Lisinopril Cough Assessment Tool
Assess Your Cough
Answer these questions to determine if your cough is likely related to Lisinopril and what steps to take next.
Ever wonder why your blood‑pressure pill suddenly makes you hack up a storm? You’re not alone. Lisinopril cough is one of the most common complaints, and it can be frustrating when you’re trying to stay healthy.
What is Lisinopril and how does it work?
When you first see the name Lisinopril is an oral ACE (angiotensin‑converting enzyme) inhibitor prescribed to lower high blood pressure and treat heart failure. It belongs to a class of drugs called ACE inhibitors that block the enzyme that turns angiotensin I into angiotensin II, a powerful vessel‑tightening hormone. By halting that conversion, blood vessels stay relaxed, blood pressure drops, and the heart doesn’t have to work as hard.
Why does Lisinopril sometimes trigger a cough?
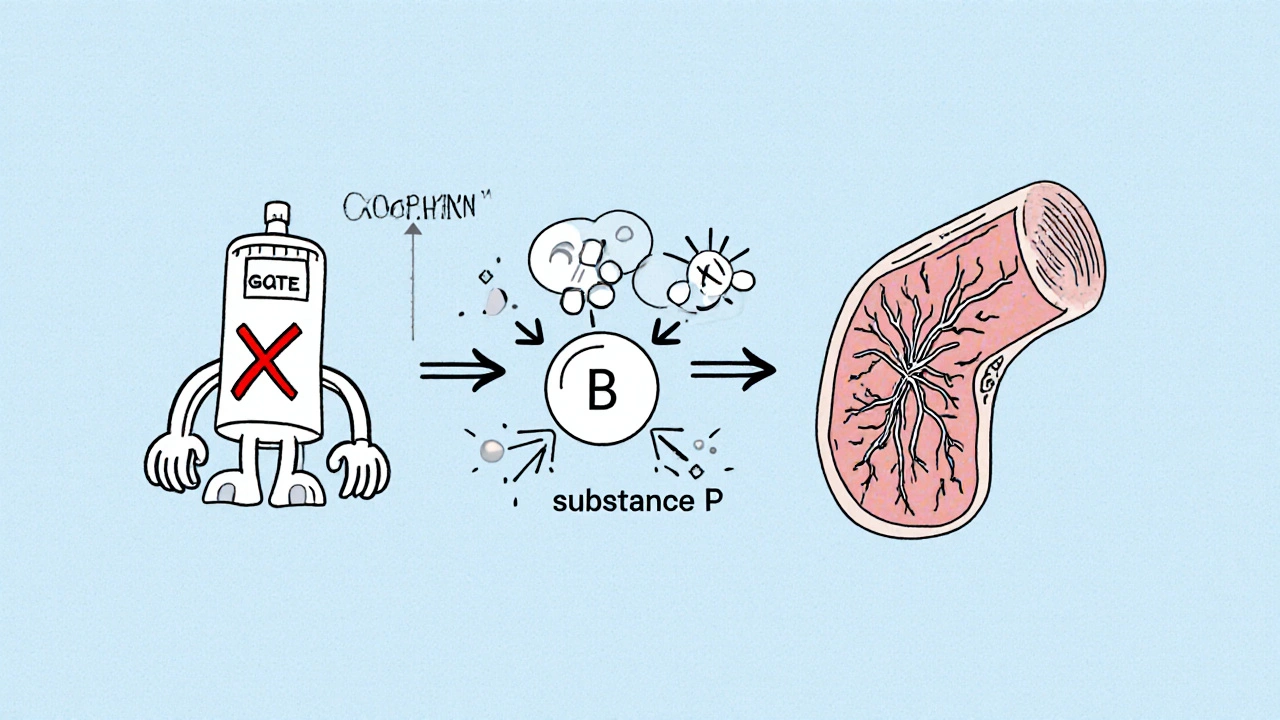
The mystery cough isn’t a random side effect - it’s tied to how ACE inhibitors interfere with a tiny peptide called Bradykinin a molecule that widens blood vessels and can irritate airway nerves when it builds up. When the ACE enzyme is blocked, bradykinin doesn’t get broken down as quickly. The extra bradykinin can stimulate the cough reflex, especially in the throat and bronchi.
Another player is the angiotensin‑converting enzyme itself, which also degrades a substance called substance P that irritates the lungs. With the enzyme out of commission, both bradykinin and substance P linger, making the airways a bit hypersensitive.
