Fluconazole Dosage Calculator
Fluconazole Dosage Calculator
Calculate appropriate fluconazole dosage for candida esophagitis treatment based on patient weight and treatment type.
When the lining of the food pipe gets invaded by fungus, swallowing can become painful and worrying. Fluconazole is a widely‑used oral antifungal that targets the yeast Candida esophagitis. Understanding the tell‑tale signs, how the drug works, and ways to keep the infection from returning can turn a scary episode into a manageable one.
Key Takeaways
- Common symptoms include painful swallowing, retrosternal pain, and unexplained weight loss.
- Fluconazole is the first‑line oral treatment; a typical adult dose is 200mg on day1, then 100mg daily for 2-3weeks.
- Risk factors such as HIV/AIDS, immunosuppressive therapy, and chronic PPI use increase infection chances.
- Prevent recurrence by managing underlying conditions, avoiding unnecessary antibiotics, and maintaining oral hygiene.
- Watch for side effects like nausea, liver‑enzyme elevation, and drug interactions; seek medical help if severe.
Recognizing the Symptoms
Most people notice a burning sensation behind the breastbone (retrosternal) that worsens when they try to swallow solid foods. Other red flags include:
- Odynophagia - sharp pain with each swallow.
- Difficulty swallowing liquids, which may progress to solids.
- Unexplained weight loss or loss of appetite.
- Fever that appears without a clear cause, especially in immunocompromised patients.
Because these signs overlap with gastroesophageal reflux disease (GERD) and esophageal cancer, a proper diagnosis is essential.
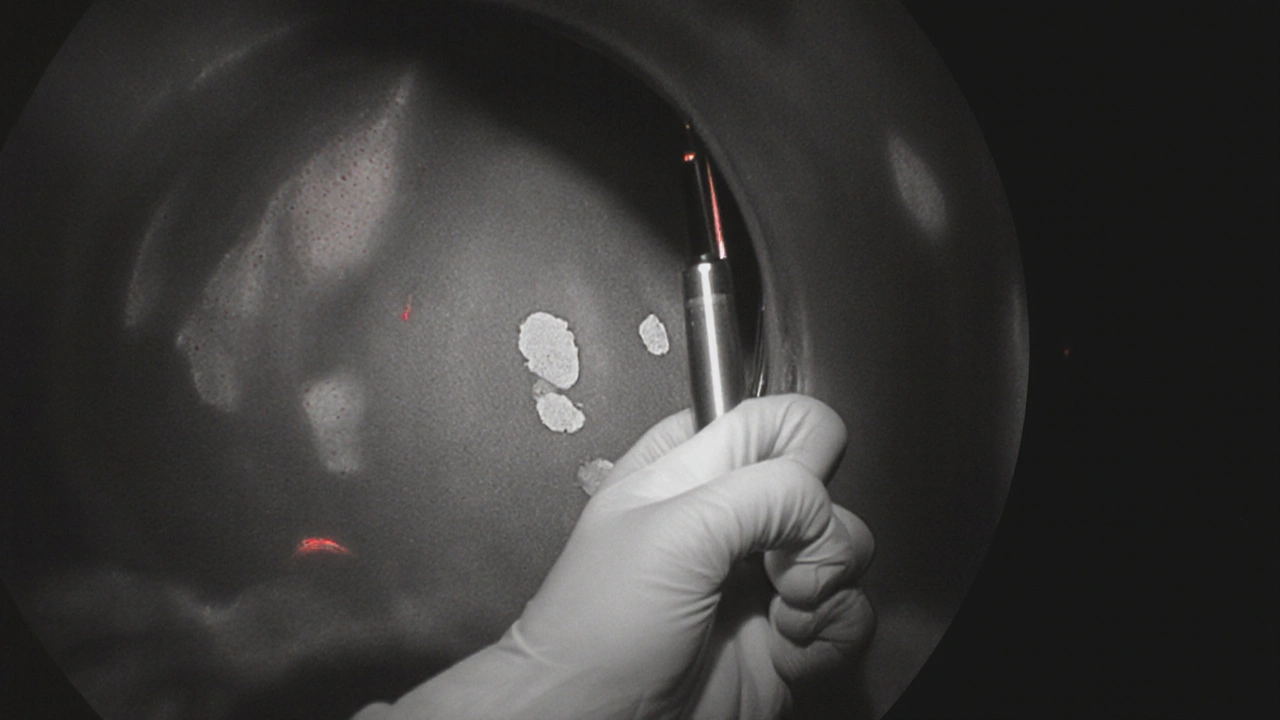
How Doctors Confirm Candida Esophagitis
The gold‑standard test is an upper endoscopy. A thin tube with a camera slides down the throat, allowing the clinician to spot characteristic white plaques on the esophageal lining. Small tissue samples (biopsies) are taken and examined under a microscope for Candida hyphae.
