What is hepatic encephalopathy?
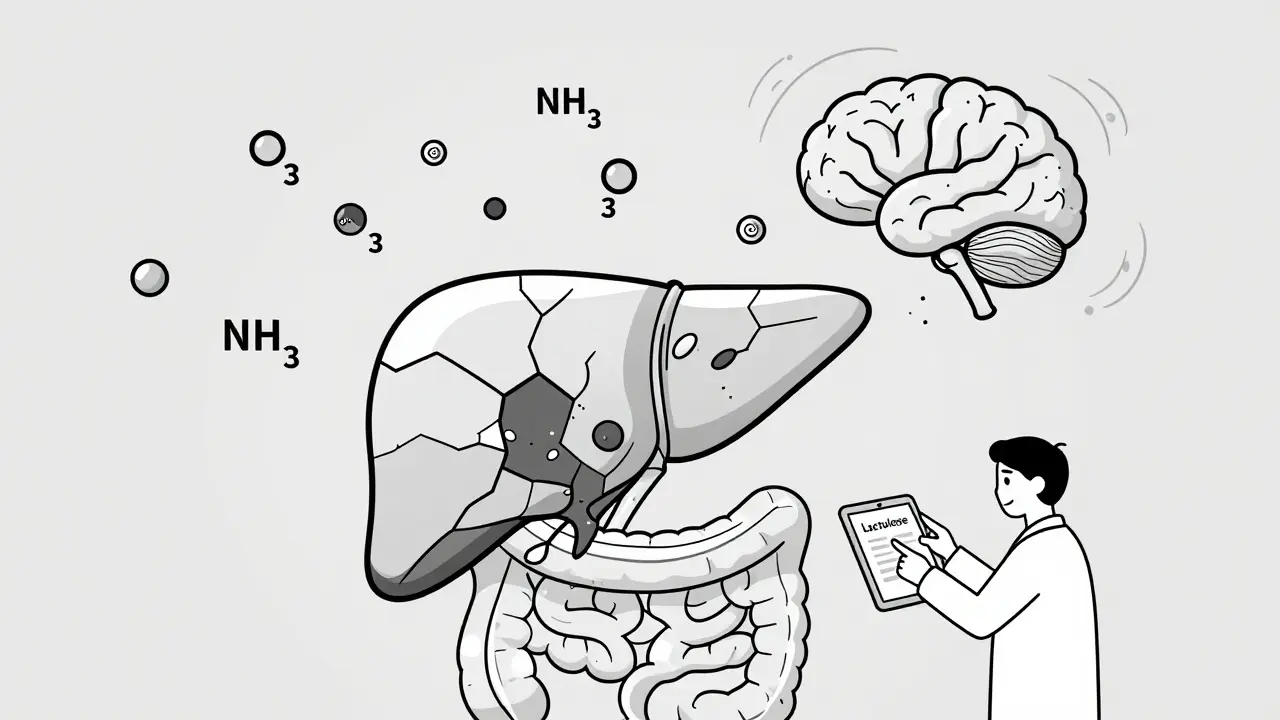
Hepatic encephalopathy is a brain disorder caused by advanced liver disease, where toxins-especially ammonia-build up in the blood because the liver can’t filter them out. This isn’t just about feeling tired. It’s when your brain starts to malfunction because your liver is failing to do its job.
People with cirrhosis are most at risk. About 30 to 45% of them will develop noticeable symptoms at some point. But even before the confusion shows up, up to 80% of cirrhotic patients have subtle brain changes only special tests can catch. These early signs are called minimal hepatic encephalopathy. You might not notice them yourself, but your memory, attention, or reaction time could be slower.
Why does confusion happen with liver disease?
The liver normally cleans ammonia from your blood. Ammonia comes from bacteria in your gut breaking down protein. When the liver is damaged, ammonia slips through and heads straight to your brain. That’s when things go wrong.
Ammonia doesn’t just make you sleepy. It causes brain cells to swell, messes with neurotransmitters, and triggers inflammation. The result? Mild confusion, forgetfulness, trouble focusing, personality shifts, or even slurred speech. In severe cases, people slip into coma. These symptoms can come on suddenly after a trigger-like an infection, bleeding in the gut, or too much protein-or creep up slowly over weeks.
What’s surprising? Ammonia levels in the blood don’t always match how bad the confusion is. Some people with high ammonia feel fine. Others with normal levels are very confused. That’s why doctors don’t rely on ammonia tests alone. They look at your liver function, your symptoms, and rule out other causes like strokes or infections.
How is lactulose used to treat hepatic encephalopathy?
Lactulose is a synthetic sugar that’s been the first-line treatment for hepatic encephalopathy since the 1960s. It’s not a cure, but it’s the most proven way to reverse symptoms quickly.
Lactulose works in three ways. First, it pulls water into your colon, making you poop more. Second, it makes your gut more acidic. That change turns ammonia (NH₃) into ammonium (NH₄⁺), a form your body can’t absorb. Third, it helps flush out ammonia through your stool.