How to know if your cough is caused by Lisinopril
- Timing: The cough usually shows up weeks to months after you start the medication.
- Type: It’s typically a dry, ticklish cough that doesn’t produce mucus.
- Frequency: Many people notice the cough getting worse at night or after talking.
If you have a productive cough (with phlegm), a fever, or shortness of breath, it’s more likely an infection or another condition, and you should see a clinician right away.
Managing the cough - what you can do right now
- Stay hydrated. Warm liquids like herbal tea can soothe irritated throat tissue.
- Avoid known irritants - smoke, strong fragrances, and very cold air can make the cough louder.
- Try an over‑the‑counter cough suppressant with dextromethorphan, but only after checking with your pharmacist.
- Talk to your doctor if the cough persists beyond two weeks or disrupts sleep.
In many cases, the doctor will suggest pausing the drug for a few days to see if the cough improves. If it does, they’ll likely consider a switch.
Alternatives to Lisinopril when the cough won’t quit
If the dry cough is unbearable, the most common route is to move from an ACE inhibitor to an ARB (angiotensin‑II receptor blocker). ARBs block the same hormone downstream, so they still lower blood pressure but don’t raise bradykinin levels.
| Drug | Cough incidence | Typical dose | Key benefit |
|---|---|---|---|
| Lisinopril | 5‑20% | 10‑40 mg daily | Proven blood‑pressure control, heart‑failure benefit |
| Captopril | 8‑30% | 25‑150 mg daily | Short‑acting, useful for renal protection |
| Losartan | 1‑5% | 25‑100 mg daily | Low cough risk, good for patients with ACE‑induced cough |
Notice how ARBs like Losartan have a much lower cough rate. Switching usually involves the same dosage schedule, but always let a clinician handle the change.

Medications and habits that can worsen the cough
Some drugs interact with ACE inhibitors and make the airway irritation worse. Common culprits include:
- Ibuprofen - non‑steroidal anti‑inflammatory drugs can increase prostaglandin levels, adding to throat irritation.
- High‑dose potassium‑sparing diuretics - may raise serum potassium and cause mild airway muscle stiffness.
- Alcohol - can dry out the mucous membranes, making a tickle louder.
If you’re taking any of these, discuss timing or possible alternatives with your pharmacist.
When to seek professional help
The cough from Lisinopril is usually harmless, but there are red flags that require prompt medical attention:
- Sudden swelling of the face, lips, tongue, or throat - could signal angioedema, a rare but serious reaction.
- Shortness of breath that doesn’t improve with rest.
- Fever, chest pain, or wheezing.
These symptoms may indicate a life‑threatening allergic response. Call emergency services if you notice any of them.
Quick checklist: What to do about a Lisinopril‑related cough
- Track when the cough started and how often it occurs.
- Stay hydrated and avoid irritants.
- Use a gentle OTC suppressant only after checking with a pharmacist.
- Schedule a review with your doctor within two weeks.
- Discuss switching to an ARB like Losartan if the cough persists.
Why does a dry cough happen with Lisinopril but not with all blood‑pressure meds?
Lisinopril belongs to the ACE‑inhibitor class, which raises bradykinin and substance P levels in the lungs. Those peptides trigger the cough reflex, while other classes (like calcium‑channel blockers or ARBs) don’t affect them.
How long does the cough usually last?
If you keep taking Lisinopril, the cough can linger indefinitely. Most patients notice improvement within a few weeks after stopping or switching the medication.
Can I use a herbal remedy to calm the cough?
Gentle options like honey‑lemon tea or slippery elm lozenges can soothe the throat, but they won’t fix the underlying bradykinin buildup. Use them alongside medical advice.
Is angioedema related to the cough?
Both share the same mechanism-excess bradykinin-so if you develop facial swelling, stop the drug immediately and seek emergency care.
What are the best ARB alternatives if I need to quit Lisinopril?
Losartan and Valsartan are the most commonly prescribed. They control blood pressure effectively and have a < 5% cough incidence.

