Sudden shortness of breath could be more than just being out of shape
If you’ve ever felt like you can’t catch your breath after walking up a flight of stairs - and it came out of nowhere - you might have brushed it off as anxiety, asthma, or just getting older. But if that breathlessness is new, sharp, and doesn’t improve with rest, it could be a pulmonary embolism. This isn’t a rare scare. About 70 out of every 100,000 people in the U.S. get one each year. And roughly 100,000 die from it annually. The scary part? Many of those deaths happen because the warning signs are ignored or misdiagnosed.
Pulmonary embolism (PE) happens when a blood clot, usually from a deep vein in the leg, breaks loose and travels to the lungs. It blocks blood flow, and suddenly, your body can’t get enough oxygen. The most common symptom? Sudden shortness of breath. In fact, 85% of people with PE report this as their first sign. It doesn’t always feel like a heart attack. Sometimes it’s just a quiet, persistent gasp - like your lungs forgot how to work.
What else might you feel besides breathlessness?
Shortness of breath is the big red flag, but PE rarely comes alone. Chest pain is the next most common symptom, reported by 74% of patients. It’s often sharp and gets worse when you breathe in deeply or cough. People mistake it for a heart problem, but it’s not your heart - it’s your lungs screaming because blood isn’t flowing right.
You might also have:
- A dry cough - or worse, coughing up blood (23% of cases)
- A racing heart (over 100 beats per minute in 30% of cases)
- Fast breathing (more than 20 breaths per minute in over half)
- Swelling or pain in one leg (44% of cases - that’s often where the clot started)
- Fainting or dizziness (14% - this is a major warning sign
Some people feel fine sitting down, then collapse when they stand up. Others have mild symptoms for days before something triggers a crisis. One patient on a health forum said she thought she had anxiety for three weeks - until she passed out in the grocery store. That’s not uncommon. In fact, 68% of people see a doctor two or more times before getting the right diagnosis. Too often, PE is called asthma, pneumonia, or panic attacks.
Why is PE so hard to diagnose?
Because its symptoms look like a dozen other things. A doctor might hear your wheezing and think asthma. Or see your elevated heart rate and assume it’s stress. Even in hospitals, if you’re young, healthy, and don’t have a history of clots, PE might not even cross their mind.
But there are clues that should raise suspicion:
- Unexplained low oxygen levels on a pulse oximeter - especially if your chest X-ray looks normal
- A history of recent surgery, long travel, or being immobile for days
- Recent cancer diagnosis or chemotherapy
- Previous blood clots - if you’ve had one before, your risk of another is 33% within 10 years
- Leg swelling or tenderness - even if you didn’t notice it
One study showed that when patients had normal chest X-rays but low oxygen and fast breathing, PE was the cause in over 40% of cases. That’s why doctors should never dismiss breathlessness just because your lungs look clear on a scan.
How do doctors confirm a pulmonary embolism?
