Rebound Congestion Recovery Estimator
Track your recovery progress after stopping nasal decongestant sprays. This tool shows what to expect based on how many days you've stopped using the spray.
Recovery Status
Recovery Timeline
Worst symptoms - Peak congestion, difficulty breathing, sleep issues
- Severe nasal blockage
- Difficulty sleeping
- Headache
- Restlessness
Early improvement - Symptoms begin to decrease
- Less severe congestion
- Improved sleep
- Less need for saline rinses
Significant improvement - Most people see major relief
- Comfortable breathing
- Normal sleep patterns
- Reduced need for medications
Full recovery - Nasal tissue heals completely
- Normal nasal function
- No rebound congestion
- Improved sense of smell
Recommended Actions
Ever used a nasal spray for a stuffy nose, only to find your congestion got worse the next day? You’re not alone. What feels like a cold that won’t quit might actually be something called rhinitis medicamentosa - a condition caused by overusing nasal decongestant sprays. It’s not a cold. It’s not allergies. It’s your nose reacting to the very medicine you thought was helping.
How a Quick Fix Turns Into a Long-Term Problem
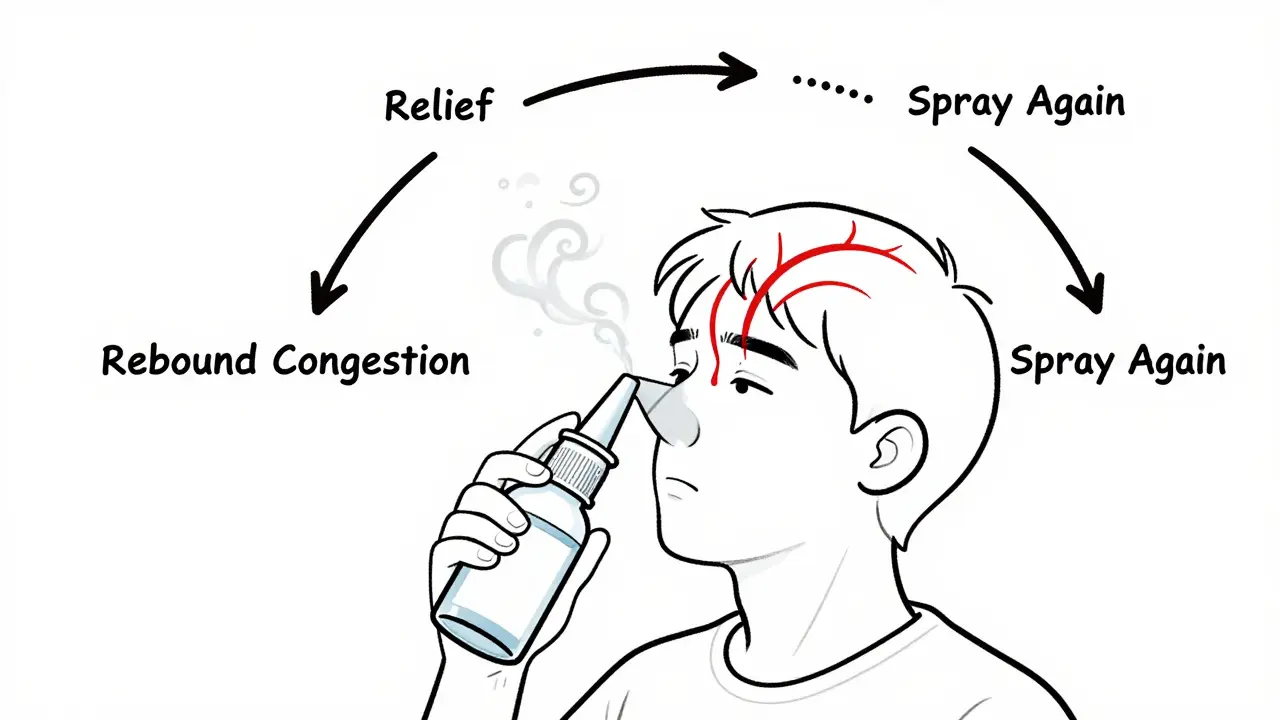
Nasal decongestant sprays like Afrin, Neo-Synephrine, and Oxymetazoline work fast. They shrink swollen blood vessels in your nose, giving you instant relief. But that relief only lasts a few hours. When the medicine wears off, the blood vessels don’t just return to normal - they swell back even bigger. This is called rebound congestion. It’s a cycle: spray → relief → congestion returns → spray again. After three to four days, your nose starts depending on the spray just to breathe normally. According to the National Center for Biotechnology Information (NCBI), this isn’t rare. About 10% of people who use these sprays longer than recommended end up with rhinitis medicamentosa. In the U.S. alone, around 500,000 cases are diagnosed every year. The NHS warns that using these sprays for more than a week makes your congestion worse. And it’s not just a nuisance - it can lead to mouth breathing, dry throat, snoring, and even nasal polyps if left unchecked.What Happens Inside Your Nose
