Every time you pick up your prescription, you’re paying the same copay-whether you get 30 days of medication or 90. That’s the secret most people don’t know. If you’re taking the same medicine every month for high blood pressure, diabetes, or cholesterol, you could be saving hundreds a year without changing anything except how you fill your script.
Why 90-Day Fills Save You Money
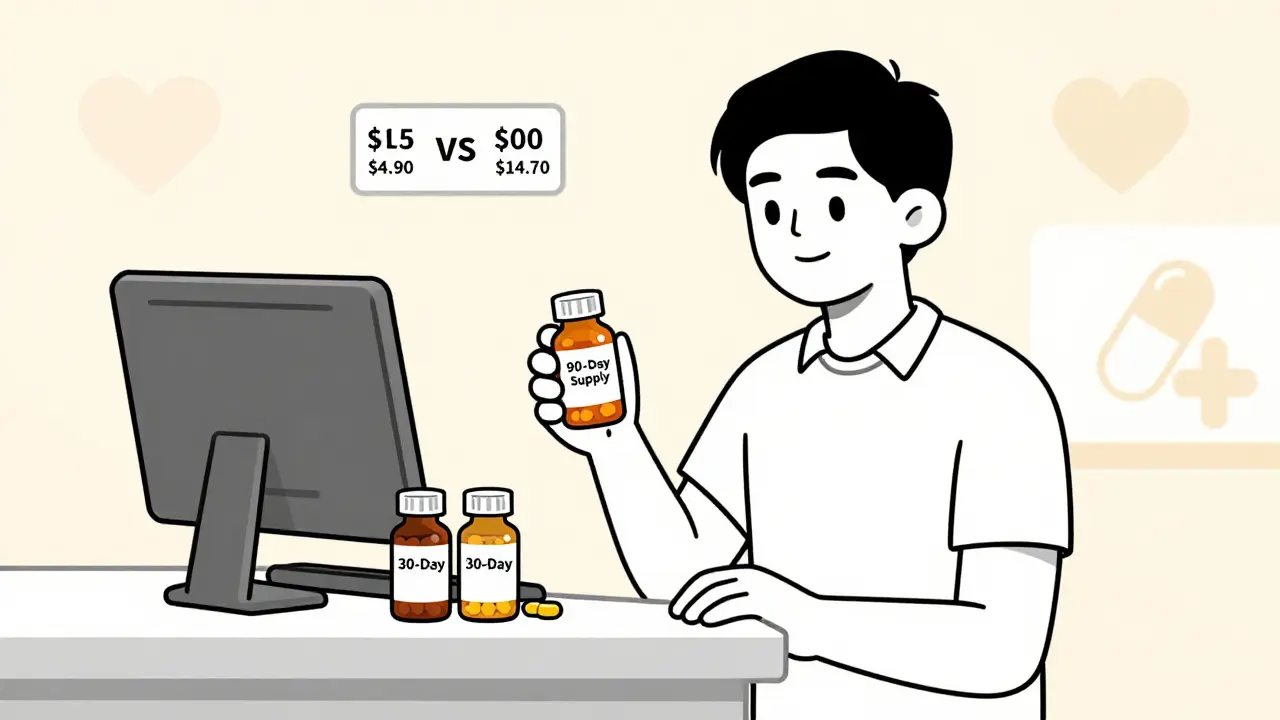
Most insurance plans charge you the same copay for a 90-day supply as they do for a 30-day one. That means you pay $4.90 once instead of $4.90 three times. Over a year, that’s $39.20 saved on just one medication. Multiply that by three or four pills you take daily, and you’re looking at over $100 saved annually-just by asking for a longer supply. It’s not magic. It’s how the system works. Pharmacy benefit managers (PBMs) and insurers set up these deals because they want you to stick with your meds. When you get 90 days at once, you’re less likely to skip doses or run out. That’s better for your health-and cheaper for the system overall.Who Qualifies for a 90-Day Fill
Not every pill qualifies. You need to be taking a medication for a chronic condition. That means drugs you use every day, long-term. Common examples include:- High blood pressure meds (like lisinopril or amlodipine)
- Cholesterol drugs (like atorvastatin or rosuvastatin)
- Diabetes medications (like metformin or glimepiride)
- Thyroid pills (like levothyroxine)
- Antidepressants or anti-anxiety meds (if taken regularly)
How to Get a 90-Day Prescription
There are two ways to get a 90-day supply, and both are simple. Option 1: Ask your doctor When you go in for your next appointment, say: “I’ve been taking this medication for months without issues. Can you write this for a 90-day supply?” Most doctors will say yes. They know it helps you stay on track and reduces waste. Option 2: Ask your pharmacy If your prescription still has refills left, walk into your local pharmacy and ask: “Can I get a 90-day fill instead of 30?” Many pharmacies will do it on the spot-even if the original script says 30 days. As long as your insurance allows it and you’ve been taking the drug safely, they can dispense three months’ worth. Some pharmacies, like CVS and Walgreens, now offer 90-day fills right at the counter. You don’t have to wait for mail-order. You can pick it up the same day.
