Pharmacogenomic Drug Response Estimator
How Your Genes Affect Medications
This tool estimates how your genetic variations might impact how your body processes medications. Based on your responses, you'll see how your metabolism speed could affect drug effectiveness and side effect risk.
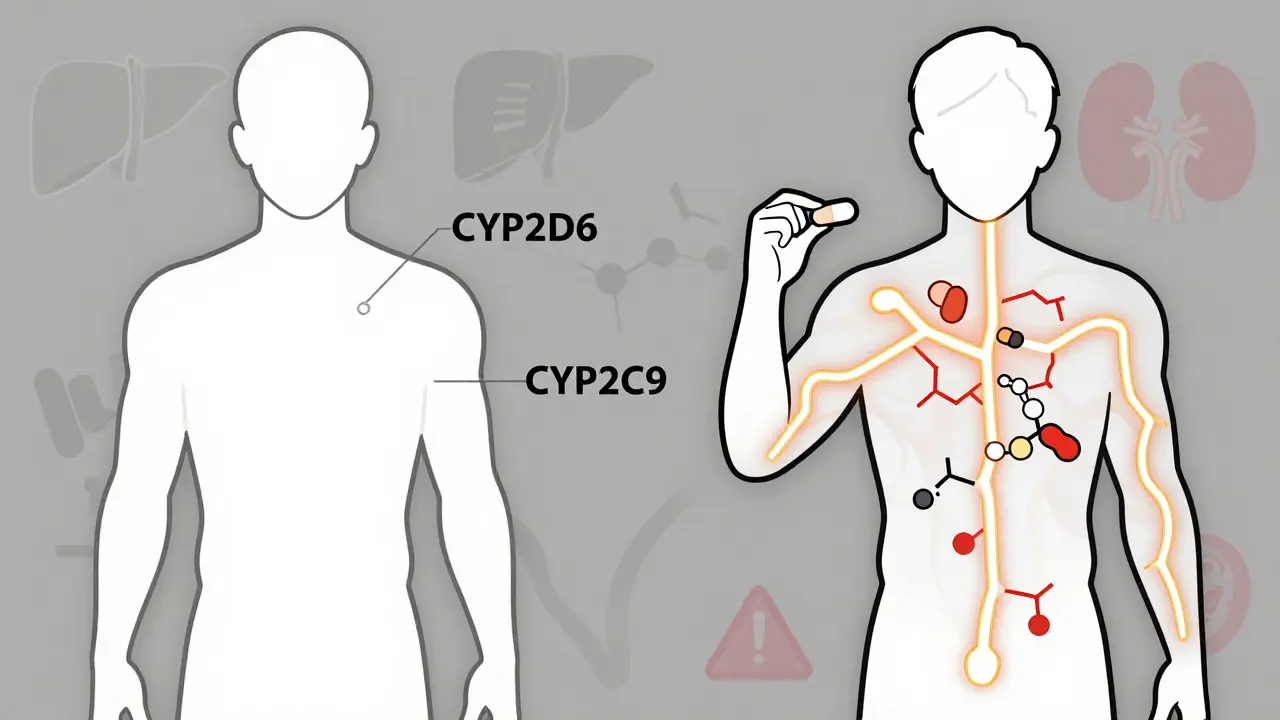
CYP2D6 (Codeine, Antidepressants)
CYP2C9 (Warfarin, NSAIDs)
CYP2C19 (Clopidogrel, Antidepressants)
Age Factor
Your Personalized Medication Profile
What This Means for You
Key Recommendations
Have you ever taken the same medication as someone else-same dose, same condition-and had a totally different experience? One person feels fine, another gets dizzy, nauseous, or worse? It’s not just bad luck. It’s biology. Medications don’t work the same way for everyone, and the reasons why are deeper than most people realize.
