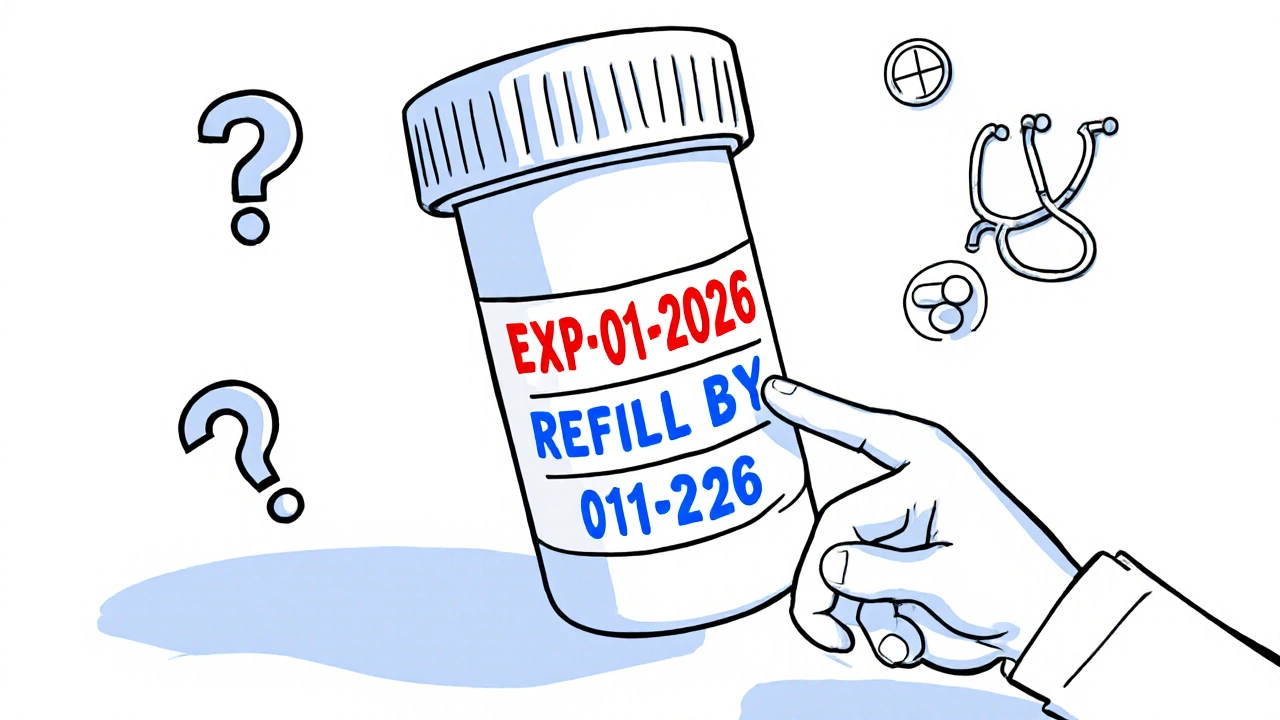
Learn the critical difference between refill-by and expiration dates on prescription labels to avoid dangerous mistakes, unnecessary costs, and treatment gaps. Know when your medicine is still safe-and when you need a new prescription.
Refill-by Date: What It Means and How to Manage Your Medication Schedule
When you see a refill-by date, the date by which you should get your next prescription filled to avoid gaps in treatment. Also known as fill-by date, it's not just a pharmacy note—it's a critical part of your medication safety plan. This date tells you when to act before your supply runs out, but it’s not the same as the expiration date. Many people confuse the two, and that’s where problems start. A pill might still be safe to take after the refill-by date, but if you don’t refill on time, you risk stopping your treatment—especially for conditions like high blood pressure, diabetes, or depression where consistency saves lives.
The prescription refill, the process of obtaining a new supply of medication after the current one is used up is tied to your doctor’s instructions and your pharmacy’s system. Some refills are automatic; others require a call or online request. But even if your pharmacy sends a reminder, it’s your job to check the refill-by date on the label. Why? Because if you wait too long, your doctor might have to reauthorize the script, causing delays. And if you refill too early, you might end up with duplicate doses or expired meds piling up. This is where pharmacy tracking, systems used by pharmacies to monitor medication usage and refill patterns for patient safety comes in. Modern systems flag when you’re due, but they can’t know if you’re out of town, forgot to pick it up, or ran out early because you took more than prescribed.
Think about drug expiration, the date after which a medication is no longer guaranteed to be safe or effective. Your refill-by date often comes weeks before the expiration date on the bottle. That’s intentional. It gives you buffer time to refill without risking expired pills. But heat, humidity, and poor storage—like keeping meds in the bathroom—can make them degrade faster. That’s why medication expiration and drug storage are part of this whole picture. You can have the perfect refill schedule, but if your pills are ruined by moisture, the date doesn’t matter.
People managing chronic conditions—like diabetes, asthma, or heart disease—live by these dates. One missed refill can mean a hospital visit. That’s why tools like visual dosing aids, tools like labeled syringes and measuring cups that help patients take the right amount and digital prescription labels, QR codes on medication bottles that link to up-to-date usage info are so helpful. They don’t replace the refill-by date, but they make following it easier. If you’re on multiple meds, a personal medication list, a written or digital record of all drugs, supplements, and allergies you take should include refill-by dates too. Write them down. Set phone alerts. Use pill organizers with date markers.
And don’t forget: if your refill-by date keeps coming up too soon, talk to your doctor. Maybe you need a larger supply, a different dosage, or a mail-order option. Some insurers limit how often you can refill, even if you need it. Patient assistance programs can help with cost, but they won’t fix a timing problem. The goal isn’t just to get your pills—it’s to get them at the right time, safely, every time. Below, you’ll find real stories and guides from people who’ve been there: how to avoid running out, how to handle insurance roadblocks, how to spot when a refill isn’t working for your life. These aren’t theory pieces—they’re fixes that worked.