When you stand up too fast and feel like the room is spinning, it’s not just a momentary blur - it’s your balance system screaming for help. Vertigo isn’t just dizziness. It’s the terrifying sensation that you or the world around you is spinning, even when you’re perfectly still. For millions of people, especially those over 65, this isn’t rare. One in three older adults deals with some kind of balance problem, and vertigo is the most common reason they end up in a doctor’s office. Most of the time, the problem isn’t in the brain - it’s in the inner ear.
What’s Really Going On in Your Inner Ear?
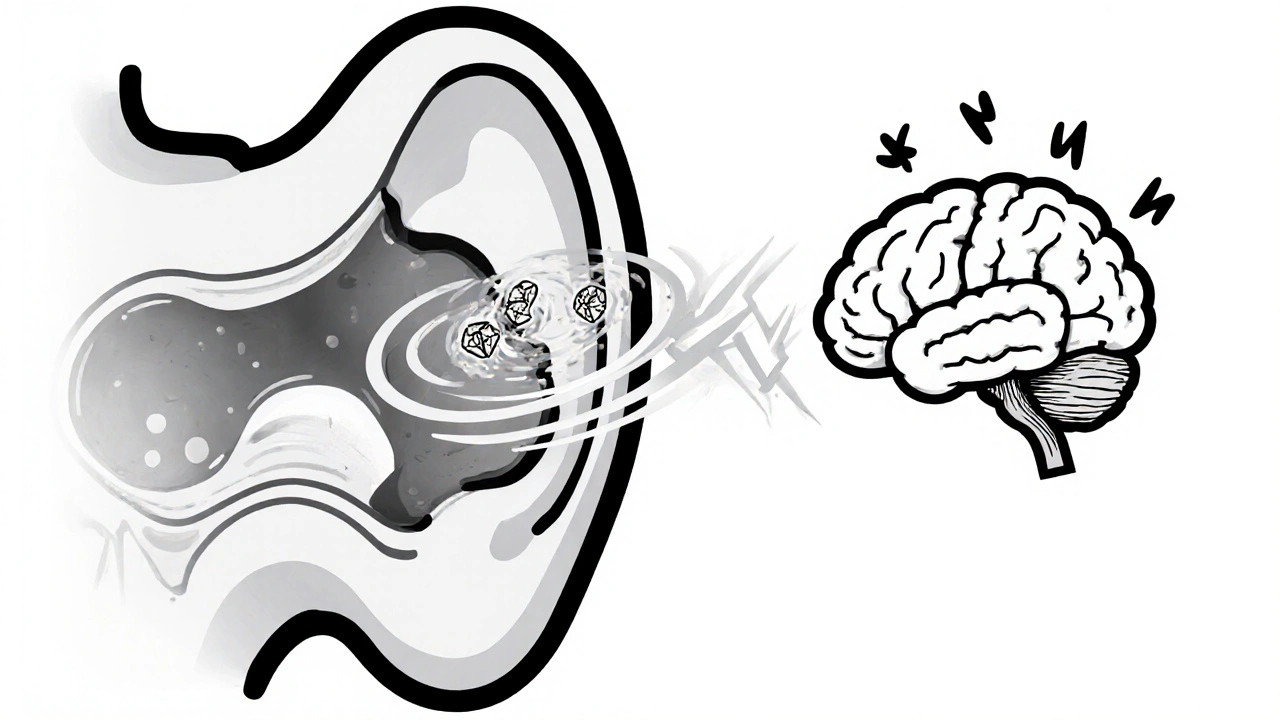
Your inner ear isn’t just for hearing. It’s your body’s built-in GPS for balance. Inside each ear, there are three fluid-filled loops called semicircular canals, and tiny calcium crystals - called otoconia - that sit on a gel-like membrane. When you move your head, these crystals shift, sending signals to your brain about which way you’re tilting. But sometimes, those crystals get loose. They drift into the wrong canal, usually the posterior one, and every time you roll over in bed or look up, they send false signals. That’s benign paroxysmal positional vertigo, or BPPV. It’s the #1 cause of vertigo, making up 20-30% of all dizziness cases - and half of all cases in people over 65. Other inner ear problems include vestibular neuritis, where a virus attacks the balance nerve, causing days of constant spinning without hearing loss. Then there’s Meniere’s disease - a chronic condition where fluid builds up in the inner ear, triggering vertigo that lasts for hours, along with ringing in the ear, muffled hearing, and that weird feeling of pressure. These aren’t just annoyances. They make you fall, avoid social situations, and lose confidence in your own body.How Do You Know It’s Not a Stroke?