It’s Not Just About the Drug-It’s About You
When a doctor prescribes a pill, they’re not just giving you a chemical. They’re handing you a key that’s supposed to unlock a specific biological lock. But here’s the catch: everyone’s locks are slightly different. Some keys turn smoothly. Others jam. Some even break the lock. This isn’t theoretical. About 3.6% of people in Europe are hospitalized because of side effects from medications they were taking as directed. In the UK, adverse drug reactions cost the NHS over £770 million every year. And it’s not just expensive-it’s dangerous. Adverse drug reactions are among the top causes of death in the US, ranking fourth after heart disease, cancer, and stroke. The truth is, most side effects aren’t random. They’re predictable-if you know what to look for. And the biggest predictor? Your genes.Your Genes Control How Your Body Handles Drugs
Your DNA doesn’t just decide your eye color or height. It controls how fast your liver breaks down medications. That’s where the cytochrome P450 enzymes come in. These are the body’s main drug-processing machines. Three of them-CYP2D6, CYP2C9, and CYP2C19-handle about 80% of all commonly prescribed drugs. But here’s the problem: these enzymes vary wildly between people. Some people are poor metabolizers. Their bodies process drugs too slowly. A standard dose of a blood thinner like warfarin can build up to toxic levels. Others are ultra-rapid metabolizers. They burn through drugs so fast that the medication never even has a chance to work. For example, about 1-2% of Europeans and up to 29% of Ethiopians are ultra-rapid metabolizers of CYP2D6. That means a standard dose of codeine? It’s useless for pain relief in those people-and could even turn into dangerous levels of morphine. One study found that 15% of all adverse drug reactions are directly tied to these genetic differences. That’s not a small number. That’s millions of people every year getting sick from drugs meant to help them.Age, Weight, and Other Hidden Factors
Genes aren’t the whole story. Your body changes as you get older. Older adults have more body fat and less muscle. Fat-soluble drugs like certain antidepressants or sleep aids get stored in fat tissue and linger longer. That means even a normal dose can pile up over time and cause dizziness, confusion, or falls. Your liver and kidneys also slow down with age. That’s why older patients often need lower doses-even if they’re otherwise healthy. A 70-year-old might need half the dose of a 30-year-old for the same drug. Then there’s what you’re taking alongside your medication. A common painkiller like ibuprofen can cause stomach bleeding in 1-2% of people. But if you’re also on a steroid or have a certain gene variant, that risk jumps to 15-30%. Combine that with alcohol, or another drug like warfarin, and you’re playing Russian roulette with your digestive system. Even something as simple as a cold or the flu can change how your body handles drugs. Inflammation from an infection can shut down your liver’s drug-processing enzymes by 20-50%. That means a drug you’ve taken safely for years might suddenly become dangerous.Real Cases: When Genetics Save Lives
There’s a 68-year-old woman from Minnesota who kept having dangerous bleeding episodes on warfarin. Her INR levels kept spiking above 10-normal is 2-3. Doctors couldn’t figure it out. She wasn’t eating differently. She wasn’t drinking alcohol. She was following instructions perfectly. Then she got tested. Turns out, she had two copies of the CYP2C9*3 variant. She was a poor metabolizer. Her body couldn’t break down warfarin at all. Once her dose was cut by 60%, her INR stabilized. She stopped bleeding. She went from being a frequent hospital patient to living normally. In cancer treatment, the difference is even clearer. Kids with leukemia who get mercaptopurine often suffer severe toxicity. But when doctors test for a specific gene variant (TPMT), they can cut the dose before side effects start. At St. Jude Children’s Research Hospital, this simple test reduced severe side effects from 25% to just 12%. And it’s not just cancer. In asthma, about 15% of patients have a genetic variant that makes them respond dramatically better to leukotriene modifiers like zafirlukast. For them, these drugs cut symptoms by 45%. But for the other 85%? They get no benefit-and pay $250 to $300 a month for nothing.Why Isn’t Everyone Getting Tested?
If this is so clear, why aren’t all doctors ordering genetic tests before prescribing? The answer? It’s not because the science is weak. It’s because the system hasn’t caught up. The FDA has included pharmacogenomic info in the labels of over 300 drugs. For 44 of them, they even give specific dosing recommendations based on genes. But only 18% of US insurers cover genetic testing for drugs. Most doctors haven’t been trained to interpret the results. Only 32% of major hospitals have systems in place to alert them when a patient’s genes suggest a problem. A 2023 survey found that 68% of physicians feel unprepared to use genetic data. That’s not because they’re lazy. It’s because they were never taught how. Pharmacogenomics isn’t in most medical school curriculums. And interpreting a genetic report takes 15-20 hours of training-time most doctors don’t have. Plus, there’s the cost. Five years ago, a full pharmacogenomic panel cost $2,000. Today, it’s around $250. That’s a huge drop. But even at $250, many patients and providers still see it as optional-not essential.
