Medication Interaction Checker
How to Use This Tool
Enter your medications, supplements, and common items you consume. This tool highlights potential interactions based on common examples from the article. Always consult your pharmacist for personalized advice.
Your Results
Every year, over a million people in the U.S. get hurt because of medication errors. A big chunk of those cases-nearly 7%-come from unexpected medication interactions. These aren’t just rare accidents. They happen when something you take-whether it’s a prescription, an over-the-counter pill, a supplement, or even your morning grapefruit juice-changes how another medicine works in your body. Sometimes it makes the drug weaker. Sometimes it makes it stronger. And sometimes, it can cause serious harm.
Most people assume their doctor knows everything about their meds. But here’s the truth: your pharmacist knows more about how drugs interact than almost anyone else. They’re trained to spot hidden dangers between your heart pill and your allergy medicine, your blood thinner and your vitamin D, your antidepressant and your evening glass of wine. Yet, only about 38% of patients get a full conversation about these risks when they pick up their prescription.
You don’t have to wait for your pharmacist to bring it up. You need to ask. Here’s exactly what to say-and why it matters.
Does this medicine interact with anything else I’m taking?
This is the most basic, most important question. Don’t just list your prescriptions. Include everything: ibuprofen, melatonin, fish oil, turmeric, iron pills, even that herbal tea you drink every night. Many people don’t think of supplements as “medicines,” but they absolutely can cause dangerous interactions.
For example, warfarin (a blood thinner) can become dangerously strong if you start taking vitamin K supplements or even eat a lot of leafy greens. On the flip side, if you suddenly cut back on those greens, your blood can clot too easily. It’s not about avoiding food-it’s about keeping your intake steady and letting your pharmacist know what you’re doing.
Another common issue: levothyroxine (for thyroid issues) and calcium supplements. If you take them together, your body absorbs up to half less of the thyroid med. The fix? Space them out by at least four hours. Your pharmacist can give you a simple schedule.
Are there foods or drinks I should avoid?
It’s not just about pills. What you eat and drink can change how your meds work.
Grapefruit juice is the classic example. It blocks an enzyme in your gut that breaks down certain drugs. That means more of the drug enters your bloodstream-sometimes way more. For statins like atorvastatin, grapefruit juice can spike levels by up to 1,500%. That raises your risk of muscle damage and kidney failure. Even one glass a day can be risky.
Antacids like Tums might seem harmless, but they can interfere with Hepatitis C treatments and some antibiotics. Dairy products can reduce the absorption of certain antibiotics like ciprofloxacin. Alcohol doesn’t just make you sleepy-it can cause dangerous reactions with metronidazole (a common antibiotic), lead to liver damage with acetaminophen, or make your blood pressure drop too low with blood pressure meds.