11 Comments
Eli Soler Caralt
October 21 2025
Ah, the paradox of a life‑saving drug that courts your throat into rebellion. Lisinopril, the aristocrat of ACE inhibitors, whispers promises of lower pressure while wearily hoarding bradykinin like a secret lover. 🤔 Yet the dry cough is its court jester, reminding us that even the most refined compounds have a mischievous side. If you’re chasing that celestial calm, remember the cough isn’t just a nuisance-it’s a biochemical epiphany. 🍵
Eryn Wells
November 2 2025
You’ve nailed it, Eli. While the chemistry can feel lofty, the practical takeaway is simple: stay hydrated, watch for night‑time spikes, and keep your doc in the loop. 🙌
Kathrynne Krause
November 14 2025
I was skeptical at first, but after weeks on Lisinopril I found myself hacking like a chain‑saw on a quiet night. The dryness felt like sandpaper on my vocal cords, and it totally wrecked my morning jogs. Switching to Losartan felt like swapping a broken saxophone for a smooth jazz piano. 🎷💊 If you’re battling that persistent tickle, give your throat a break and talk about an ARB with your doctor. Trust me, the relief is like a fresh breeze after a storm.
Dana Yonce
November 25 2025
Totally feel you, that sandpaper feeling is brutal. 😤 Hydration and honey‑lemon tea helped me survive the first week.
Ashok Kumar
December 7 2025
When a patient reports a stubborn dry cough after starting Lisinopril, the first step is to verify the temporal relationship between the drug initiation and symptom onset. Most clinicians will ask whether the cough appeared weeks or months after the prescription, because a delayed onset is characteristic of ACE‑inhibitor–induced cough. If the cough is dry, non‑productive, and worsens at night, it aligns with the classic presentation described in pharmacology textbooks. Conversely, a productive cough accompanied by fever or dyspnea should raise red flags for infection or heart failure rather than a medication side effect. The pathophysiology hinges on bradykinin and substance P accumulation, which sensitize the cough receptors in the upper airway. These neuropeptides are normally degraded by ACE, so inhibition leads to their buildup and the irritating tickle. Clinicians often advise patients to stay well‑hydrated, as moist mucosa can dampen the stimulus that triggers the reflex. Warm herbal teas, especially those with honey, provide both soothing warmth and a thin coating that may reduce irritation. Over‑the‑counter cough suppressants containing dextromethorphan can be used, but only after confirming there are no contraindications with the patient’s other medications. If the cough persists beyond two weeks despite these measures, the physician should consider a brief drug holiday to see if symptoms abate. A rapid improvement after stopping Lisinopril strongly suggests causality, prompting a switch to an angiotensin‑II receptor blocker. Losartan, Valsartan, and Irbesartan are popular choices because they preserve the antihypertensive effect without the bradykinin surge. Dose titration of the new ARB should mirror the former ACE inhibitor regimen to maintain blood pressure control. Patients must be educated about the low but existent risk of angioedema with any renin‑angiotensin system blocker, though it is far more common with ACE inhibitors. Finally, documenting the side effect in the medical record helps future prescribers avoid repeat exposures and contributes to pharmacovigilance data.
Jasmina Redzepovic
December 19 2025
Listen, the cough isn’t some mystical curse; it’s a textbook side effect of ACE inhibition. If you don’t want to sound like a hamster on a wheel, just switch to an ARB. Doctors who keep you on Lisinopril after weeks of coughing are basically ignoring the data. 🙄
Ivan Laney
December 30 2025
Alright, let me break this down in layman’s terms: you take Lisinopril, it blocks the conversion of angiotensin I to II, your vessels relax, blood pressure drops-great. But simultaneously it disables the enzyme that destroys bradykinin, so that peptide lingers and tickles the vagus nerve, producing the dreaded dry cough. You can try masking the symptom with honey or OTC suppressants, but that’s merely putting a band‑aid on a structural issue. The most efficient route is a swift transition to a receptor blocker, which sidesteps the bradykinin pathway entirely. In practice, a two‑day washout isn’t even necessary; physicians often cross‑titrate, ensuring continuous hypertension control while the cough fades.
Kimberly Lloyd
January 11 2026
The cough reminds us that even our bodies speak in riddles, urging us to listen before we push forward. Embracing the pause to reassess medication can be a moment of self‑care, a tiny rebellion against unnoticed discomfort. Keep your spirits up, stay hydrated, and trust that a better option awaits.
Sakib Shaikh
January 23 2026
Oh, the tragedy of a noble pill turning you into a midnight howler! 🌙💨 The airway becomes a stage, bradykinin the relentless director shouting 'Encore!' Yet the plot twist is simple: swap the script to an ARB and the curtain falls on the cough. Your throat will thank you, and the drama will end.
Devendra Tripathi
February 3 2026
While most people accept the cough as inevitable, I’d argue it’s an avoidable flaw in drug design. The industry should prioritize agents that don’t trap bradykinin.
Nick M
February 15 2026
All these meds are just Big Pharma’s way to keep us buying more.