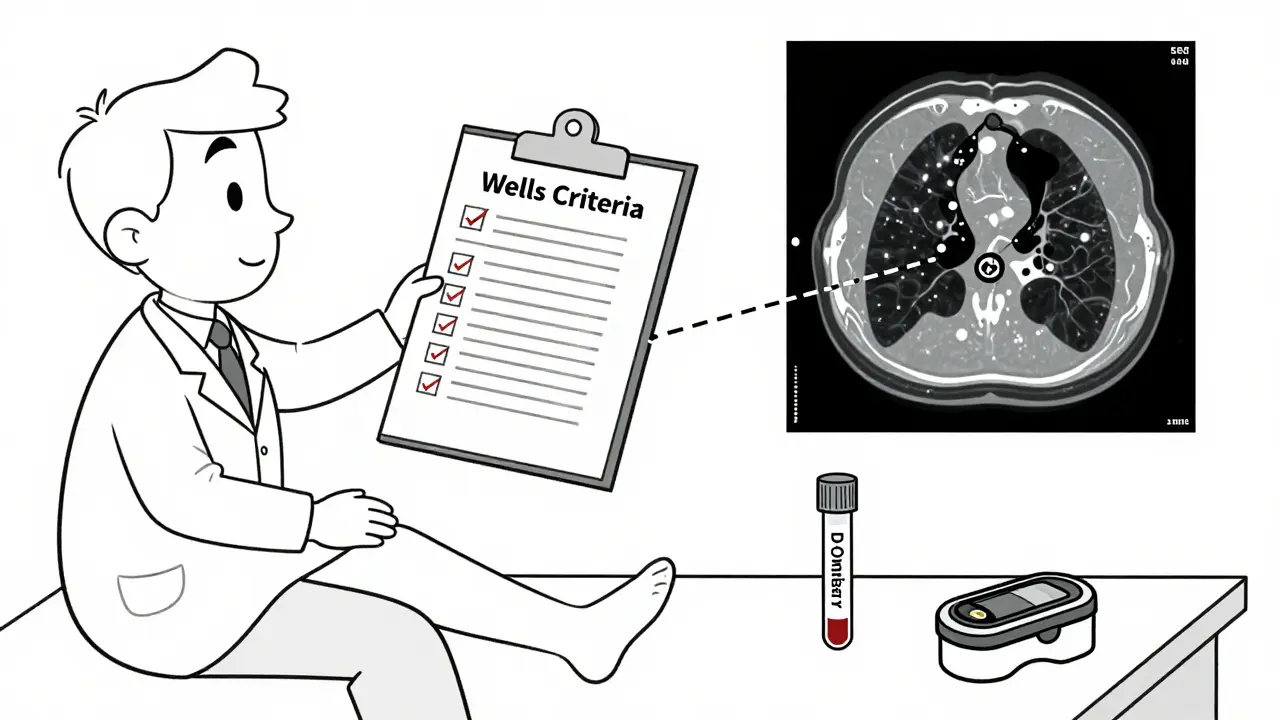
If PE is suspected, doctors follow a step-by-step process. It’s not guesswork. It’s science.
Step 1: Clinical scoring
Two tools are used to estimate your risk: the Wells Criteria and the Geneva Score. These aren’t fancy machines - they’re simple checklists. Did you have recent surgery? Do you have leg swelling? Is your heart rate over 100? Are you on birth control or hormone therapy? Each answer adds points. If your score is low, you’re likely not in danger. If it’s high, you need immediate testing.
Step 2: D-dimer blood test
This test looks for a protein fragment released when a clot breaks down. If the result is negative and your clinical score is low, PE is ruled out 97% of the time. But here’s the catch: D-dimer goes up with age, pregnancy, infection, cancer, or recent surgery. So if you’re over 50, a negative test doesn’t mean much on its own. That’s why doctors now use age-adjusted D-dimer levels - the cutoff rises by 10 ng/mL for every year over 50. This cuts down on unnecessary scans by over a third.
Step 3: CT Pulmonary Angiography (CTPA)
This is the gold standard. You get an IV with contrast dye, then a CT scan of your chest. It shows exactly where the clot is. Sensitivity? 95%. Specificity? 96%. That means it almost never misses a clot - and almost never gives a false alarm. It’s fast, accurate, and available in most hospitals. Radiation exposure is low - about the same as a cross-country flight.
If you can’t have contrast dye (due to kidney issues or allergy), doctors turn to a ventilation/perfusion (V/Q) scan. It’s less common, needs special equipment, and isn’t available everywhere - only 78% of major hospitals in developed countries have it. But it’s still reliable, with 85% sensitivity and 95% specificity.
Step 4: Ultrasound of the legs
If you have swelling or pain in one leg, an ultrasound can find a deep vein thrombosis (DVT). If it’s positive, and your symptoms match PE, you don’t always need a CT scan. A clot in the leg + sudden breathlessness = PE until proven otherwise. Ultrasound is quick, painless, and 90%+ accurate for clots in the big veins.
What happens if you’re unstable?