Ask specifically: “Is there anything I should stop eating, drinking, or drinking too much of while on this?” Don’t assume your pharmacist will guess your habits.
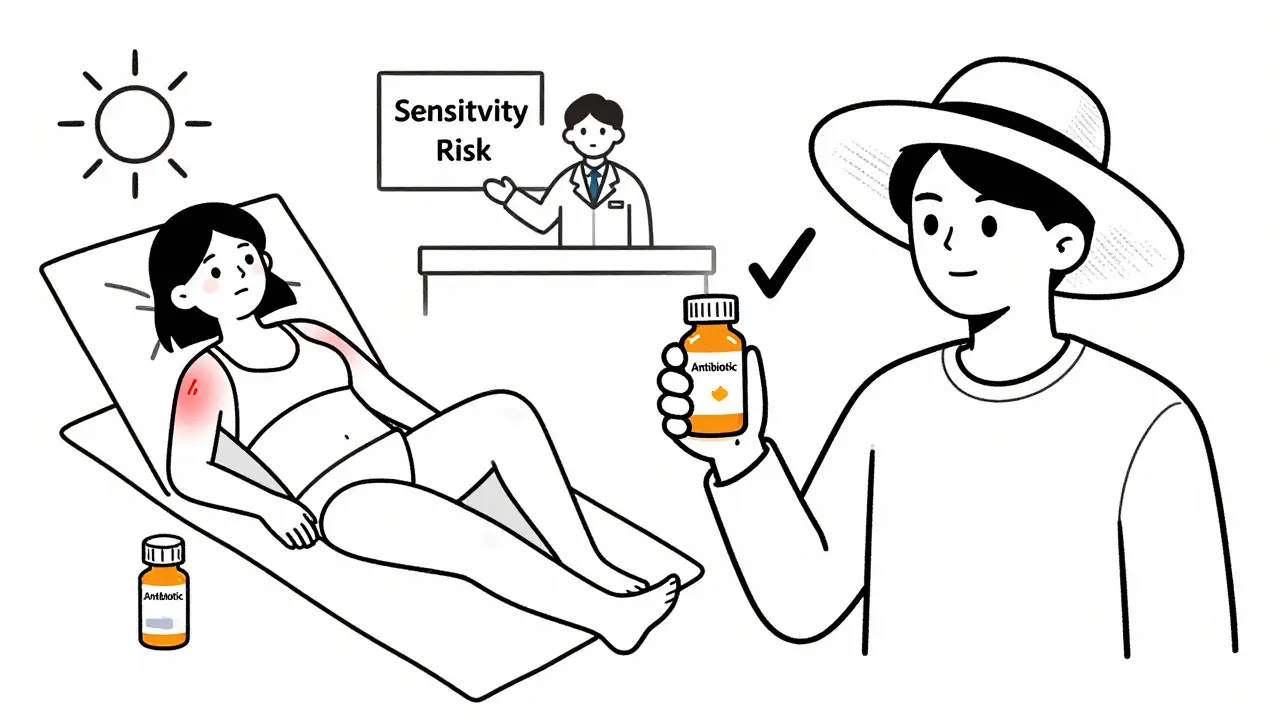
Can this medicine make me more sensitive to sunlight?
This one catches people off guard. Some medications-like certain antibiotics, diuretics, acne treatments, and even some antidepressants-can make your skin react badly to the sun. You might get a bad sunburn after just 10 minutes outside, or your skin could darken unevenly.
It’s not just about sunscreen. You might need to avoid midday sun entirely, wear long sleeves, or even skip tanning beds. If you’re planning a beach trip or outdoor activity, ask this question ahead of time. It’s a simple one, but it can prevent a painful, long-lasting reaction.
What signs should I watch for if there’s a bad interaction?
Not all interactions cause obvious symptoms right away. Some build up slowly. Others hit fast and hard.
With SSRIs (like sertraline) and certain migraine meds (like triptans), you could develop serotonin syndrome-a rare but life-threatening condition. Signs include confusion, rapid heartbeat, high fever, muscle stiffness, and tremors. If you start feeling “off” after adding a new med, don’t wait. Call your pharmacist or doctor.
With blood thinners, watch for unusual bruising, nosebleeds, or blood in your urine or stool. With statins, unexplained muscle pain or weakness could signal damage. Your pharmacist can tell you which symptoms are red flags for your specific meds.
They’ll also tell you what to do if you notice them: stop the medicine? Call 911? Wait and monitor? Don’t guess. Get the plan in advance.
Will I need blood tests or other monitoring?
Some medications require regular checks to stay safe. Warfarin needs frequent INR blood tests. Lithium requires kidney and thyroid checks. Some diabetes drugs need liver function monitoring. If you’re starting a new drug that’s known to interact with others, your pharmacist should tell you if monitoring is needed.
Even if your doctor ordered tests, ask: “Will my pharmacist be looking at these results too?” Many pharmacies now track lab values and will call you if something looks off-before you feel sick.
What if I forget to take my pill? Will that cause an interaction?
Skipping a dose isn’t just about missing the benefit-it can trigger problems. For example, if you take a blood pressure med once a day and miss it, your pressure might spike. Then you take two pills the next day to “catch up.” That double dose could interact dangerously with your other meds.
With antibiotics, missing doses can lead to resistance. With mood stabilizers, skipping doses can trigger mood swings or seizures.
Your pharmacist can help you create a fail-safe plan: “If I miss a dose, should I take it later? Skip it? Double up?” Don’t wing it. Get the rule before you forget.
Do any of my other meds affect how this one works?
It’s not just about the new drug. Your existing meds might be changing how the new one behaves.
For example, if you’re on a strong painkiller like oxycodone and your doctor adds a new antidepressant, that antidepressant might slow down how your body breaks down the painkiller. Result? You get too much of it. You could overdose-even if you’re taking the same dose you always have.