The Future Is Already Here
The tide is turning. In January 2024, Medicare started covering pharmacogenomic testing for 17 high-risk medications. The FDA approved the first point-of-care CYP2C19 test in 2023-it gives results in 60 minutes. That means a cardiologist can test a patient for clopidogrel resistance right in the office and switch them to a better drug before they leave. In oncology, 65% of hospitals now use pharmacogenomics routinely. In psychiatry, it’s 42%. But in primary care? Only 18%. That’s where most prescriptions start-and where most side effects happen. The next big leap? Polygenic risk scores. Instead of looking at one gene, scientists are now combining hundreds of genetic markers to predict how someone will respond to a drug. Early studies show this approach is 40-60% more accurate than single-gene tests. The goal isn’t to eliminate all side effects. That’s impossible. But we can eliminate the ones that are preventable. The ones caused by a simple mismatch between a drug and a person’s biology.What You Can Do Today
You don’t need to wait for your doctor to order a test. If you’ve had unexpected side effects from a medication-especially if you’ve had them more than once-ask about pharmacogenomics. Keep a record: What drug? What side effect? When did it start? Did anyone else in your family have a bad reaction? That information is valuable. If you’re on multiple medications-especially if you’re over 65-talk to your pharmacist. Pharmacists spend 2-3 hours a week on pharmacogenomic cases. They’re often the best people to ask. And if you’re prescribed a drug with known genetic risks-like warfarin, clopidogrel, or certain antidepressants-ask: “Is there a genetic test that could help determine the right dose for me?” It’s not about being special. It’s about being smart. Your body isn’t broken. It’s just different. And now, we have the tools to match the medicine to the person-not the other way around.Why do some people have side effects from a drug while others don’t?
It’s mostly due to genetic differences that affect how the body absorbs, breaks down, and responds to drugs. Variations in enzymes like CYP2D6 and CYP2C9 can make someone a poor or ultra-rapid metabolizer, leading to either toxic buildup or no effect at all. Age, other medications, and even infections can also change how a drug behaves in the body.
Is genetic testing for drug reactions worth it?
For certain high-risk drugs like warfarin, clopidogrel, or some antidepressants, yes. Studies show genotype-guided dosing reduces hospitalizations by up to 31% and cuts emergency visits by 32%. If you’ve had bad reactions before or take multiple medications, testing can prevent serious harm and save money in the long run.
Can I get pharmacogenomic testing without a doctor’s order?
Some direct-to-consumer tests are available, but they’re not always clinically validated. The most reliable results come from tests ordered by a healthcare provider who can interpret them in context with your medical history. Insurance coverage is still limited, but Medicare now covers testing for 17 high-risk medications starting in 2024.
Which drugs have known genetic interactions?
The FDA lists 44 drugs with actionable genetic information, including warfarin (CYP2C9, VKORC1), clopidogrel (CYP2C19), codeine (CYP2D6), tamoxifen (CYP2D6), and certain antidepressants like SSRIs. These drugs have specific dosing guidelines based on genetic test results.
Are side effects more common in older adults?
Yes. Older adults are more likely to experience side effects because their liver and kidneys process drugs slower, they have more body fat (which stores certain drugs), and they often take five or more medications at once. This combination increases the risk of dangerous drug interactions and side effects by up to 300% compared to younger adults.
14 Comments
Jenny Salmingo
January 1 2026
My grandma took warfarin for years and never knew why she kept bleeding. Once they tested her genes, everything changed. She’s been fine for two years now. Just goes to show, it’s not magic-it’s science.
Everyone deserves to know what their body actually needs.
Paul Huppert
January 1 2026
Same. I had a bad reaction to an SSRI and thought I was just ‘fragile.’ Turns out I’m a poor CYP2D6 metabolizer. Took me three years to find out. Why isn’t this standard?
John Chapman
January 2 2026
This is 🔥 I’ve been telling my doctor for years that ‘one size fits all’ is garbage. Finally someone’s saying it right.
💯💯💯
Sara Stinnett
January 3 2026
Oh please. You’re telling me we should all get DNA tests before taking aspirin? This is what happens when you give people data without wisdom.
The real problem isn’t genetics-it’s the medical industrial complex selling you ‘personalized’ nonsense to make you pay more.
Let me guess-next they’ll test your DNA before you drink coffee.
Brandon Boyd
January 4 2026
Listen. I used to think this was all hype. Then my sister almost died on codeine after her wisdom teeth came out. Turned out she was an ultra-rapid metabolizer. The hospital didn’t even know to test her.
