When you hear about colorectal polyps, it’s easy to think they’re all the same. But not all polyps are created equal. Two major types - adenomas and serrated lesions - follow very different paths to cancer, and knowing the difference can change how you’re monitored, treated, and even how often you get screened.
What Are Colorectal Polyps?
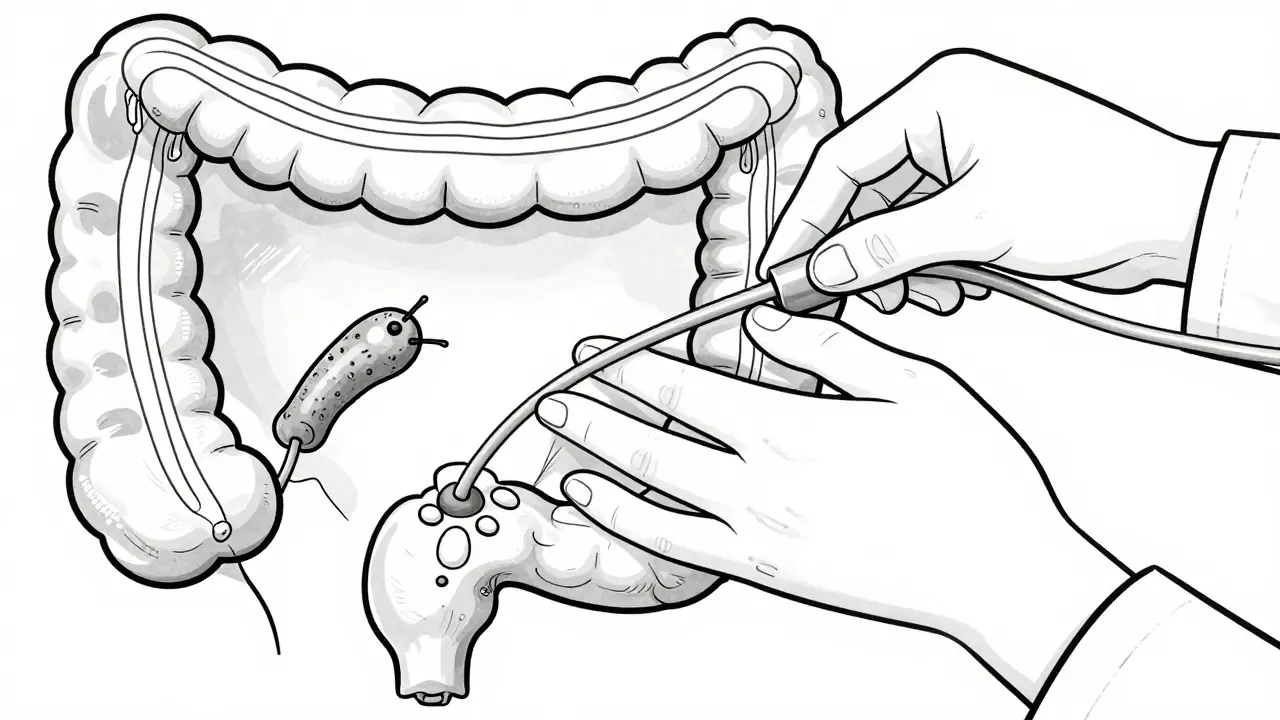
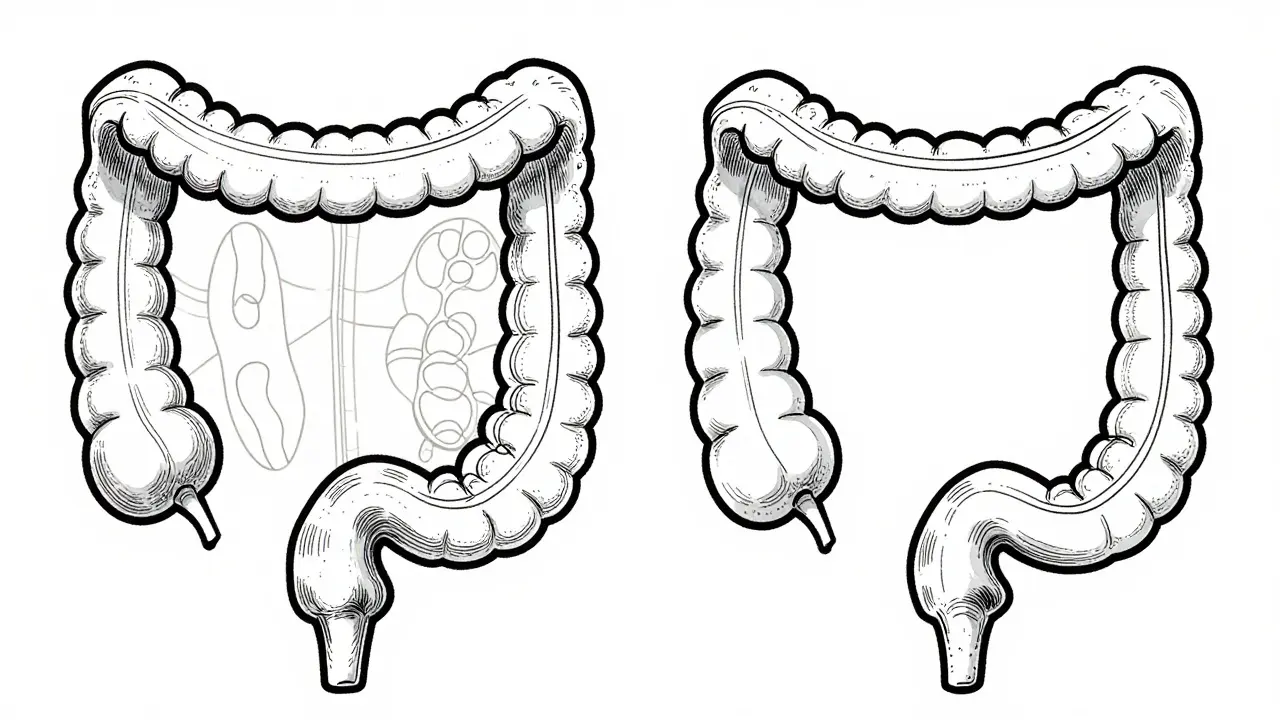
Colorectal polyps are small growths on the inner lining of your colon or rectum. About 30 to 50% of adults over 50 will develop at least one. Most don’t cause symptoms. You won’t feel them. You won’t know they’re there unless you get a colonoscopy. The big concern? Some polyps can turn into cancer over time. That’s why doctors remove them during screening. But not all polyps carry the same risk. The two main precancerous types are adenomas and serrated lesions - and they need to be treated differently.Adenomas: The Classic Precancerous Polyp
Adenomas make up about 70% of all precancerous polyps. They’re the type most doctors have been watching for decades. Under the microscope, they look like abnormal glandular tissue - think of them as misshapen versions of the normal lining of your colon. There are three subtypes:- Tubular adenomas - the most common, making up 70% of adenomas. They’re usually small and have a low risk of turning cancerous.
- Tubulovillous adenomas - about 15% of adenomas. A mix of tubular and villous features. Higher risk than tubular.
- Villous adenomas - only 15% of adenomas, but the most dangerous. They grow flat and wide, making them harder to remove completely. They carry the highest cancer risk.
Serrated Lesions: The Stealthy Pathway to Cancer
Serrated lesions are named for their saw-toothed appearance under the microscope. They account for 20-30% of all colorectal cancers - a number that surprised doctors just 20 years ago. There are three types:- Hyperplastic polyps - usually harmless, especially if they’re small and in the lower colon. Most don’t turn into cancer.
- Sessile serrated adenomas/polyps (SSA/Ps) - these are the real concern. Flat, hard to spot, and often hiding in the right side of the colon (the cecum and ascending colon). They follow a different molecular path than adenomas - driven by BRAF mutations and DNA methylation, not APC gene changes.
- Traditional serrated adenomas (TSAs) - rarer than SSA/Ps, but also precancerous. They tend to be more irregular in shape and grow faster.