Or, if you’re on a birth control pill and your doctor prescribes an antibiotic like rifampin, the pill might stop working. That’s not rare-it’s well-documented. Your pharmacist should flag that. But they won’t know unless you tell them what you’re already taking.
How do I keep track of all this?
Write it down. Every time you get a new prescription, supplement, or OTC med, add it to a list. Include the name, dose, how often you take it, and why. Keep it in your phone, wallet, or on your fridge.
Update it every three months. Even if nothing changed, review it. You might forget you started taking a new vitamin. Or you might have stopped a med and forgotten to tell your pharmacist.
Bring this list to every appointment-with your doctor, your pharmacist, even the ER. It’s your safety net. And if you’re using a pharmacy app like CVS or Walgreens, check their “interaction checker” tool-but don’t rely on it alone. Apps miss about a third of serious interactions. A human pharmacist won’t.
What if I can’t afford my meds?
Switching to a cheaper generic or changing brands can sometimes change how a drug interacts. A generic version might have different fillers or release rates. Your pharmacist can help you pick one that’s safe and affordable.
They also know about copay cards, patient assistance programs, and mail-order options that can cut your costs without risking safety. Don’t skip a med because it’s expensive. Ask your pharmacist for help. They’ve got options you won’t find online.
Medication interactions aren’t something you should fear. They’re something you should understand. Your pharmacist isn’t just filling your prescription-they’re your last line of defense against a hidden danger. But they can’t help if you don’t ask.
Next time you pick up your meds, take two minutes. Ask the questions. Write down the answers. It could save your life.
Can over-the-counter meds interact with prescription drugs?
Yes, absolutely. Common OTC drugs like ibuprofen, antacids, and cold medicines can interact with prescriptions. For example, ibuprofen can increase bleeding risk when taken with blood thinners like warfarin. Antacids can block absorption of thyroid meds and some antibiotics. Always check with your pharmacist before taking any new OTC product-even if it’s labeled “natural” or “safe.”
Do herbal supplements cause interactions?
Yes, and they’re often overlooked. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and even some cancer drugs. Garlic and ginkgo can thin the blood and increase bleeding risk during surgery. Ginseng can interfere with blood sugar control and blood pressure meds. Herbal products aren’t regulated like prescription drugs, so their strength and ingredients can vary. Always tell your pharmacist exactly what supplements you’re taking.
Why doesn’t my doctor tell me about interactions?
Doctors focus on diagnosing and treating your condition. They often don’t have time to review every single medication you take, especially if you see multiple specialists. Pharmacists, however, are trained specifically to review your full list of meds and spot interactions. They’re the experts in drug chemistry and how substances behave in the body. Your doctor prescribes; your pharmacist verifies safety.
Can alcohol interact with my medications?
Yes. Alcohol can increase drowsiness with sedatives, anxiety meds, and painkillers. It can damage your liver when mixed with acetaminophen. With metronidazole, it causes severe nausea, vomiting, and rapid heartbeat. Even with blood pressure meds, alcohol can cause dangerous drops in blood pressure. If you drink regularly, tell your pharmacist. They can tell you if it’s safe to have even one drink.
What if I get a new prescription from a different doctor?
Always bring your full medication list to every appointment. Even if you use the same pharmacy, a new doctor might not have access to your full history. Ask your pharmacist to review your entire list whenever you get a new prescription. Many pharmacies will flag potential interactions automatically-but only if they have your complete profile. Don’t assume someone else is keeping track.
Are there apps or tools that can check for interactions?
Yes, apps from CVS, Walgreens, and others let you enter your meds and check for interactions. But they’re not perfect. Studies show they miss up to 37% of clinically significant interactions. They’re helpful for a quick check, but never a replacement for talking to your pharmacist. Human experts catch subtle, complex interactions that software can’t-like how timing, dosage, or your liver function changes the risk.
Can my pharmacist help if I have multiple doctors?
Absolutely. Pharmacists are trained to coordinate care across providers. If you see a cardiologist, a rheumatologist, and a pain specialist, each might prescribe something without knowing what the others ordered. Your pharmacist can review all prescriptions together, spot conflicts, and even contact your doctors to suggest safer alternatives. They’re the only healthcare professional whose job is to see the full picture.
What if I’m pregnant or breastfeeding?
