the drug, it hits harder.
Someone with the AA genotype might need only 5 to 7 mg per week. Someone with the GG genotype? 28 to 42 mg per week. That’s a 70% difference. And if you’re started on a standard 5 mg daily dose without knowing your genotype, you’re basically playing Russian roulette with your bleeding risk.
One user, u/ClottingConfused, got tested and found they were AA genotype. Their doctor still started them on the usual dose. Two weeks later, they ended up in the ER with an INR of 6.2. That’s not negligence-it’s ignorance. And it’s still common.
When Both Genes Work Against You
The real danger comes when you have both bad variants: CYP2C9*3 and VKORC1 AA. Together, they make you extremely sensitive to warfarin. A 2020 review found these patients had an 83% higher chance of having a dangerously high INR in the first week of treatment. Their risk of bleeding isn’t just higher-it’s explosive.
Studies show that people with this combo take nearly twice as long to reach a stable dose. They need more frequent blood tests. They’re more likely to be hospitalized. And they’re far more likely to need reversal agents like vitamin K or fresh frozen plasma.
Genetic Testing: Is It Worth It?
The data says yes. The EU-PACT trial, published in The Lancet in 2013, showed that using genetic info to guide the first dose reduced major bleeding by 32% in the first 90 days. More recent data from 2025 confirms that genotype-guided dosing cuts major bleeding by 27% during the first three months.
But here’s the problem: only 5 to 15% of U.S. patients get tested before starting warfarin. Why? Cost, access, and confusion. A test costs $250 to $500 out of pocket. Medicare covers it under CPT codes 81225 and 81227, but private insurers often don’t. And many doctors don’t know how to interpret the results.
A 2023 survey found only 38% of primary care doctors could correctly explain how CYP2C9*3 affects warfarin metabolism. That’s not just a knowledge gap-it’s a safety gap.
What the Guidelines Say
The Clinical Pharmacogenetics Implementation Consortium (CPIC) has clear guidelines: test for CYP2C9 and VKORC1 before starting warfarin if you’re likely to be on it long-term. They even have a dosing algorithm that groups patients into low, medium, or high dose categories based on genotype, age, weight, and other meds.
But not everyone agrees. The American College of Chest Physicians says the evidence isn’t strong enough to recommend routine testing. The FDA includes genetic info on the warfarin label, but doesn’t require testing. It’s a mess.
What’s clear? For high-risk patients-older adults, those with prior bleeding, or people on multiple interacting drugs-genetic testing isn’t optional. It’s essential.
What About DOACs?
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban don’t need genetic testing. They’re easier to use. That’s why warfarin use has dropped from 68% to 42% in new atrial fibrillation cases since 2010.
But warfarin isn’t going away. It’s still the only option for people with mechanical heart valves. It’s also cheaper and reversible. Vitamin K or prothrombin complex concentrate can reverse it fast. DOACs? Reversal agents exist, but they’re expensive and not always available.
For patients who need long-term anticoagulation-say, for life after a clot-warfarin’s low cost and reversibility still make sense. And if you’re going to take it for years, minimizing bleeding risk with genetics makes perfect sense.

Real-World Impact: More Than Numbers
A 2022 survey of over 1,200 warfarin users found that 74% of those who had genetic testing reported higher satisfaction with their treatment. Their average satisfaction score was 7.8 out of 10. Those without testing? 6.2. The difference? Not just in numbers-it’s in peace of mind.
Patients who get tested feel more in control. They understand why their dose changed. They’re less likely to skip blood tests. And they’re less likely to panic when their INR shifts.
One patient told me: “I used to dread my INR checks. Now I know why I’m on 3 mg instead of 5. My doctor didn’t guess. They knew.” That’s the power of genetics.
What You Can Do
If you’re starting warfarin:
- Ask your doctor if genetic testing is available and covered by your insurance.
- If you’ve had unstable INRs, bleeding, or trouble finding the right dose, ask if you’ve been tested.
- Request your results. Don’t assume your doctor remembers them.
- Keep a copy of your genotype report. It matters for future meds too-CYP2C9 affects dozens of other drugs.
If you’re already on warfarin and struggling:
- It’s not too late. Get tested now. Your dose can still be adjusted.
- Ask your pharmacist or hematologist to review your genotype with you.
- Use apps or tools that track INR and dose history-many integrate with genetic data.
The Future Is Personalized
By 2030, 60% of new warfarin users are expected to get genetic testing. Costs are falling-under $100 by 2027. New networks like WaGIN are launching to track outcomes across tens of thousands of patients. The evidence is stacking up.
Warfarin isn’t perfect. But it’s still vital. And genetics isn’t a luxury-it’s the missing piece that turns guesswork into science.
If you’re on warfarin, don’t accept random dosing. Ask for your genes. Your body already knows how to respond. It’s time your doctor listened.
15 Comments
Allison Reed
November 26 2025
Just got my CYP2C9*3 result last month-was on 6mg and bleeding through tissues. Down to 2.5mg and my INR’s been rock solid for 4 months. I used to hate blood draws. Now I look forward to them. Genetics saved my life.
Stop guessing. Get tested.
