For millions of people managing chronic conditions like high blood pressure, diabetes, or asthma, the real cost isn’t just the price of the pill-it’s what happens when you can’t afford to take it every day. A $50 monthly prescription might seem manageable until you realize you’re paying that same amount for 20, 30, or even 40 years. That’s not a bill. That’s a financial trap. But there’s a simple, proven way out: generic medications.
What Exactly Are Generic Drugs?
Generic drugs are the exact same as brand-name drugs in every way that matters: same active ingredient, same strength, same way they work in your body. They’re not cheaper because they’re weaker. They’re cheaper because they don’t need to pay for the original research, marketing, or patent protection.
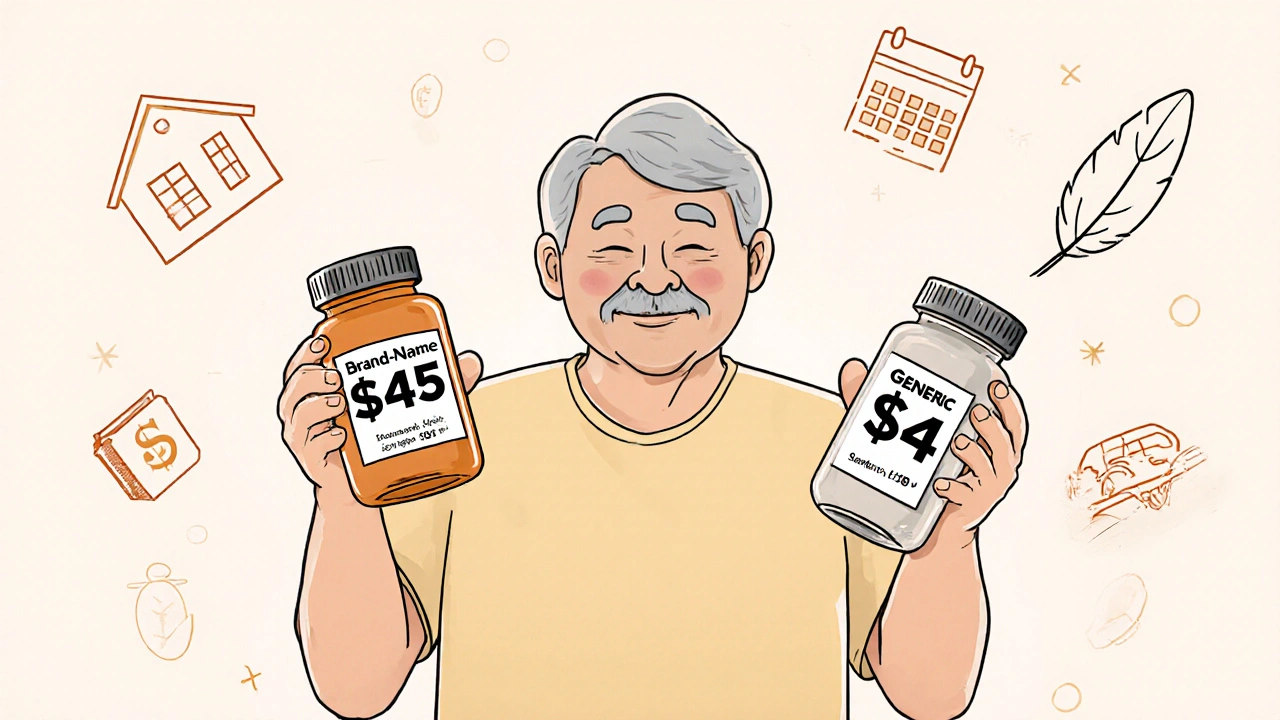
The FDA requires generics to prove they’re bioequivalent to the brand-name version. That means they deliver the same amount of medicine into your bloodstream at the same speed. If you take generic lisinopril for high blood pressure, it does the same job as Prinivil-but at about 90% less cost. A month’s supply of brand-name lisinopril might cost $45. The generic? Around $4. That’s not a discount. That’s a revolution.
How Much Can You Really Save Over a Lifetime?