Many medications are unsafe during pregnancy or breastfeeding, and some interactions become more dangerous. For example, certain antibiotics, blood pressure meds, and even some OTC sleep aids can pass into breast milk or affect fetal development. Your pharmacist can help you find safe alternatives and tell you if a medication is safe to use while nursing. Never assume something is safe just because it’s “over-the-counter.” Always ask.
If you’re taking more than one medication, you’re at risk. But you’re not powerless. The right questions turn fear into control. Your pharmacist has the answers. You just have to ask.

8 Comments
jonathan soba
January 28 2026
Let’s be real - most pharmacists are overworked and underpaid. They’ll give you the bare minimum if you don’t push. I once asked about grapefruit and my statin, and the guy just nodded like I was asking if the store had toilet paper. Didn’t even blink. You gotta grill them. Like, ‘So, if I drink one glass of OJ with pulp, am I signing up for an ER visit?’ Make them sweat. It’s your life.
Chris Urdilas
January 29 2026
My pharmacist once handed me a pill bottle and said, ‘Take one daily.’ I asked if it played nice with my turmeric and CBD oil. He paused. Looked at me like I’d asked if the sun was made of cheese. Then he pulled up his computer, typed it in, and said, ‘Yeah, you’re fine… but maybe skip the CBD before yoga.’ I didn’t even know he knew what CBD was. Point is - ask. Even the weird stuff. They’ve seen it all.
Phil Davis
January 31 2026
My doctor prescribed me a new antidepressant. I forgot to mention I was taking St. John’s Wort because I thought it was ‘just a herb.’ Turns out, it’s like pouring gasoline on a candle. I ended up in the ER with serotonin syndrome. Not funny. Not a joke. I’m alive because my pharmacist caught it when I went back for a refill. He didn’t yell. He just said, ‘You know that stuff you think is harmless? It’s not.’ I now keep a laminated list taped to my fridge. It’s my survival guide.
Irebami Soyinka
February 1 2026
Y’all in the West think you can just pop pills like candy and then blame the system when your liver gives up. 😒 In Nigeria, we don’t have fancy apps or pharmacists with 12 degrees. We use ginger, garlic, and prayer - and we don’t mix them with ‘Western poison’ unless we’re ready to die. 🙏 If you’re taking warfarin and drinking palm wine? You’re not brave - you’re just stupid. Ask your pharmacist? Nah. Ask your ancestors first. They knew what was safe before your ‘science’ was even born.
Mel MJPS
February 1 2026
I’m 72 and on 8 different meds. I used to be too embarrassed to ask questions - thought I’d sound dumb. Then my pharmacist, Linda, sat me down with a cup of tea and said, ‘Honey, if you don’t ask, I can’t help.’ Now I write everything down. Even the gummy vitamins. She even called my cardiologist when my BP meds clashed with my thyroid pills. She’s not just filling prescriptions - she’s keeping me alive. Don’t be shy. Your pharmacist is your secret weapon.
Katie Mccreary
February 2 2026
My mom took OTC sleep aids with her blood pressure med. Ended up in a coma for 3 days. She didn’t think it mattered because it was ‘natural.’ Spoiler: natural doesn’t mean safe. Pharmacist? She never asked. Now I carry a laminated list in my purse. If you’re not asking, you’re gambling. And the house always wins.
SRI GUNTORO
February 3 2026
People these days take supplements like they’re candy. You think turmeric is harmless? It’s a blood thinner. You think garlic is just flavor? It’s a drug. And you’re not a scientist - you’re just a guy who read a blog. If you’re not telling your pharmacist everything, you’re not just irresponsible - you’re dangerous. Your life isn’t a TikTok trend. Stop being lazy.
Rose Palmer
February 3 2026
Thank you for this comprehensive and clinically vital guide. As a healthcare professional with over two decades of experience in patient safety protocols, I can confirm that the statistics cited are not only accurate but conservative. Pharmacists are the final, critical checkpoint in the medication chain. Their training in pharmacokinetics, pharmacodynamics, and polypharmacy risk assessment is unparalleled. I routinely recommend patients bring a complete, updated medication list - including dosage, frequency, and indication - to every pharmacy visit. This practice reduces adverse drug events by up to 42%. Your emphasis on proactive inquiry is not merely advisable - it is a standard of care. Please share this with everyone you know.