Doctors usually start with 30 to 45 mL, taken three or four times a day. The goal isn’t to cause diarrhea-it’s to get two to three soft bowel movements every day. Too little, and it won’t work. Too much, and you’ll be stuck in the bathroom. Many patients say the taste is awful and the cramping is rough. But for many, it’s the difference between staying out of the hospital and ending up in intensive care.
Some people get lactulose as a rectal enema if they’re too confused to swallow. That’s common in acute cases. In one study, 65% of people who didn’t improve were simply getting too low a dose. The key? Dosing it right-and sticking with it.

What’s rifaximin, and why is it added to lactulose?
Rifaximin is an antibiotic that doesn’t get absorbed into the bloodstream. Instead, it stays in the gut to kill ammonia-producing bacteria.
It’s not used alone. It’s added to lactulose when someone keeps having flare-ups. The RIFHE study showed it cuts recurrent episodes by 58% compared to placebo. It’s taken as two 550 mg pills daily. For many, it’s a game-changer. One patient on a liver forum said, “After six months of lactulose and rifaximin, I went back to part-time work.”
But it’s expensive-around $1,200 a month. And there’s a small risk: about 1 in 500 people get Clostridium difficile diarrhea from it. Still, for people who’ve had multiple hospital stays, the benefit usually outweighs the cost and risk.
What triggers hepatic encephalopathy flare-ups?
Many episodes don’t come out of nowhere. They’re triggered. And knowing the triggers is half the battle.
- Infections: Spontaneous bacterial peritonitis (infection in the belly fluid) causes 25-30% of HE episodes.
- Bleeding: A bleeding ulcer or varices in the esophagus can dump protein into the gut, feeding ammonia-producing bacteria. This triggers 20-25% of cases.
- Electrolyte imbalances: Low potassium or dehydration makes the liver work harder and ammonia harder to clear. That’s 15-20% of cases.
- Constipation: If you’re not pooping regularly, ammonia builds up. Lactulose helps here too.
- Medications: Benzodiazepines (like Valium or Xanax) make HE 3.2 times more likely. Even over-the-counter sleep aids can be dangerous.
- UTIs and other hidden infections: One caregiver noticed her husband’s confusion always came after a urinary tract infection. Monthly testing stopped 80% of his episodes.
That’s why doctors ask: “Did you have a fever? Did you bleed? Did you miss your diuretics?” It’s not just about the liver-it’s about the whole body.
How do you prevent hepatic encephalopathy?
Prevention is smarter-and cheaper-than waiting for a crisis.
First, take lactulose daily if you’ve had HE before. A study showed prophylactic use (15 mL twice daily) cuts recurrence by 50% in six months. Don’t wait until you’re confused to start it.
Second, watch your protein. You don’t need to starve yourself. In fact, too little protein weakens your muscles and makes recovery harder. During a flare-up, cut back to 0.5 grams per kilogram of body weight. Once you’re stable, go back to 1.2-1.5 grams per kilogram. That’s about 70-90 grams a day for most adults-enough for eggs, fish, beans, and lean meat.
Third, avoid alcohol and sedatives. Even small amounts can trigger a flare. And never take sleeping pills or anti-anxiety meds without checking with your liver specialist.
Fourth, track your bowel movements. If you’re not having two to three soft stools a day, your lactulose dose needs adjusting. Keep a simple log: date, number of stools, consistency.
Fifth, get vaccinated. Hepatitis A and B shots, the pneumococcal vaccine, and the flu shot all reduce infection risks that can trigger HE.
What if lactulose doesn’t work?
Not everyone responds. About 20-30% of patients don’t improve with standard treatment. When that happens, doctors look for hidden causes.
Maybe it’s not HE at all. Could it be kidney failure? A brain tumor? An undiagnosed infection? One patient was misdiagnosed with dementia for two years before someone realized it was HE.
Or maybe the lactulose dose is too low. As mentioned, 65% of non-responders were on less than 30 mL per day. Sometimes, you need 90 mL or more.
Other options include:
- L-ornithine-L-aspartate (LOLA): A supplement that helps the liver process ammonia. Studies show it improves mental clarity in about 35% of patients.
- Fecal microbiota transplant (FMT): Transplanting healthy gut bacteria from a donor. In trials, it lowered ammonia in 70% of people who didn’t respond to drugs.
- AST-120: An oral adsorbent used in Japan since 2005. It binds toxins in the gut before they’re absorbed. Recently approved in Europe.
- SYN-004 (ribaxamase): A new drug in development that breaks down antibiotics in the gut to protect good bacteria. Early results show a 35% drop in HE episodes.
Research is moving fast. A new blood test, being tested by Virginia Commonwealth University, could predict HE risk with 85% accuracy using 12 biomarkers. And smartphone apps like EncephalApp can track subtle brain changes before symptoms get bad.
What does life look like after a diagnosis?
Living with hepatic encephalopathy isn’t easy, but it’s manageable. Many people go back to work, drive, and live independently-if they stick to the plan.
Family support is huge. In one survey, 65% of HE episodes were noticed by family members before the patient realized anything was wrong. That’s why caregivers need to learn the signs: slurred speech, forgetfulness, personality changes, or odd behavior.