Your nasal passages are lined with tiny blood vessels that expand when you’re congested. Decongestant sprays force them to shrink. But over time, your body gets used to the constant vasoconstriction. When you stop using the spray, those vessels overreact, flooding your nose with blood and causing even more swelling than before. Doctors describe the physical signs: red, swollen, sometimes granular nasal tissue. In advanced cases, the lining becomes dry, crusty, and even thin. You might feel like your nose is permanently blocked - even when you’re not sick. That’s the hallmark of rebound congestion. And unlike allergies or colds, there’s no runny nose or sneezing. Just relentless stuffiness.The Only Real Cure: Stopping the Spray
The hardest part? You have to stop using the spray. Completely. There’s no way around it. No trick. No shortcut. The only way to reverse rhinitis medicamentosa is to let your nose heal on its own. But stopping cold turkey can be brutal. The first few days are the worst. You might feel like you can’t breathe. Sleep becomes impossible. That’s normal. The good news? It doesn’t last forever. Most people start to feel better within 7 to 14 days. The key is sticking it out. Doctors at Mayo Clinic recommend a smart way to make it easier: stop the spray in one nostril first. Wait until that side clears up - usually 3 to 5 days - then stop it in the other. This gives your body a chance to adjust gradually. Patients who try this method report more manageable symptoms than those who quit both sides at once.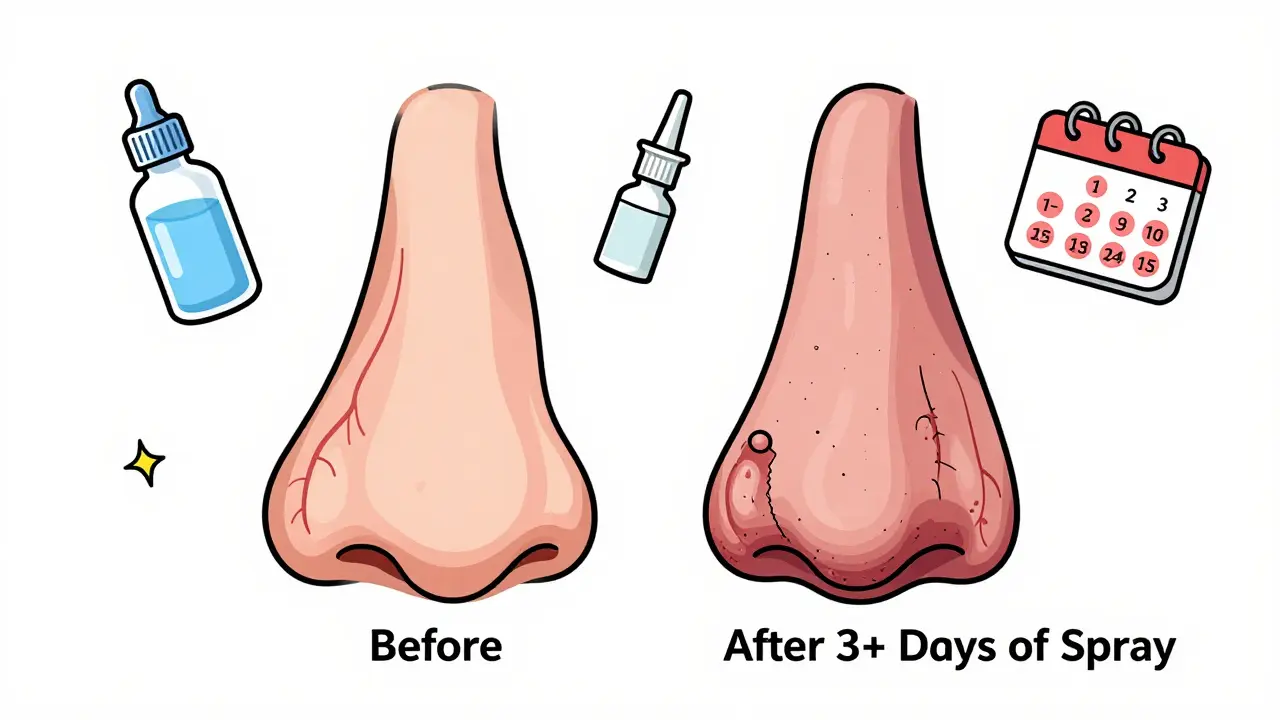
What to Use Instead: Proven Relief Strategies
While your nose heals, you need alternatives. Here’s what actually works:- Intranasal corticosteroids - Sprays like Flonase (fluticasone) and Nasonex (mometasone) are the gold standard. They reduce inflammation without causing rebound. Studies show 68-75% of users see major improvement after 2-4 weeks of daily use. Start using them the day you quit the decongestant spray.
- Saline nasal irrigation - Rinsing your nose with salt water (using a neti pot or squeeze bottle) helps clear mucus and soothe irritated tissue. A 2022 review found it helped 60% of patients during withdrawal. Use it 2-3 times a day, especially in the first week.