If you’re collapsing, your blood pressure is dropping, or you’re in shock - time isn’t on your side. In these cases, doctors skip the D-dimer and go straight to a bedside echocardiogram. This ultrasound of the heart checks for right ventricular strain - a sign that the heart is struggling to pump blood through blocked arteries. If it’s there, you likely have a massive PE. You need emergency treatment immediately - clot-busting drugs or even surgery.
One hospital system reduced time-to-CT from over two hours to under 45 minutes by creating a dedicated PE pathway. Mortality dropped from 8.2% to 3.1%. That’s not a small win - that’s life or death.
Who’s at highest risk?
You might think PE only affects older people or those with chronic illness. But it can strike anyone.
- Recent surgery or trauma - especially hip or knee replacements
- Long flights or car rides - sitting for more than 4 hours increases risk
- Cancer - cancer patients have nearly 5 times higher risk
- Pregnancy or postpartum - hormonal changes and pressure on veins
- Hormone therapy or birth control pills - especially if you smoke or are over 35
- Family history of clots - inherited clotting disorders
- Obesity - adds pressure on veins and slows blood flow
And here’s something many don’t know: if you’ve had a PE or DVT before, your chance of another one within 10 years is one in three. That’s why doctors don’t just treat the clot - they look for why it happened in the first place.
New tools are making diagnosis faster and smarter
Technology is helping. Artificial intelligence is now being used to analyze CT scans. One AI tool, called PE-Flow, detected clots with 93.7% accuracy - better than some radiologists. Hospitals are forming specialized teams called PERT (Pulmonary Embolism Response Teams) - a group of specialists who jump in when PE is suspected. These teams cut treatment delays by 3 days and lower death rates by over 4%.
Research is also looking at new blood markers beyond D-dimer. One study combined D-dimer with two other proteins and got a 98.7% accuracy rate for ruling out PE in intermediate-risk patients. That could mean fewer scans, less radiation, and faster answers.
What you can do - before it’s too late
You can’t always prevent PE, but you can spot it early.
- If you have sudden shortness of breath - especially with chest pain or leg swelling - don’t wait. Go to the ER.
- Don’t let anyone tell you it’s just anxiety. If you feel something’s wrong, trust your gut.
- If you’ve had a clot before, ask your doctor about long-term prevention - blood thinners might be needed for months or years.
- Move during long trips. Walk every hour. Wear compression socks if you’re at risk.
- Know your family history. If a close relative had a clot before age 50, get tested for inherited conditions.
PE doesn’t care if you’re fit, young, or healthy. It doesn’t announce itself with a siren. It whispers - with breathlessness, with pain, with a fainting spell. And if you listen, you might just save your life.
Can you have a pulmonary embolism without knowing it?
Yes - especially if the clot is small. Some people have tiny clots in the outer edges of the lungs that cause mild, temporary breathlessness they write off as fatigue or allergies. But even small clots can grow or break off again. If you’ve had unexplained shortness of breath, leg swelling, or chest pain, it’s not worth ignoring.
Is a pulmonary embolism the same as a heart attack?
No. A heart attack is caused by a blocked artery in the heart. A pulmonary embolism is a clot in the lungs. The chest pain can feel similar - sharp and worse with breathing - but the cause and treatment are completely different. One affects the heart muscle; the other affects lung blood flow. Misdiagnosing PE as a heart attack can delay life-saving treatment.
Can a blood test alone confirm a pulmonary embolism?
No. The D-dimer test can only rule out PE - not confirm it. A high D-dimer means there’s clotting somewhere in the body, but it doesn’t say where. It can be elevated after surgery, infection, pregnancy, or even with age. Only imaging like a CT scan or V/Q scan can show the clot in the lungs.
How long does it take to recover from a pulmonary embolism?
Recovery varies. Most people start feeling better in days to weeks after starting blood thinners. But full recovery can take months. Some have lasting lung damage or develop chronic high blood pressure in the lungs (chronic thromboembolic pulmonary hypertension). That’s why follow-up scans and long-term monitoring are important - especially if you had a large clot.
Are there alternatives to CT scans for diagnosing PE?
Yes - a V/Q scan is the main alternative, especially if you can’t have contrast dye. It’s less common and requires nuclear medicine equipment, so it’s not available everywhere. Ultrasound of the legs can also support diagnosis if a clot is found. But for most people, CTPA remains the fastest and most accurate option.