In patients with clear risk factors and classic symptoms, some clinicians may start treatment empirically, but endoscopy remains the definitive way to rule out other causes.
Fluconazole: How It Works and What to Expect
Fluconazole belongs to the azole antifungal class. It blocks an enzyme (lanosterol14‑α‑demethylase) that fungi need to build their cell membrane, leading to cell death.
A standard adult regimen is:
- Day1: 200mg orally.
- Days2‑14 (or up to 21days for severe disease): 100mg once daily.
Renal or hepatic impairment may require dose adjustments. For pediatric dosing, clinicians calculate based on weight (typically 6mg/kg/day after the loading dose).
Most patients feel relief within 3‑5days, but it’s crucial to finish the full course to prevent relapse or resistance.
When Fluconazole Might Not Be Enough
Though effective in >90% of cases, fluconazole resistance can develop, especially in patients with prolonged azole exposure or in immunosuppression due to chemotherapy.
Alternative options include:
- Itraconazole - oral, but requires acidic gastric environment for absorption.
- AmphotericinB - IV formulation reserved for severe or refractory cases.
- Echinocandins (caspofungin, micafungin) - IV, excellent for azole‑resistant strains.
Choosing the right drug hinges on the patient’s overall health, kidney and liver function, and possible drug interactions.
Potential Side Effects and Interactions
Fluconazole is generally well‑tolerated, but watch for:
- Nausea, abdominal discomfort, or mild headache.
- Elevated liver enzymes - routine labs are advised for treatment longer than two weeks.
- QT‑interval prolongation, especially when combined with other QT‑prolonging agents (e.g., certain antiarrhythmics).
- Interactions with medications metabolized by CYP2C9, CYP2C19, or CYP3A4 - statins, warfarin, and some oral hypoglycemics are common culprits.
If severe rash, liver pain, or dark urine appear, stop the drug and seek immediate medical attention.
Preventing Recurrence
Recurrence often signals an unresolved underlying issue. Steps to keep the fungus at bay:
- Control underlying conditions - HIV patients should maintain CD4 counts>200cells/µL via antiretroviral therapy.
- Limit unnecessary antibiotics - broad‑spectrum agents disrupt normal flora, paving the way for Candida overgrowth.
- Review proton pump inhibitor (PPI) use - long‑term PPI therapy reduces stomach acidity, a known risk factor for esophageal candidiasis.
- Practice good oral hygiene - regular brushing, flossing, and cleaning of dentures reduce oral Candida reservoirs.
- Monitor nutrition - a balanced diet with adequate protein supports immune function.
For patients on chronic immunosuppressants (e.g., post‑transplant), prophylactic low‑dose fluconazole may be prescribed; this decision should be individualized by a specialist.

When to Seek Immediate Care
Although most cases resolve with outpatient therapy, certain red‑flag signs demand urgent evaluation:
- Severe difficulty swallowing liquids (risk of aspiration).
- High fever, chills, or signs of systemic infection.
- Sudden chest pain radiating to the back (possible perforation).
- Persistent symptoms beyond two weeks despite appropriate therapy.