That’s not bad luck. That’s negligence.
Doctors need to stop pretending they know everything. We’re not lab rats-we’re people with unique biology.
If you’re on more than three meds or over 60, ask for the test. It’s not expensive anymore. It’s not experimental. It’s basic care.
Stop waiting for the system to catch up. Be the person who asks the question first.
And if your doctor rolls their eyes? Find a new one.
You’re not being ‘difficult.’ You’re being smart.
Frank SSS
January 5 2026
Yeah sure, genes matter. But let’s be real-most people just don’t follow directions. I’ve seen people take 4 pills at once, drink grapefruit juice, and wonder why they passed out.
Genetics? Maybe. But laziness? Definitely.
Also, why are we acting like this is new? My grandfather was on warfarin in the 70s and they adjusted his dose weekly based on blood tests. We used to do this without DNA.
Now we’re outsourcing common sense to a lab.
Branden Temew
January 5 2026
If we’re going to test everyone’s genes before prescribing, shouldn’t we also test their willpower, their sleep schedule, and their ability to read a label?
Or is this just another way to make medicine feel high-tech while ignoring the real issue: we treat people like data points, not humans?
Also, if your liver can’t handle a pill, maybe you shouldn’t be taking pills.
Just saying.
Robb Rice
January 7 2026
As someone who works in healthcare administration, I’ve seen the data. Pharmacogenomic testing reduces ER visits by 32%. That’s not just clinical-it’s financial. Hospitals save money. Patients live longer. Insurance companies should be screaming for this.
So why aren’t they? Because change is slow. Because paperwork is a nightmare. Because no one wants to retrain 800,000 doctors overnight.
But it’s coming. The tech is here. The evidence is solid. We’re just stuck in bureaucratic quicksand.
It’s not that we don’t know what to do. It’s that we’re too afraid to do it.
Deepika D
January 7 2026
Let me tell you something from India-we’ve been dealing with this for decades without fancy tests. My uncle took the same antidepressant as his cousin. One got dizzy, the other felt fine. They didn’t know why. But they didn’t panic. They adjusted. They watched. They talked to the pharmacist.
Genes are important, yes. But so is community. So is patience. So is listening to your body.
Western medicine loves to overcomplicate things. We don’t always need a lab to know something’s wrong. Sometimes we just need to slow down.
And yes, I’ve seen people die from side effects. But I’ve also seen people heal because someone sat with them for 45 minutes and asked, ‘How do you feel?’
Don’t forget the human part of medicine. The genes are just one piece.
Test if you can. But don’t stop being human if you can’t.
Retha Dungga
January 9 2026
So what you're saying is we're all different and that's why drugs don't work the same and we need tests and stuff
but like
what if you're just... not meant to take pills
maybe the real answer is less medicine
not more tests
just saying
🌿
Brady K.
January 11 2026
Oh wow. So now we’re going to run a full genomic panel before giving someone Tylenol? Brilliant. Let’s turn every pharmacy into a CRISPR lab.
Meanwhile, 70% of Americans can’t afford a $50 copay. But hey, let’s spend $250 on a gene test so we can avoid the side effects of a drug that’s been around since 1950.
Pharmacogenomics is cool. But let’s not pretend it’s a magic bullet while the system crumbles around us.
Fix the damn system first. Then we’ll talk about your CYP2C19 variant.
Urvi Patel
January 11 2026
Why are you wasting time with this genetic nonsense when the real issue is that Western medicine is built on profit not healing
Big Pharma doesn't want you to know your body can heal itself
they want you dependent on pills
and now they're selling you DNA tests to keep you hooked
it's all a scam
eat more turmeric
Martin Viau
January 13 2026
As a Canadian, I’m shocked this isn’t standard here. We’ve got universal healthcare-why aren’t we using it to prevent avoidable hospitalizations?
Our system is broken, sure. But this is the kind of thing that could actually make it better.
Stop treating patients like lab samples. Start treating them like people who have actual DNA.
Also, why are Americans still surprised by this? We’ve known about CYP enzymes since the 80s.
Kayla Kliphardt
January 14 2026
I had a reaction to metoprolol last year. My heart raced. I thought I was having anxiety. Turned out I was a poor CYP2D6 metabolizer. My doctor had never heard of it.
Now I’m on a different beta-blocker. No issues.
I wish I’d known sooner.
Thank you for writing this.