- Short-term oral steroids - For severe cases, doctors may prescribe a 5-day course of prednisone. A 2021 study showed 82% of patients had significant relief. This isn’t for everyone, but it can be a game-changer for those stuck in extreme discomfort.
- Humidifiers and hydration - Dry air makes congestion worse. Use a humidifier at night. Drink plenty of water. It keeps nasal tissues moist and helps your body recover faster.
What Doesn’t Work (And Why)
Don’t fall for quick fixes that make things worse:- Switching to another decongestant spray - You’re just restarting the cycle. Same problem, different brand.
- Oral decongestants like pseudoephedrine - They can help temporarily, but they raise blood pressure. One in seven people with high blood pressure had dangerous spikes in a 2021 study. Not worth the risk.
- Essential oils or home remedies alone - Steam, eucalyptus, or peppermint might feel soothing, but they don’t fix the underlying inflammation. They’re comfort, not treatment.
Why Some People Relapse - And How to Avoid It
It’s not uncommon to give up during the first week. The discomfort is real. A Cleveland Clinic study found that 22% of patients who didn’t get counseling went back to using decongestant sprays. But those who got clear instructions - and knew what to expect - had only a 7% relapse rate. Here’s what works:- Write down your plan. Know exactly when you’ll start corticosteroids and how often to use saline.
- Track your progress. Even if it feels like you’re getting worse, write down how you feel each day. You’ll see small improvements you’d otherwise miss.
- Don’t rush. It takes time. Most people see real improvement by day 10. Full recovery often takes 2-4 weeks.

Prevention: How to Never Get Here Again
The best treatment is avoiding rhinitis medicamentosa in the first place.- Never use nasal decongestant sprays for more than 3 days. That’s the rule. Period.
- Use saline irrigation first. The American College of Allergy, Asthma, and Immunology now recommends it as the first line of defense for congestion.
- Read the label. Since December 2022, the FDA requires all OTC nasal sprays to have a clear warning: “DO NOT USE MORE THAN 3 DAYS.” If your bottle doesn’t say that, it might be expired or mislabeled.
- If congestion lasts longer than a week, see a doctor. It’s probably not a cold - it could be allergies, a sinus infection, or something else that needs different treatment.