Can stress or anxiety cause symptoms like a pulmonary embolism?
Anxiety can cause shortness of breath and a racing heart - but it won’t cause low oxygen levels with a normal chest X-ray, or sudden leg swelling. If you have symptoms that don’t fit your usual anxiety pattern - especially if they came on suddenly - don’t assume it’s just stress. PE can mimic anxiety, but it’s a medical emergency. Always get checked.
What happens if PE is left untreated?
Untreated PE can be fatal. Large clots can block major lung arteries, causing sudden cardiac arrest. Even smaller clots can lead to long-term lung damage or chronic high blood pressure in the lungs. About 1 in 3 people with untreated PE die within the first few hours. Early diagnosis and treatment with blood thinners reduce death risk by over 80%.

9 Comments
Madhav Malhotra
January 11 2026
Man, I never realized how sneaky PE can be. In India, we often brush off breathlessness as heat or stress, especially after long flights. My uncle had one after a 14-hour trip to Dubai - thought it was just fatigue. Got diagnosed only after he collapsed at the temple. This post saved my life - I’m getting my mom checked now.
Priya Patel
January 12 2026
OMG I had this exact thing last year. Thought I was having a panic attack. Went to urgent care twice. They gave me an inhaler and told me to breathe deep. I almost didn’t go back the third time - but my leg was swelling so bad I couldn’t wear my sandals. Turned out to be a PE. I’m alive because I trusted my gut. Don’t ignore the whispers.
Jason Shriner
January 13 2026
so like… if you’re young and fit and you just ran 5k and then couldn’t catch your breath… is it still pe? or just your lungs being dramatic? like… i feel like we’re being scared into panic buying ct scans now
Sean Feng
January 13 2026
another medical post pretending to be a thriller novel. breathlessness is common. pe is rare. stop fearmongering with 85% stats and no context. also why are you talking like a textbook that got drunk at a conference
Christian Basel
January 15 2026
While the clinical pathways described are generally aligned with current ACCP guidelines, the overreliance on CTPA without adequate pretest probability stratification may contribute to iatrogenic radiation exposure and contrast-induced nephropathy in low-risk cohorts. The age-adjusted D-dimer algorithm, while validated in multiple cohorts, exhibits reduced specificity in inflammatory states.
Vincent Clarizio
January 16 2026
Let me tell you something about the human body - it doesn’t lie. But doctors? They’re trained to see patterns, not people. I’ve seen a 28-year-old athlete with zero risk factors get sent home three times with ‘anxiety’ while his oxygen saturation dropped to 89%. Three days later he was on a ventilator. This isn’t about statistics. It’s about listening. The body whispers. The mind screams. The system? It’s still asleep. And every time it ignores a whisper, someone dies quietly in a hallway waiting for a CT that never comes. We’ve turned medicine into a checklist game. But PE doesn’t care about your EHR protocols. It just waits. And when it strikes, it doesn’t ask permission. It takes. And then it’s gone. And the family’s left wondering why no one listened. You want to save lives? Stop treating symptoms. Start treating silence.
Alex Smith
January 18 2026
So let me get this straight - if I’m on birth control, flew to Bali, and now my calf feels like it’s full of cement, I should skip the ‘maybe it’s just sore’ phase and go straight to the ER? Cool. Got it. Thanks for not making me feel like an idiot for thinking I was just lazy. Also, AI detecting clots better than radiologists? That’s either terrifying or the future. Probably both.
Roshan Joy
January 18 2026
Great breakdown! In India, we don’t talk enough about blood clots. My cousin had a PE after her baby - no one warned her. She was told it was postpartum fatigue. Please share this with your friends, especially if you’re pregnant, traveling, or on pills. Knowledge is the best medicine.
Jason Shriner
January 19 2026
you said it bro. pe is like the ghost of medicine. no one sees it till it's too late. and then suddenly everyone's an expert. i'm getting my legs scanned next week just in case. thanks for the nudge