Not every dizziness is harmless. About 20% of vertigo cases come from the brain - stroke, multiple sclerosis, or vestibular migraine. The scary part? Stroke can mimic BPPV. That’s why doctors use the HINTS exam: Head Impulse, Nystagmus, Test of Skew. Done within 48 hours of symptoms, it catches stroke with 96.8% accuracy - better than an MRI in the first few hours. If you have vertigo plus double vision, slurred speech, weakness on one side, or trouble walking straight, don’t wait. Go to the ER. Vestibular migraine is the most common brain-related cause. It doesn’t always come with a headache. You might just feel dizzy for hours after eating cheese, drinking wine, or sleeping poorly. It’s often misdiagnosed as anxiety or stress. But if you’ve had migraines before, and your dizziness comes with light sensitivity or nausea, it’s likely vestibular migraine.The Epley Maneuver: A 15-Minute Fix for BPPV
If you’ve been told you have BPPV, you’re in luck. There’s a simple, non-drug fix that works in most cases. The Epley maneuver is a series of slow head movements designed to guide those loose crystals back to where they belong. Done correctly, it clears up vertigo in 80-90% of people after one or two sessions. The Cleveland Clinic reports 95% success within two weeks. You can do it at home - but only after a doctor confirms it’s BPPV. Do it wrong, and you might make it worse. The key steps: sit on the edge of your bed, turn your head 45 degrees toward the affected ear, lie back quickly with your head hanging slightly off the bed, wait 30 seconds, turn your head 90 degrees to the opposite side, wait again, then roll onto your side and sit up. Each position needs to be held for at least 30 seconds. Many people feel dizzy during the maneuver - that’s normal. It means it’s working. Doctors often give patients a video or printed guide. Some even use smartphone apps now that track head position with the phone’s sensor. These apps are about 85% accurate at spotting the right kind of nystagmus (eye jerking) that confirms BPPV.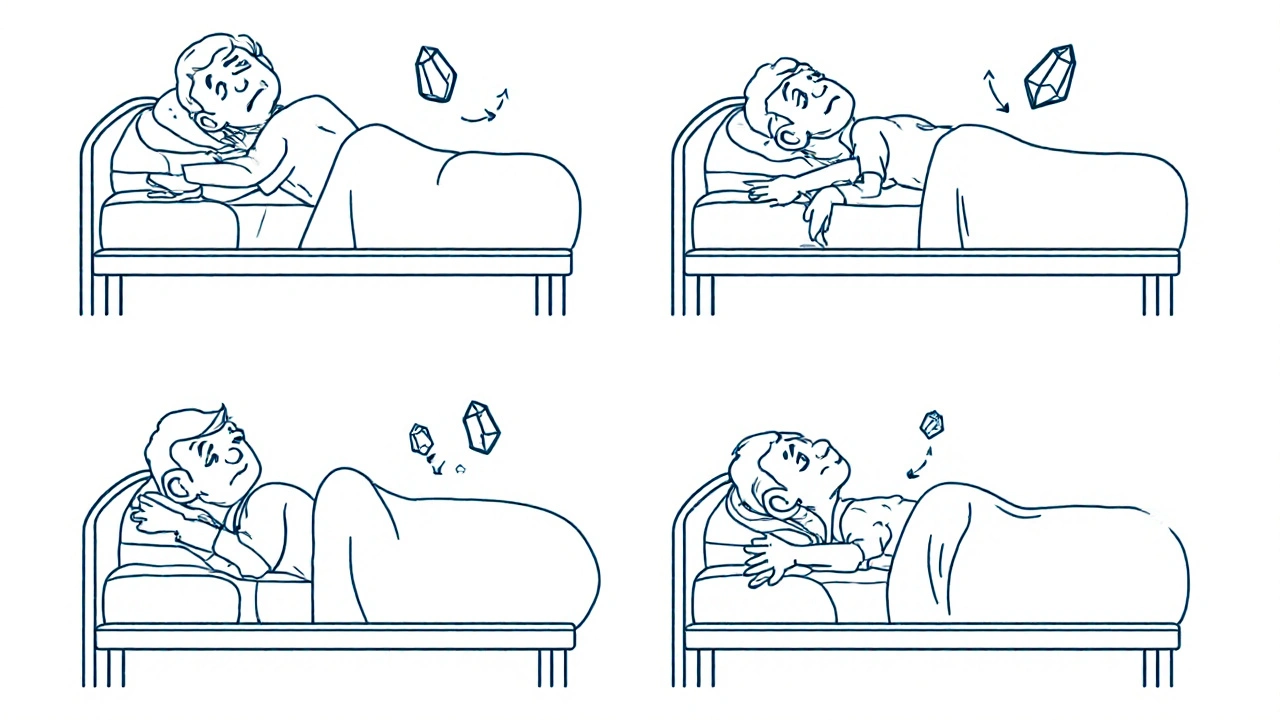
Vestibular Therapy: Training Your Brain to Rebalance
If your vertigo won’t go away with the Epley maneuver - or if it’s from vestibular neuritis, Meniere’s, or vestibular migraine - then vestibular rehabilitation therapy (VRT) is your next step. It’s not massage or stretching. It’s physical therapy for your balance system. VRT uses three types of exercises:- Gaze stabilization: You focus on a stationary object while moving your head side to side or up and down. This retrains your eyes and inner ear to work together.