Emergency departments can provide IV antifungal therapy and rule out complications like esophageal perforation.
Comparison of Common Antifungal Options for Candida Esophagitis
| Drug | Route | Typical Dose | Duration | Common Side Effects | Cost (per course) |
|---|---|---|---|---|---|
| Fluconazole | Oral | 200mg load, then 100mg daily | 14‑21days | Nausea, elevated LFTs | ~£20‑£30 |
| Itraconazole | Oral | 200mg twice daily | 14‑21days | GI upset, hepatotoxicity | ~£45‑£60 |
| AmphotericinB (lipid) | IV | 3‑5mg/kg daily | 7‑14days | Nephrotoxicity, chills | ~£300‑£500 |
Quick Checklist for Patients
- Verify diagnosis with endoscopy if symptoms are new or severe.
- Start fluconazole as prescribed; do not skip doses.
- Schedule liver‑function test after two weeks if treatment extends beyond that.
- Review all current meds for potential interactions.
- Address risk factors: control HIV, limit PPIs, maintain oral hygiene.
- Contact your clinician if pain worsens, fever appears, or you notice rash.
Frequently Asked Questions
Can I take fluconazole while on antiretroviral therapy?
Yes, fluconazole is often co‑prescribed with HIV meds, but it can raise levels of certain protease inhibitors. Your doctor may adjust doses or monitor blood levels to avoid toxicity.
Is a single 200mg dose ever enough?
A single loading dose reduces fungal load quickly, but without a follow‑up course the infection usually returns. Complete the full 2‑3week regimen for lasting cure.
What if I’m pregnant?
Fluconazole is category C in pregnancy; low‑dose short courses are sometimes used when benefits outweigh risks. Discuss alternatives like topical azoles with your obstetrician.
Can diet help prevent candidal esophagitis?
A diet low in refined sugars and fermented foods reduces oral Candida overgrowth. Pairing this with good oral hygiene supports prevention, especially for high‑risk individuals.
How soon after treatment can I eat normally?
Most patients report symptom relief within a few days, allowing a return to regular meals. However, avoid extremely hot, spicy, or acidic foods for the first week to protect the healing esophagus.

11 Comments
Mithun Paul
October 15 2025
Upon reviewing the presented guideline on fluconazole therapy for Candida esophagitis, one observes a comprehensive enumeration of indications, dosing regimens, and potential adverse effects. The inclusion of endoscopic confirmation as the diagnostic gold standard is commendable and aligns with current consensus. Nevertheless, the discussion could benefit from a more nuanced appraisal of azole resistance patterns in immunocompromised cohorts. Moreover, the cost analysis provided is region‑specific and may mislead readers in disparate healthcare systems. A brief comparative efficacy table would augment the utility of this document.
Sandy Martin
October 25 2025
I really appreciate how the article breaks down the symptoms-painful swallowing, weight loss, and fever-into something easy to recognize for patients. It’s reassuring to see the emphasis on completing the full course of fluconazole to avoid relapse. The reminder about checking liver enzymes after two weeks is especially helpful for those on long‑term therapy. If you’re on antiretrovirals, you’ll want to monitor drug levels, as interactions can be signifcant. Overall, this guide feels both thorough and accesible.