Jacob Keil
November 28 2025
so like… if your genes say u r sensitive to warfarin does that mean ur body is just weak or is this like… evolution failing us? why dont we all just take the new drugs? this feels like medical witchcraft tbh
Rosy Wilkens
November 29 2025
Let me guess-this ‘genetic testing’ is just another Big Pharma ploy to sell more tests while keeping the real solution (vitamin K supplements) off the market. The FDA doesn’t require it? That’s because they’re in bed with the labs. My cousin’s doctor pushed this same ‘precision medicine’ nonsense before prescribing her a dangerous cocktail of anticoagulants. She’s now on a feeding tube.
Wake up. This isn’t science. It’s profit.
Andrea Jones
November 29 2025
Okay but imagine if your doctor just handed you a pill and said ‘good luck’-and then you bled out because they didn’t know your genes? That’s not medicine, that’s Russian roulette with a stethoscope.
And hey-this isn’t just about warfarin. CYP2C9 affects like 20 other meds. Your migraine pill? Your antidepressant? Your painkiller? All of them. So yeah, get tested once. Save yourself 100 future headaches.
Also-shoutout to u/WarfarinWarrior. You’re my hero.
Justina Maynard
November 30 2025
My grandma’s INR spiked to 7.1 after her doc gave her 5mg because ‘everyone starts there.’ She ended up with a brain bleed. The ER doc said, ‘We didn’t know she was AA genotype.’ We had to fight for two weeks to get the test done. Turns out, her dad had the same issue-he died at 68 from a spontaneous hemorrhage.
So no, this isn’t theoretical. It’s family history written in DNA.
And yes, I’m still mad.
Also, I just got my own results. CYP2C9*3 + VKORC1 AA. I’m on 1.5mg. My doc looked at me like I was from Mars. He’s now Googling CPIC guidelines while I’m sipping tea.
Evelyn Salazar Garcia
December 1 2025
Why are we still using warfarin? DOACs exist. They’re safer. Cheaper long-term. Why are we clinging to 1950s tech? This whole post feels like a glorified ad for genetic testing companies.
Clay Johnson
December 3 2025
Genetics doesn’t change biology. It reveals it.
Warfarin was never meant to be dosed by weight or age.
It was meant to be dosed by enzyme activity.
We ignored that for 70 years.
Now we’re surprised people bleed?
Jermaine Jordan
December 4 2025
Imagine this: You’re a doctor. You’ve got 8 minutes with a patient. You’re tired. You’re overwhelmed. You’re told to ‘start at 5mg.’ You do. You don’t know about CYP2C9*3 because your med school didn’t teach it. And now someone’s in the ER because of a system failure-not because you’re a bad doctor.
This isn’t about blame.
This is about fixing the system.
Test. Train. Standardize. Or keep burying people in silence.
Chetan Chauhan
December 6 2025
in india we dont even have access to warfarin testing. we get the same dose as americans. my uncle had a stroke because his INR was 1.8. then he bled into his knee because they upped it to 7.5mg. no testing. no data. just luck. this is rich people medicine. and you want us to feel guilty for not having it? laughable.
Phil Thornton
December 6 2025
My INR was 5.3. ER. Vitamin K. 3 days in hospital.
Got tested after.
CYP2C9*3 / VKORC1 AA.
Now I’m on 2mg.
Peace of mind? Yes.
Still hate needles.
But I’m alive.
Pranab Daulagupu
December 7 2025
As someone from a country where genetic testing is rare, I see the value here. But we need low-cost, scalable models. Not just for the U.S. My cousin in rural Punjab needs this too. Maybe community labs? Mobile phlebotomy? AI-guided dosing via SMS? We can’t wait for insurance to catch up. The tech exists. We need the will.
Barbara McClelland
December 8 2025
Okay, real talk-this is the kind of info that should be on the warfarin bottle. Like ‘Warning: May cause bleeding if you have CYP2C9*3.’
Also, if you’re on warfarin and haven’t been tested, don’t panic. Just ask your pharmacist for a referral. It’s not expensive. It’s not magic. It’s just… smart.
And if your doc says ‘we don’t do that here’? Go to a hematologist. They’ll know what to do.
You deserve to be treated like a person, not a statistic.
Alexander Levin
December 10 2025
Genetic testing? LOL. Next they’ll tell us to test for ‘sun sensitivity’ before taking aspirin. This is all a scam. I’ve been on warfarin for 12 years. Never had a problem. My INR’s always 2.4. They just want your money. 🤡
Ady Young
December 11 2025
I work in a rural clinic. We started offering CYP2C9/VKORC1 testing last year through a grant. We did 47 tests. 18 patients had high-risk genotypes. 12 of them had been on warfarin for over a year with unstable INRs. After adjusting doses based on genetics? Zero major bleeds in 8 months.
It’s not perfect. But it’s better.
And it’s not expensive when you’re doing it right.
Just sayin’.
Travis Freeman
December 12 2025
I’m from Nigeria. We use warfarin because DOACs cost more than a month’s rent. But here’s what I’ve seen: the people who survive are the ones who know their family history. ‘My uncle bled out.’ ‘My aunt had to get transfusions.’ They ask questions. They push back.
Genetics isn’t just about SNPs. It’s about listening to your body-and your ancestors.
And yeah-test if you can. But if you can’t? Know your story. That’s the first dose.