Mail-Order vs. Retail Pharmacy
You’ve got two main options: getting your meds delivered or picking them up in person.| Feature | Mail-Order | Retail Pharmacy |
|---|---|---|
| Cost | Usually lowest copay | Same or slightly higher |
| Delivery | Free shipping, no trip needed | Pick up in person |
| Convenience | Best for busy people | Best if you need it fast |
| Speed | Takes 5-10 days | Same-day pickup |
| Refills | Auto-refill options | Manual refill each time |
How Much Can You Really Save?
Let’s say you take a $120/month drug. With 30-day fills, you pay $4.90 per fill. That’s $58.80 a year. With a 90-day fill? Still $4.90-but now you get 90 days. That’s only four fills a year, not twelve. Total cost: $19.60. You just saved $39.20 on that one pill. Do that for three other meds, and you’re saving over $100 a year-no extra work, no new insurance. According to UnitedHealth Group, Americans already save $600 million a year using 90-day fills. If more people used them, that number could hit $23 billion over ten years.What to Watch Out For
It’s not always smooth sailing. Here are the common roadblocks-and how to fix them. 1. Insurance won’t cover it Some plans only allow 90-day fills for mail-order, not retail. Others don’t cover certain drugs at all. Solution: Call your insurer. Ask: “Does my plan cover 90-day fills for [medication name] at retail pharmacies?” Write down the answer. 2. The pharmacy says no Some staff aren’t trained on this. If they refuse, ask to speak to the pharmacist. Say: “I know this is allowed under my plan. Can you check with your benefits team?” Most will fix it once they look it up. 3. You need prior authorization For some high-cost drugs, your insurer might require extra paperwork. Your doctor’s office can handle this. Just ask them to submit it when they send the 90-day script. 4. You’re worried about stock If you’re afraid of getting too much medicine, remember: most pills last years if stored properly. Keep them in a cool, dry place. If you stop taking the drug, you can return unopened bottles to the pharmacy for credit.
Real Benefits Beyond Money
Saving money is great. But the real win is better health. People who get 90-day fills are far more likely to take their meds consistently. That means fewer hospital visits, fewer complications, and better control of conditions like diabetes and heart disease. You also cut down on trips to the pharmacy. Instead of 12 visits a year, you make just four. That’s eight fewer errands. Less time stuck in traffic. Less stress. Less chance of missing a dose because you were too busy.What to Do Next
Here’s your simple action plan:- Make a list of all the medications you take every day for more than 3 months.
- Check your last prescription label. Do you still have refills left?
- Call your doctor’s office and ask if they can write a 90-day script for each one.
- Call your pharmacy and ask if they can fill your current script for 90 days.
- Ask your insurer if 90-day fills are covered for each drug.
- Choose mail-order if you want the lowest price and don’t mind waiting. Choose retail if you need it fast.
Final Thought
This isn’t a trick. It’s a standard benefit built into your insurance plan. Millions of people use it. But most don’t know it exists. You’re not asking for a favor. You’re asking for what you’re already entitled to. Start with one medication. See how much you save. Then do it again with the next. In a few months, you’ll wonder why you didn’t do this sooner.Can I get a 90-day fill for any medication?
No. Only maintenance medications for chronic conditions qualify-like those for high blood pressure, diabetes, cholesterol, thyroid issues, or depression. You also need to have taken the drug before without problems. New prescriptions or short-term meds (like antibiotics) won’t qualify.
Do I have to use mail-order to get a 90-day fill?