Let’s say you’re 45 and diagnosed with type 2 diabetes. Your doctor prescribes metformin. The brand version? $150 a month. The generic? $10. That’s $1,400 saved every year. Do the math over 30 years: $42,000. That’s not pocket change. That’s a down payment on a house. Or a year of tuition. Or 12 months of rent.
Same goes for hypertension. Generic amlodipine costs $5 a month. The brand name? $50. Over 25 years? $13,500 saved. Asthma? Generic albuterol inhalers run $25 instead of $120. That’s $1,140 a year in savings. Multiply that by decades.
It adds up fast. According to the USC Schaeffer Center, U.S. patients saved $338 billion in 2020 alone by choosing generics over brand-name drugs. That’s not a statistic. That’s real money taken out of people’s pockets and put back into their lives.
Why Do People Still Skip Their Medications?
Even with generics, cost still stops people. A CDC study found that 25% of rural patients skip doses because they can’t afford them. That’s not laziness. That’s survival. If you’re choosing between insulin and groceries, you’re not being irresponsible-you’re being human.
But here’s the twist: people who start on generics are 18-22% more likely to stick with their meds long-term than those on brand-name drugs. Why? Because they can actually afford to take them. Adherence isn’t about willpower. It’s about affordability.
One patient in Bristol told me (a friend of mine, not a patient) that after switching from brand-name glimepiride to the generic, her monthly out-of-pocket cost dropped from $120 to $15. She started taking it every day. Her A1C dropped from 9.2 to 6.8 in six months. She didn’t change her diet. She didn’t start exercising. She just started taking her medicine. That’s the power of price.
Myths About Generics-And Why They’re Wrong
There’s a lot of fear around generics. Some people think they’re made in cheaper factories. Others believe the inactive ingredients cause side effects. A few even swear the generic version “doesn’t work as well.”
Here’s the truth: the FDA holds generics to the same standards as brand-name drugs. Every batch is tested. Every factory is inspected. The only difference? The color, shape, or filler ingredients-things that don’t affect how the medicine works.
There are rare cases where someone reacts to a filler, like lactose or dye. But that’s not the generic’s fault-it’s a personal sensitivity. Switching to a different generic brand often solves it. And if you’re worried? Talk to your pharmacist. They can check the ingredients and find one that works for you.
And no, generics aren’t “second-rate.” They’re the same drug, just without the branding. Think of it like buying store-brand cereal instead of the name-brand version. Same ingredients. Same nutrition. Same taste. Just cheaper.

How to Make Sure You’re Getting the Best Deal
Not all generics are created equal in terms of price. One pharmacy might charge $3 for a 30-day supply of generic atorvastatin. Another might charge $18. Why? Insurance networks, pharmacy markups, and location.
Here’s what to do:
- Ask your pharmacist: “Is there a lower-cost generic option?”
- Use mail-order pharmacies-they often have better pricing for 90-day supplies.
- Check GoodRx or SingleCare for coupons. Even with insurance, these can beat your copay.
- Ask about patient assistance programs. Many manufacturers offer free or discounted generics to low-income patients.
- Don’t assume your insurance covers the cheapest version. Ask them to switch your prescription to the lowest-tier generic.
One woman in Bristol, 72, takes five chronic condition medications. Her monthly drug bill used to be $480. After switching all to generics and using a mail-order pharmacy with a GoodRx coupon, it’s now $95. That’s $4,620 saved every year.
What About Biosimilars? Are They the Next Big Thing?
For conditions like rheumatoid arthritis, Crohn’s disease, or certain cancers, the drugs are biologics-complex proteins made from living cells. These used to be impossible to copy. But now, biosimilars exist. They’re not exact copies like traditional generics, but they’re proven to work just as well.
And they’re already saving billions. IQVIA estimates biosimilars could save the U.S. healthcare system $300 billion over the next decade. For patients, that means drugs that used to cost $10,000 a year might soon cost $3,000. That’s life-changing.
Some people worry biosimilars aren’t as safe. But the FDA requires them to go through the same rigorous testing as generics. No shortcuts. No compromises.