What’s New in Treatment
Research is moving fast. Early trials show promise for:- Azelastine nasal spray - an antihistamine that reduces congestion without rebound. Early studies show 65% effectiveness.
- Low-dose capsaicin - the compound in hot peppers. Applied as a nasal spray, it seems to reset nerve sensitivity in the nose. Trials at Massachusetts Eye and Ear show 70% success rates.
Real Stories: What Patients Say
One Reddit user, AllergySufferer89, wrote in June 2023: “After 3 weeks of Flonase and no Afrin, my nose finally cleared up - the first week was hell but worth it.” Another user on WebMD said: “I thought I was addicted to my spray. Turns out I was. Stopped both nostrils at once. First 5 days were torture. But by day 12, I could breathe through my nose for the first time in months.” The pattern is clear: pain now, freedom later.Can nasal decongestant sprays cause permanent damage?
Not usually, but long-term overuse can lead to permanent changes in nasal tissue. Chronic use can cause the lining to thin, become crusty, or even develop nasal polyps - noncancerous growths that block airflow. The risk of polyps increases by 15% after six months of daily spray use. Stopping early prevents this.
How long does rebound congestion last after stopping the spray?
Most people notice improvement between days 7 and 14. Severe symptoms peak around days 3-5. Full recovery typically takes 2-4 weeks. The longer you used the spray, the longer it takes to heal. But patience pays off - your nose will recover.
Is Flonase safe to use long-term?
Yes. Unlike decongestant sprays, intranasal corticosteroids like Flonase are designed for daily, long-term use. They reduce inflammation without causing rebound. Side effects are rare and mild - maybe a dry nose or slight nosebleed. They’re much safer than continuing to use decongestant sprays.
Can I use saline spray every day?
Absolutely. Saline spray or irrigation is safe for daily use - even multiple times a day. It helps clear mucus, moisturizes dry tissue, and reduces irritation. It’s not a cure by itself, but it’s a powerful support tool during recovery.
Why do some doctors recommend stopping one nostril at a time?
It’s a trick to make withdrawal easier. By keeping one side open, you maintain some airflow while the other side heals. Most patients who try this report less discomfort than those who quit both sides at once. It’s not magic - just smart pacing.
Should I avoid all nasal sprays if I’ve had rebound congestion?
No - just avoid decongestant sprays (oxymetazoline, phenylephrine). Corticosteroid sprays (Flonase, Nasonex), antihistamine sprays (Azelastine), and saline sprays are safe and often recommended. The issue isn’t nasal sprays in general - it’s the type you’re using.
14 Comments
Henry Jenkins
January 26 2026
Man, I didn’t realize how hooked I was on Afrin until I tried to quit. First three days were pure hell-felt like my sinuses were glued shut. I started Flonase the day I stopped, and honestly? That’s what saved me. Saline rinses twice a day helped too. It’s not glamorous, but it works. Took me 18 days to feel normal again. Now I use saline like it’s oxygen.
Ashley Karanja
January 27 2026
This is such a critical piece of medical literacy that gets buried under marketing hype. The pharmaceutical industry thrives on quick fixes, and rebound congestion is a textbook example of how convenience can rewire physiology. What’s fascinating is how the nasal vasculature develops tolerance-essentially, your body forgets how to regulate blood flow without pharmacological coercion. The fact that corticosteroids don’t trigger this is because they modulate inflammation at the cytokine level, not vasoconstrict outright. It’s not just about stopping the spray-it’s about retraining your autonomic nervous system’s response to mucosal stress.
Karen Droege
January 28 2026
I’ve been a nasal spray addict for 7 years. I thought I was just chronically congested. Turns out I was poisoning my own nasal lining. I followed the one-nostril method and holy hell-it was brutal but doable. I cried on day 4. I screamed into a pillow on day 5. But by day 11? I woke up and actually sniffed. Like, I could smell coffee. I hadn’t smelled coffee in over two years. If you’re reading this and still using Oxymetazoline-stop. Now. Your nose will thank you in 3 weeks. And yes, Flonase is your new best friend.
Aurelie L.
January 29 2026
Just stop using it.