- Balance retraining: Standing on one foot, walking heel-to-toe, or standing on foam - all while keeping your balance. These rebuild your body’s confidence in movement.
- Habituation: Repeatedly doing movements that trigger dizziness - like turning your head quickly - until your brain learns to ignore the false signals.
Medications: Short-Term Relief, Long-Term Risk
Doctors often reach for meclizine (Antivert) or promethazine when vertigo hits. These drugs calm the inner ear signals and reduce nausea. They work - about 70% of people feel better in a few hours. But they don’t fix the cause. And using them for more than 72 hours? That’s dangerous. Your brain needs to adapt. It’s called vestibular compensation. The longer you suppress the signals with pills, the slower your brain learns to compensate. Studies show prolonged use can delay recovery by 30-50%. That means you stay dizzy longer. Many patients report feeling foggy, drowsy, or too tired to work. One Reddit user wrote: “Meclizine made me too sleepy to drive. The exercises took three weeks, but I finally got my life back.” For Meniere’s disease, doctors prescribe water pills (like triamterene-hydrochlorothiazide) and a strict low-sodium diet - under 2,000mg a day. That’s harder than it sounds. Most packaged food has more sodium than you think. A single slice of bread can have 200mg. You need to cook from scratch, avoid canned soups, and skip the deli meats. For vestibular migraine, preventive meds like propranolol or topiramate are used. These reduce vertigo frequency by half in about 60% of patients. But again, they’re not a cure. They’re a tool to buy time while your brain heals.
What You Can Do Right Now
If you’re dizzy right now, here’s what to do:- Don’t panic. Sit or lie down. Close your eyes. Breathe slowly.
- Write down what happened: Did it start when you turned your head? Did you feel ringing or fullness in your ear? How long did it last?
- See a doctor who specializes in balance - an ENT or vestibular therapist. Ask: “Could this be BPPV?” and “Have you done the Dix-Hallpike test?”
- If you’re diagnosed with BPPV, ask for the Epley maneuver. Don’t wait. It’s fast, free, and works.
- If it’s not BPPV, ask for vestibular rehab. Find a physical therapist trained in vestibular therapy. Most hospitals and clinics have them.
- Stop taking dizziness pills after 3 days. Let your brain heal.
What’s Next for Vertigo Treatment?