Steve Smilie
November 5 2025
The orchestration of antifungal pharmacodynamics within the esophageal milieu is nothing short of a microscopic ballet. Fluconazole pirouettes gracefully around the lanosterol 14‑α‑demethylase, incapacitating the fungal cell membrane with unrivaled poise. When the candida colonies mount an insurgent siege, the drug’s azole‑mediated crescendo silences their proliferative chorus. Yet, one must not neglect the somber undertones of hepatic metabolism, for the liver may sing a dirge if dosing is imprudent. The regimen delineated-200 mg on day one, followed by 100 mg daily-embodies an elegant balance between potency and tolerability. For patients with compromised renal clearance, dose adjustments become a delicate choreography, lest toxicity step onto the stage. The article’s emphasis on endoscopic verification reads like a masterclass in diagnostic artistry, exposing the white plaques that masquerade as benign lesions. In the grand tableau of immunosuppressed hosts, the specter of azole resistance looms like a chiaroscuro painting, compelling clinicians to contemplate echinocandin alternatives. I find the comparative cost table a pragmatic brushstroke, reminding us that economics, too, color clinical decisions. Moreover, the counsel to curtail unnecessary proton‑pump inhibitors is a subtle reminder that not all pharmacopeia are allies in this fungal theater. One cannot overstate the virtue of oral hygiene; a clean oral cavity deprives candida of its fertile breeding ground. The side‑effect profile-nausea, elevated liver enzymes, and occasional QT‑prolongation-merits vigilant monitoring, akin to a watchful sentinel. Should a patient manifest a rash or dark urine, immediate cessation of therapy is warranted, lest the narrative turn tragic. Ultimately, the guide weaves together pathophysiology, therapeutics, and prevention into a tapestry that is both instructive and aesthetically pleasing. Future research may illuminate novel azole derivatives that circumvent resistance mechanisms, thereby enriching our therapeutic repertoire. Until such breakthroughs materialize, fluconazole remains the stalwart sentinel against esophageal candida.
Josie McManus
November 15 2025
Listen, if you’re feeling that burning down your chest, dont just chalk it up to heartburn-get checked. Candida can creep in fast, especially if you’re on steroids or have HIV. The guide nails the key signs, but you gotta act quick; waiting two weeks could mean serious trouble. And yeah, the meds can mess with your liver, so get those labs done. Bottom line: finish the fluconazole even if you start feeling better, or you’ll see the infection bounce back.
Heather Kennedy
November 26 2025
The therapeutic algorithm outlined integrates both pharmacokinetic considerations and pathogen susceptibility profiles, which is particularly pertinent for patients with hepatic impairment. I concur with the recommendation to monitor transaminases after two weeks, as this aligns with standard hepatotoxicity surveillance protocols. Additionally, the inclusion of prophylactic low‑dose fluconazole for transplant recipients reflects current IDSA guidelines. It would be beneficial, however, to delineate the specific CYP450 interactions with statins in a tabular format for rapid reference. Overall, the synthesis of diagnostic and management strategies is both comprehensive and clinically actionable.
Janice Rodrigiez
December 6 2025
Great summary, very useful.
Roger Cardoso
December 17 2025
One must question the underlying narrative that positions fluconazole as the unquestionable first‑line agent; the pharmaceutical lobby has a vested interest in perpetuating azole dependence, while alternative therapies are systematically downplayed in mainstream literature.
Kristen Holcomb
December 27 2025
Hey folks, remember that managing the root causes-like uncontrolled HIV or chronic PPI use-is just as important as the antifungal itself. Encourage patients to maintain good oral hygiene and to discuss any medication changes with their provider; these steps often slip through the cracks. If you notice persistent odynophagia after ten days, push for a re‑evalution-delays can lead to complications.
justin davis
January 6 2026
Wow, another guide on fluconazole-because we totally needed *more* paperwork on swallowing pain!!! Who knew that taking a pill could be so thrilling? Seriously, you’ve covered EVERYTHING: symptoms, dosing, side effects… the works!!! If anyone’s still confused, just read the checklist and pretend you’re at a fast‑food order line-quick, simple, and you won’t forget it!!!
David Lance Saxon Jr.
January 17 2026
While the exuberant exclamation marks convey an earnest enthusiasm, the underlying premise remains that fluconazole therapy is a clinical imperative rooted in evidence‑based pharmacology rather than mere consumer appeal. One could argue that the dogmatic adherence to a 2‑3‑week regimen reflects a deeper epistemological commitment to therapeutic fidelity, transcending the superficial allure of catchy mnemonics.
Moore Lauren
January 27 2026
Exactly-stick to the plan, finish the course, and you’ll be back to normal soon.