George Rahn
January 29 2026
It’s not just a medical issue-it’s a societal collapse of self-regulation. We’ve turned our bodies into machines to be tinkered with, not ecosystems to be respected. The decongestant spray is the opioid of the nasal passage: immediate gratification, delayed catastrophe. And yet, we keep reaching for it. Why? Because we’ve lost the patience to heal. We’ve forgotten that biology doesn’t operate on Amazon Prime delivery timelines. The cure isn’t in a bottle-it’s in discipline. In stillness. In surrender to the natural rhythm of the body. We don’t need more drugs-we need more reverence.
TONY ADAMS
January 31 2026
Bro I did the one nostril thing and it was wild. Left side cleared in 4 days. Right side? Still a brick wall. I kept spraying the right one ‘just a little’ and now I’m back at square one. Ugh. I hate this.
shivam utkresth
February 1 2026
As someone from India, I’ve seen this play out in clinics where people use nasal sprays for months because they can’t afford to see a doctor. The problem is even worse here-no one tells you the label says ‘3 days max.’ We’re taught to self-medicate. The fact that the FDA now mandates that warning? Long overdue. But education needs to reach the villages too, not just the urban clinics.
Uche Okoro
February 1 2026
The neurophysiological mechanisms underlying rebound congestion involve downregulation of alpha-adrenergic receptors in the nasal vasculature, compounded by increased expression of inflammatory mediators such as IL-6 and TNF-alpha. The mucosal epithelium undergoes metaplastic changes, reducing ciliary density and impairing mucociliary clearance. Consequently, the reliance on exogenous vasoconstrictors becomes a self-perpetuating feedback loop. Corticosteroids mitigate this by suppressing NF-kB signaling pathways, thereby restoring baseline vascular tone without inducing receptor desensitization.
Geoff Miskinis
February 2 2026
Let’s be real-this whole post reads like a pharmaceutical white paper. Flonase? That’s just a more expensive, slower-acting version of the same problem. You’re replacing one dependency with another. And saline? A glorified saltwater rinse. The real solution is systemic: detox your environment, reduce allergens, fix your posture, breathe through your nose. But no one wants to hear that. Too much effort. Too little profit.
eric fert
February 3 2026
Okay, but what if you’re one of those people who *only* gets congested when you’re stressed? What if your nose is just a barometer for your anxiety? You stop the spray, you breathe through your mouth, you feel better for a week, then BAM-back to square one because your cortisol levels are still through the roof. So now you’re not just addicted to a spray-you’re addicted to being a stressed-out human. And Flonase doesn’t fix that. Maybe we need to treat the mind, not just the nose.
Faisal Mohamed
February 4 2026
The capsaicin trials are fascinating. It’s essentially neural recalibration-burning the nerves just enough to reset their sensitivity. It’s like shock therapy for your sinuses. The fact that a compound from chili peppers can outperform synthetic vasoconstrictors? That’s poetic. Nature’s medicine, refined by science. I hope this becomes mainstream. We’re too obsessed with blocking symptoms. We need to rewire the system.
Rakesh Kakkad
February 5 2026
Respected sir, I have read your comprehensive exposition on the pathophysiology of rhinitis medicamentosa with profound intellectual engagement. The empirical data presented, particularly the NCBI and Mayo Clinic references, aligns with clinical observations in Indian otolaryngology practice. However, I must respectfully posit that the cultural context of self-medication in low-resource settings remains under-addressed. The socioeconomic determinants of nasal spray dependency are not merely biomedical-they are epistemic, rooted in accessibility, literacy, and the commodification of health. A public health intervention, not merely a clinical protocol, is required to dismantle this cycle at scale.
Ashley Porter
February 6 2026
I used the one-nostril trick. Took 12 days. Felt like a zombie. But now? I don’t even miss the spray. Weirdly, I feel more awake. Like my brain isn’t oxygen-deprived anymore.
SWAPNIL SIDAM
February 7 2026
Bro, I tried this last year. Stopped both sides at once. Day 3 I cried. Day 5 I almost went back. But I didn’t. Now I use saline every morning. My nose feels clean. I breathe. I sleep. It’s not magic. It’s just… work. And it’s worth it.