No. Many retail pharmacies like CVS, Walgreens, and Rite Aid now offer 90-day fills in-store. You can pick them up the same day. Mail-order is usually cheaper, but retail gives you instant access and face-to-face help from a pharmacist.
Will my copay be higher for a 90-day supply?
Almost never. Most insurance plans charge the same copay for 30 and 90-day supplies. That means you pay $4.90 once instead of $4.90 three times. Some plans even offer a lower copay for 90-day fills. Always check your plan details or call your insurer to confirm.
What if my doctor won’t write a 90-day script?
Ask why. If it’s because you’re new to the medication, they may want to start with 30 days. But if you’ve been taking it for months with no issues, they should be willing. If they refuse without a good reason, ask for a referral to another provider or call your insurance-they often have guidelines that support 90-day fills for stable patients.
Can I switch from mail-order to retail later?
Yes. You can switch anytime. If you start with mail-order and later want to pick up your meds locally, just call your pharmacy and ask them to transfer your prescription. You’ll need to confirm your insurance covers retail 90-day fills first. Most do.
Is it safe to keep 90 days of medication at home?
Yes. Most pills are stable for years if stored properly-in a cool, dry place away from sunlight and moisture. Avoid keeping them in the bathroom or near the kitchen sink. If you stop taking the medication, many pharmacies will take back unopened bottles for credit or safe disposal.
How do I know if my insurance covers 90-day fills?
Call the number on your insurance card and ask: “Does my plan allow 90-day fills for maintenance medications at retail pharmacies?” Be ready to name your specific drug. You can also check your plan’s website under “pharmacy benefits” or “formulary.”
10 Comments
Jan Hess
January 15 2026
Just did this for my blood pressure med and saved $40 in one go. No brainer. Why aren’t more people doing this
Sohan Jindal
January 17 2026
This is how the big pharma and insurance companies trick you. They want you dependent. They don’t care if you save money. They just want you hooked. Next they’ll be selling you 180-day fills and calling it ‘patriotic’
Frank Geurts
January 18 2026
It is, indeed, a matter of considerable public interest that such a straightforward, cost-effective mechanism remains underutilized by the general populace; one might reasonably infer that systemic informational deficits, rather than structural impediments, are the primary cause of this phenomenon.
Arjun Seth
January 20 2026
You think this is about saving money? No. This is about control. They want you to take pills forever. They don’t want you healed. They want you paying. Always paying. Look at the pharma ads on TV - they don’t sell cures. They sell forever.
Ayush Pareek
January 21 2026
This is such a simple win. I told my dad about it last month and he’s now saving $120 a year on his diabetes meds. He didn’t even know he could ask. You don’t need to be a genius - just brave enough to say ‘Can I get more?’
Niki Van den Bossche
January 22 2026
Oh please. You’re all so naive. This is just the tip of the iceberg. The real agenda? Once you’re on 90-day fills, they start tracking your habits, your refill patterns, your health data - and sell it to data brokers. You think you’re saving money? You’re becoming a product.
Iona Jane
January 23 2026
I tried this once. The pharmacy said no. Then my insurance said I needed prior auth. Then my doctor ghosted me. Now I’m in the ER again. This system is rigged. They want you sick. They want you desperate. I’m not alone.
Jaspreet Kaur Chana
January 25 2026
Bro in India I did this with my thyroid pills last year - saved over ₹15,000 in 12 months. Pharmacist was shocked I even asked. But I just said ‘Yaar, maine yeh 6 months se le raha hoon, 90 days ka de do na?’ He laughed and did it. No drama. Just ask. Simple.
Haley Graves
January 26 2026
If you’re on maintenance meds and not doing this, you’re leaving money on the table. It’s not complicated. Call your doctor. Call your pharmacy. Call your insurer. Do it now. Your future self will thank you.
Nishant Garg
January 27 2026
It’s funny how something so simple - asking for more pills at once - becomes this radical act of self-advocacy. We’ve been conditioned to wait, to obey, to not question. But here’s the truth: your insurance isn’t your enemy. It’s a contract. And you’re owed the full benefit. The pharmacy staff? Most of them are overworked and undertrained. They’re not hiding anything - they just don’t know you’re allowed to ask. So ask. Loudly. Politely. Repeatedly. Until they do. Because you’re not begging. You’re claiming what’s yours. And if they push back? Say ‘I’ll speak to your manager.’ And then do it. That’s the power move. Not the savings. The audacity.