The future is getting smarter. Researchers are testing drugs that might stop calcium crystals from breaking loose in the first place. One experimental drug, CPP-115, cut BPPV recurrence by 40% in early trials. Gene therapy for Meniere’s is being tested in animals - and so far, it’s reduced symptoms by 70%. Telehealth is changing access too. People in rural areas can now do video-guided Epley maneuvers with a specialist watching through their phone camera. Success rates are 75% - almost as good as in-person visits. And insurance? Medicare covers 80% of vestibular rehab. Private insurers usually cover 70%, but often limit you to 10-20 sessions. If you’re struggling to afford therapy, ask your clinic about sliding-scale fees. Many have payment plans.Real Stories, Real Results
A 72-year-old woman in Bristol spent three months going to different doctors. They all said it was anxiety. Then she saw a vestibular therapist who did the Dix-Hallpike test. BPPV. One Epley maneuver. She was symptom-free in 15 minutes. “I cried,” she said. “I hadn’t slept on my side in years.” Another man with Meniere’s cut his vertigo attacks from daily to once a month by switching to a low-sodium diet, doing daily balance exercises, and taking a water pill. “I stopped being afraid to go out,” he told his therapist. “Now I walk the dog every morning.” The common thread? They didn’t just wait for pills to work. They took action. They moved. They changed their habits. And their brains responded.Is vertigo the same as dizziness?
No. Dizziness is a general term that includes lightheadedness, unsteadiness, or feeling faint. Vertigo is a specific type of dizziness where you feel like you or your surroundings are spinning. It’s caused by a mismatch in signals from your inner ear, eyes, or brain.
Can BPPV come back after treatment?
Yes. About 30-50% of people have a recurrence within five years. That’s why doctors recommend doing the Epley maneuver again if symptoms return. Some people learn to do it themselves at home. There’s no permanent cure, but each episode is treatable.
How long does vestibular therapy take to work?
Most people start feeling better in 2-4 weeks, with major improvement by 6-8 weeks. But you need to do the exercises twice a day. Skipping days slows progress. The first week is often the hardest - symptoms might get worse before they get better.
Are there any home remedies for vertigo?
The only proven home remedy is the Epley maneuver for BPPV. Other things like ginger tea or essential oils may help with nausea, but they won’t fix the root cause. Avoid the “head spin” trick - it can make BPPV worse. Stick to evidence-based methods.
Can stress cause vertigo?
Stress doesn’t cause BPPV or Meniere’s, but it can trigger vestibular migraine and make existing vertigo feel worse. High stress raises cortisol, which affects fluid balance in the inner ear. Managing stress with sleep, breathing, or therapy can reduce attack frequency.
When should I see a doctor for dizziness?
See a doctor if your dizziness lasts more than a few days, comes with hearing loss, ringing in the ear, double vision, weakness, or trouble walking. If you’re over 60 and have sudden vertigo, don’t wait - get checked for stroke. Even if you think it’s just stress, a simple test can rule out BPPV or other treatable causes.
15 Comments
amit kuamr
December 2 2025
The Epley maneuver works if you do it right but most people mess it up by rushing the positions. I’ve seen patients spin for hours because they didn’t wait 30 seconds. Patience is the real treatment.
Also stop using meclizine like candy. It’s not a fix it’s a crutch.
Scotia Corley
December 2 2025
While I appreciate the clinical overview, I must emphasize that the overreliance on vestibular therapy as a panacea ignores the systemic neglect of neurological diagnostics in primary care. The HINTS exam should be standard in ER protocols, not an afterthought reserved for specialists. The fact that it’s not reflects a deeper institutional failure in vestibular medicine.
Karandeep Singh
December 2 2025
bro the erpley thing is a scam i did it and got worse then i just laid down and it went away in 2 days
elizabeth muzichuk
December 3 2025
Let me tell you something. I had vertigo for 11 months. Doctors called it anxiety. I was told to take Xanax. I didn’t. I found a therapist who did the Dix-Hallpike test on day one. BPPV. One maneuver. I cried. I haven’t slept on my side in 8 years. Now I do. And I’m not afraid to tell you: if you’re still on meds after 72 hours, you’re letting your brain rot. Stop being passive. Move. Your body isn’t broken. It’s just forgotten how to listen.
Debbie Naquin
December 3 2025
The neuroplastic reweighting of vestibulo-ocular and somatosensory integration pathways underpins VRT efficacy. The habituation protocols induce synaptic pruning of maladaptive vestibular reflexes, effectively recalibrating the central compensation threshold. The 70-80% improvement rate is statistically significant but only when adherence exceeds 85% of prescribed sessions. Noncompliance correlates strongly with prolonged cortical inhibition of vestibular nuclei activity. In lay terms: you have to do the exercises even when you feel like dying. That’s the price of neural adaptation.