Why Detection Is So Hard
Adenomas are usually raised and easy to spot during colonoscopy. Serrated lesions? Not so much. SSA/Ps are often flat or slightly elevated. They blend into the colon wall. They’re commonly found in the proximal colon - the part that’s harder to clean and see clearly. That’s why the miss rate for sessile polyps is 2-6%, even with skilled endoscopists. Magnifying colonoscopy can help. It shows distinct patterns: round or open pit structures, expanded crypt openings, and twisted blood vessels. But not every clinic has this tech. That’s why AI-assisted colonoscopy systems - like GI Genius - are changing the game. A 2021 study in The Lancet Gastroenterology & Hepatology showed these tools boost adenoma detection by 14-18%. They’re also helping catch those sneaky serrated lesions that slip through the cracks.Removal and Follow-Up
The goal is simple: remove every polyp completely. For adenomas under 2 cm, success rates are 95-98%. But for large sessile serrated lesions - especially those over 2 cm - removal success drops to 80-85%. Why? Because they’re flat, wide, and sometimes hidden under folds or mucus. After removal, surveillance isn’t one-size-fits-all.- If you had one or two small tubular adenomas, you’re usually cleared for 7-10 years.
- If you had a villous adenoma or one larger than 1 cm, you’ll need a repeat colonoscopy in 3 years.
- If you had an SSA/P that’s 10 mm or larger, U.S. guidelines say to come back in 3 years. Some European guidelines say 5 years - but the debate is ongoing.
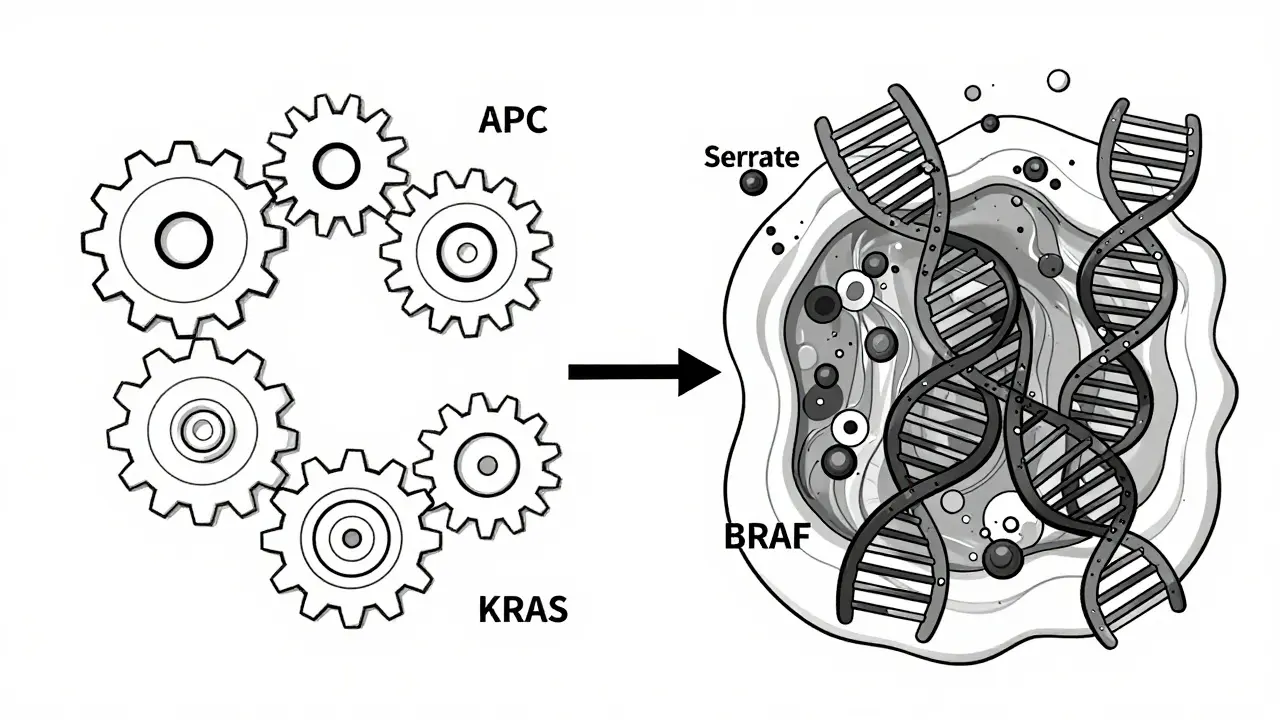
Molecular Differences Matter
Adenomas follow the chromosomal instability pathway. That means they pick up mutations in genes like APC and KRAS over time. They grow slowly, often over 10-15 years. Serrated lesions, especially SSA/Ps, follow the CpG island methylator phenotype (CIMP) pathway. They’re driven by BRAF mutations and massive DNA methylation. This pathway can skip the intermediate stages and turn cancerous faster - sometimes in as little as 5 years. That’s why researchers are now pushing for molecular testing of polyps after removal. In the next 5 years, doctors will likely use genetic markers to decide who needs a 3-year follow-up and who can wait 7. This could cut the 6.5 million surveillance colonoscopies done each year in the U.S. by 20-30%.What You Should Know
You don’t need to memorize every subtype. But here’s what you should walk away with:- Not all polyps are dangerous - but some need serious attention.