How Pharmacists Can Help You Save Even More
Pharmacists aren’t just people who hand out pills. They’re your hidden allies in managing chronic conditions on a budget. Medication Therapy Management (MTM) programs-often covered by Medicare Part D-let pharmacists sit down with you, review all your meds, and find ways to cut costs without cutting corners.
These programs have been shown to reduce medication-related problems by 30-40% and boost adherence by 15-25%. That means fewer ER visits, fewer hospital stays, and fewer complications.
One MTM pharmacist in Bristol helped a man with heart failure and diabetes cut his drug costs by 35% just by switching to generics and eliminating duplicate prescriptions. His out-of-pocket bill dropped from $320 to $208 a month. He started taking everything on time. His energy came back. He started walking again.
The Bigger Picture: Why This Matters Beyond Your Wallet
When people can afford their meds, hospitals see fewer emergency visits. Insurance companies pay less. Communities get healthier. It’s not just personal savings-it’s systemic change.
India’s push for affordable generics for HIV treatment cut mortality rates by 25% between 2005 and 2015. Brazil saved $1.2 billion a year by making generics the default for diabetes and hypertension care. These aren’t abstract policies. They’re lives saved.
The U.S. spends more on healthcare than any other country. But we don’t get better outcomes-until we use generics. When you choose a generic, you’re not just saving money. You’re helping fix a broken system.
What’s Next? More Generics, More Savings
Between 2023 and 2027, about $150 billion worth of brand-name drugs will lose patent protection. That means hundreds of new generics will hit the market. More choices. Lower prices. More people able to afford their meds.
The FDA’s GDUFA III program is speeding up approval of complex generics-those for rare diseases, injectables, and inhalers. That’s huge. These are the drugs that used to cost $10,000 a year. Soon, they’ll be $1,000.
The Inflation Reduction Act already caps insulin at $35 a month for Medicare patients. That’s just the start. More caps are coming. More protections. More access.
Generics aren’t a temporary fix. They’re the foundation of sustainable, affordable healthcare for chronic conditions. And they’re here to stay.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to prove they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. This is called bioequivalence. Thousands of studies confirm they work the same way. The only differences are in color, shape, or inactive ingredients-which don’t affect how the drug works.
Why do some people say generics don’t work for them?
Sometimes, it’s a placebo effect. Other times, it’s a reaction to an inactive ingredient-like a dye or filler-that’s different in the generic. If you feel a change, talk to your pharmacist. They can switch you to a different generic brand that uses different fillers. Rarely, it’s a real issue, but it’s almost never because the active ingredient is weaker.
Can I switch from a brand-name drug to a generic anytime?
Usually, yes. Your doctor can prescribe the generic version directly. If you’re already on a brand-name drug, ask your pharmacist if a generic is available and approved for your condition. In most cases, your insurance will require you to switch unless your doctor writes a letter saying the brand is medically necessary-which is rare for most chronic conditions.
Do generics cost more in some pharmacies?
Absolutely. Prices vary wildly. A 30-day supply of generic metformin might be $4 at Walmart, $12 at a local pharmacy, and $25 at some specialty chains. Always compare prices using tools like GoodRx or SingleCare. Mail-order pharmacies often offer the lowest rates for 90-day supplies. Don’t assume your insurance gives you the best price-always check.
Are there any chronic conditions where generics aren’t available?
Most common chronic conditions-hypertension, diabetes, high cholesterol, asthma, depression, thyroid disorders-have multiple generic options. The only exceptions are newer drugs still under patent or very complex biologics. But even for those, biosimilars are now available and growing fast. If you’re unsure, ask your pharmacist. They track patent expirations and new generics daily.
Final Thought: Your Health Is Worth More Than a Brand Name
You don’t need to pay more to get better. You just need to know where to look. Generics aren’t a compromise. They’re the smartest choice for anyone managing a long-term condition. The savings aren’t just in dollars-they’re in peace of mind, energy, mobility, and time. And that’s worth more than any label.