Mary Ngo
December 3 2025
Who funded this article? The vestibular therapy industry? The pharmaceutical companies pushing low-sodium diets? The device makers selling $200 phone apps that claim to detect nystagmus? I’ve seen this before - the same people who sold us low-fat diets are now selling us balance exercises. The inner ear doesn’t need rehab. It needs less sodium, less stress, and less corporate manipulation disguised as science.
James Allen
December 5 2025
Look, I get it. You want to fix vertigo with yoga and head turns. But let’s be real - if you’re over 65 and dizzy, it’s not BPPV. It’s your body saying you’ve been sitting too long. Go outside. Walk. Lift something. Stop watching videos. America’s biggest problem isn’t loose crystals - it’s laziness. We medicate instead of moving. We Google instead of getting up. Do you think your great-grandpa took meclizine? No. He walked to the store. And he didn’t fall. Because he didn’t sit on his butt all day.
Kenny Leow
December 6 2025
Good post. I’m from Singapore and we’ve got a growing elderly population with vertigo issues. Here, VRT is covered under Medisave - so access isn’t the problem. The problem is stigma. Older folks think dizziness = old age. They don’t ask for tests. They just stop leaving the house. We need more community outreach. Maybe even temple-based balance workshops. 🙏
Kelly Essenpreis
December 7 2025
So you're telling me I have to do head spins and eat no salt and do exercises for weeks just so I can stop feeling like I'm on a boat? I don't have time for this. I work two jobs. My insurance won't cover it. And the doctor didn't even do the test. He just handed me a prescription. You're not helping. You're just making me feel guilty.
Alexander Williams
December 9 2025
The 95% success rate cited for the Epley maneuver is based on selection bias. Studies exclude patients with comorbid vestibular neuritis, migraines, or cervical spine pathology. In real-world clinics, recurrence rates are closer to 40-60% within 12 months. The literature omits this. Why? Because it undermines the narrative of a simple fix. The truth is messy. The inner ear is not a plumbing system. It’s a dynamic neural interface. You can’t flush it.
Charlotte Collins
December 10 2025
Let me be brutally honest - if you’re still dizzy after the Epley maneuver, you’re not doing the exercises right. Or worse - you’re doing them when you’re exhausted, dehydrated, or stressed. Your vestibular system isn’t broken. It’s overwhelmed. You’re running on fumes. Sleep. Hydrate. Cut out caffeine. Stop scrolling at 2am. No app, no maneuver, no pill will fix that. Your brain needs rest. Not more stimulation.
Margaret Stearns
December 12 2025
i had this last year. did the epley at home. it worked. but i kept doing the balance stuff even after i felt better. now i dont get dizzy at all. my dog loves it when i do the heel-to-toe walk in the kitchen. he thinks im dancing.
Rachel Stanton
December 14 2025
For anyone reading this and feeling overwhelmed - you’re not alone. I’m a vestibular therapist. I’ve seen people quit after one week because their dizziness spiked. That’s normal. That’s your brain rewiring. I tell my patients: ‘It’s not getting worse - it’s getting ready to get better.’ Do the exercises. Write down your progress. Celebrate small wins. One day you’ll realize you walked to the mailbox without holding the railing. That’s your victory. You’ve got this.
Bonnie Youn
December 16 2025
DO THE EPLEY. DO THE EXERCISES. STOP TAKING PILLS. YOU CAN DO THIS. I DID. MY MOM DID. MY NEIGHBOR DID. IT WORKS. YOUR BRAIN IS SMARTER THAN YOU THINK. JUST MOVE. JUST TRY. JUST START TODAY. NO EXCUSES. I BELIEVE IN YOU.
Suzanne Mollaneda Padin
December 16 2025
I’m a physical therapist in rural Maine. We don’t have a vestibular specialist within 90 miles. So I started doing video-guided Epley maneuvers over Zoom. Patients record themselves. I watch the eye movements. We adjust. Success rate’s 72%. It’s not perfect - but it’s better than nothing. If you’re in a remote area, reach out. I’ll help. No charge. We’re all in this together.