- Adenomas are common and well-understood. Serrated lesions are less common but just as dangerous - especially if they’re flat and in the right colon.
- Size, shape, and location all matter. A big, flat polyp is harder to remove and more risky than a small, stalked one.
- Screening saves lives. Removing polyps cuts colorectal cancer risk by up to 70%.
- If you’ve had a serrated polyp, stick to your follow-up schedule. Don’t skip it.
14 Comments
Doreen Pachificus
January 5 2026
Had a polyp removed last year. Didn't even know it was there until the colonoscopy. Scary how silent these things are.
Chris Cantey
January 7 2026
The real tragedy isn't the polyps-it's the system that waits for symptoms before acting. Prevention is a luxury in a healthcare economy built on intervention.
Abhishek Mondal
January 7 2026
Adenomas? Serrated lesions? Please. This is all just corporate oncology marketing dressed up as science. The real risk is overdiagnosis-colonoscopies are invasive, expensive, and often unnecessary. I’ve read the Cochrane reviews. You’re better off with a stool test and a prayer.
Oluwapelumi Yakubu
January 8 2026
Yo, this is wild-polyps are like silent ninjas in your gut. One minute you're eating tacos, next minute your colon’s hosting a cancer party. But hey, we got AI now? That’s like having a robot cop patrolling your insides. Respect. 🤖
Enrique González
January 8 2026
Screening saved my dad’s life. Don’t wait for pain. Don’t wait for bleeding. Don’t wait for anything. Just get it done. Your future self will thank you.
Ethan Purser
January 10 2026
They say ‘early detection saves lives’-but who’s really being saved? The system? The pharmaceutical companies? Or just the people who can afford $3,000 procedures with no insurance? This isn’t medicine-it’s a privilege.
Rory Corrigan
January 11 2026
SSA/Ps are the quiet killers. I had one missed during my last scope. They’re like ghosts-flat, hidden, and totally ignored until it’s too late. AI is the only reason I’m still here.
Stephen Craig
January 11 2026
Size matters. Location matters. Molecular pathway matters. But most of all, follow-up matters. Don’t skip the next colonoscopy.
Connor Hale
January 13 2026
It’s fascinating how medicine evolves. We used to treat all polyps the same. Now we know the biology behind them. That’s progress. Not perfect, but real.
Roshan Aryal
January 13 2026
Why are we still using Western guidelines in India? Our diet, our genetics, our microbiome-none of it matches your data. This is colonial medicine repackaged as science. We need our own studies, not your American polyp dogma.
Jack Wernet
January 14 2026
Thank you for this clear, thoughtful breakdown. As someone who works in public health, I appreciate how you balanced technical detail with accessibility. This is the kind of information that empowers patients.
Charlotte N
January 14 2026
So if I had a serrated polyp… does that mean I’m doomed? Or is it just… more likely? I’m confused. I mean, I got it removed right? So why are you saying I’m at higher risk? I don’t get it
Catherine HARDY
January 16 2026
AI colonoscopy? That’s just the beginning. Soon they’ll be injecting nano-bots to scan your colon while you sleep. And then-guess what?-they’ll start charging you for ‘preventive data subscriptions’. You think this is about health? It’s about control.
bob bob
January 16 2026
My buddy had a villous adenoma-big, flat, nasty. They had to do two surgeries to get it all. But he’s good now. Just got his 3-year checkup. Don’t let fear stop you. Just get it done. You’re stronger than you think.