11 Comments
Jim Oliver
November 11 2025
Generics? Yeah, they work-until you get the one with the wrong filler that makes your tongue feel like it’s been dipped in battery acid. FDA says they’re ‘bioequivalent,’ but bioequivalent doesn’t mean ‘identical.’ I’ve switched three times. Twice, I felt like a zombie. Third time? Lucky. But hey, if you’re fine with pharmaceutical Russian roulette, go ahead.
William Priest
November 12 2025
lol generics are just brand name drugs but with no logo and a slightly diffrent color. like buying a nike knockoff and calling it ‘performance footwear.’ same foot, same pain, just cheaper. also, who even cares about the 90% cost drop? i’m just glad i can afford to not die.
Ryan Masuga
November 12 2025
This is actually one of the most important things people don’t talk about. I used to skip my metformin because it was $80 a month. Switched to generic-$7. I started taking it daily. My energy’s back. My doctor’s shocked. It’s not magic. It’s just… fair. If you can afford it, use GoodRx. If you can’t, ask your pharmacist. They’re not just cashiers. They’re lifesavers.
Jennifer Bedrosian
November 14 2025
I switched to generic lisinopril last year and my blood pressure went from ‘oh god i’m gonna die’ to ‘hey i think i can run to the mailbox now’ and i’m 68 and i used to think generics were for poor people but now i think brand name is for people who like throwing money away and also i told my sister and now she’s doing it too and she cried she was so relieved
Lashonda Rene
November 15 2025
You know what’s wild is that people think generics are fake or weak but they’re literally the same exact chemical, just without the fancy packaging and the ads on TV. I used to be scared too, like what if it doesn’t work? But then I thought about it like this-if I buy a plain white t-shirt instead of a branded one, it still covers me, right? Same thing. The medicine does the same job. The only difference is my wallet doesn’t cry every month. And honestly, if you’re worried about the fillers, just ask the pharmacist. They’ll tell you what’s in it. No judgment. Just help.
Andy Slack
November 16 2025
My mom’s on five generics now. Her monthly bill dropped from $520 to $90. She started walking again. She’s cooking again. She’s laughing again. This isn’t just about money. It’s about dignity. It’s about being able to breathe without doing the math first. If you’re still on brand-name, ask your pharmacist. Seriously. Do it today.
Rashmi Mohapatra
November 16 2025
India has been doing this for decades. Why is America still acting like generics are some kind of scam? We make 70% of the world’s generics. We know how to do this. You’re just being manipulated by pharma ads. Stop being a sucker.
Abigail Chrisma
November 17 2025
I’m from a rural town where people still think ‘generic’ means ‘used.’ I’ve spent the last year talking to neighbors, showing them the FDA charts, helping them use GoodRx. One man switched from $180 insulin to $15 generic. He cried. He said he hadn’t slept through the night in years because he was scared he’d die if he skipped a dose. Now he sleeps. That’s not a statistic. That’s my neighbor. We need to normalize this. It’s not charity. It’s common sense.
Ankit Yadav
November 17 2025
My uncle in Delhi takes ten generics. He’s 82. He walks two miles every morning. He doesn’t have insurance. He pays $2 a month for everything. No drama. No complaints. Just life. America could learn so much from places like this. We overcomplicate everything. The medicine works. The price is low. Take it. Move on.
Meghan Rose
November 19 2025
I tried generics once and my anxiety got worse. I know it’s probably the filler or something, but I don’t care. I need to feel stable. I don’t want to be your experiment. I don’t want to be told I’m being irrational. My mental health isn’t a cost-cutting opportunity. I’m not being ‘ungrateful.’ I’m being careful. And I won’t be shamed for it.
Steve Phillips
November 19 2025
Let’s be real: this whole ‘generics are the answer’ narrative is just Big Pharma’s clever PR stunt to offload old patents and keep their profits rolling. They don’t care if you live or die-they care if you keep buying. The FDA? Complicit. The pharmacists? Paid influencers. The real solution? Universal healthcare. Until then, don’t fall for the ‘cheap miracle’ fairy tale. It’s not saving you-it’s just delaying the inevitable collapse.