And yes, it’s isolating. 42% of patients say they’ve withdrawn from social life because they’re embarrassed or afraid of having a flare-up in public. But with good treatment, many regain their confidence.
One man in Bristol told his doctor: “I used to forget my wife’s birthday. Now I take my lactulose every morning, and I remember everything.”
What’s the future of hepatic encephalopathy treatment?
The future is personal. Researchers are no longer treating HE as one condition. They’re starting to see subtypes: some driven by gut bacteria, others by inflammation, others by brain sensitivity.
Next-gen drugs are coming. Non-antibiotic alternatives to rifaximin are in Phase 3 trials. Smartwatches that monitor reaction time and speech patterns could alert you to a flare before it happens. And with the NIH funding a $5.2 million project to map the gut-liver-brain axis, we’re closer than ever to predicting and preventing HE before it starts.
Right now, the best tool is still lactulose-cheap, proven, and effective when used right. But the next decade will bring more precision, less trial and error, and fewer hospitalizations.
Can hepatic encephalopathy be reversed?
Yes, in most cases. If caught early and treated properly, symptoms like confusion, sleepiness, and personality changes can fully improve. Lactulose and rifaximin often restore mental clarity within days. But if liver damage is severe and untreated, HE can progress to coma or death. The key is early action and consistent treatment.
Does lactulose cause diarrhea?
It can, but it shouldn’t. Lactulose is meant to cause two to three soft stools per day-not watery diarrhea. If you’re having more than that, your dose is too high. Too few stools mean it’s not working. The goal is balance. Adjust the dose under your doctor’s guidance. Many people learn their sweet spot after a few weeks.
Is hepatic encephalopathy the same as dementia?
No. Dementia is progressive and irreversible, caused by brain cell death from Alzheimer’s or other neurodegenerative diseases. Hepatic encephalopathy is a reversible brain dysfunction caused by liver failure. Symptoms can look similar-memory loss, confusion-but HE improves with treatment. Many people are misdiagnosed with dementia before their liver disease is recognized.
Can I eat protein if I have hepatic encephalopathy?
Yes-but carefully. During a flare-up, your doctor may temporarily reduce protein to 0.5 grams per kilogram of body weight. Once you’re stable, you need 1.2-1.5 grams per kilogram to maintain muscle and strength. Plant-based proteins (beans, lentils) and dairy are often better tolerated than red meat. Never cut protein long-term without medical advice.
How do I know if my lactulose dose is right?
You should have two to three soft, non-watery bowel movements every day. If you’re having fewer, increase the dose by 15 mL every day until you reach that goal. If you’re having diarrhea or cramps, lower it. Keep a log for a week and bring it to your doctor. Most treatment failures happen because people are on too low a dose-not because the drug doesn’t work.
Can I stop taking lactulose if I feel better?
No. Hepatic encephalopathy is a chronic condition if you have cirrhosis. Stopping lactulose-even if you feel fine-raises your risk of a severe flare-up. Most people need to take it long-term. Prophylactic use cuts recurrence by half. Think of it like blood pressure medicine: you take it to stay well, not just when you feel sick.
13 Comments
Herman Rousseau
December 21 2025
This is the kind of post that saves lives. Lactulose isn't glamorous, but it's the unsung hero of liver care. I've seen patients go from confused and withdrawn to driving themselves to appointments just by getting the dose right. Don't underestimate the power of two to three soft poops a day. It's not sexy, but it's science.
And yes - if you're on rifaximin, stick with it. The cost sucks, but so does spending a week in the ICU because you thought you could skip a dose.
Ajay Brahmandam
December 23 2025
I’ve been managing HE for 5 years. My trick? I keep a little notebook. Date, stool count, how sharp I felt that day. After a month, I saw patterns. Missed my lactulose? Foggy by noon. Ate too much steak? Slurred speech by dinner. It’s not magic - it’s data.
Johnnie R. Bailey
December 23 2025
Let’s talk about the elephant in the room: protein fear. I used to tell my patients to eat tofu, eggs, and Greek yogurt - not because they’re ‘liver-friendly’ but because muscle wasting kills faster than ammonia. You don’t need to starve. You need to strategize. Plant proteins are easier on the gut, and dairy gives you glutamine without the ammonia spike. And yes, you can still have a chicken breast. Just don’t eat six of them at once.
Jeremy Hendriks
December 24 2025
The system is broken. Big Pharma pushes expensive drugs while the real solution - lactulose - costs pennies. Why? Because nobody gets rich selling a syrup that makes you poop. We’re treating symptoms, not the profit model. This isn’t medicine. It’s capitalism with a stethoscope.
jenny guachamboza
December 25 2025
I think this whole HE thing is a scam. I read on a forum that the liver doesn’t even make ammonia - it’s all from 5G towers and GMO soy. My uncle stopped taking lactulose and now he’s ‘energized’ - he says the ‘truth’ set him free. 🌱🌀
Candy Cotton
December 25 2025
I find it deeply concerning that this article casually endorses fecal transplants without addressing the ethical implications of sourcing donor material from individuals with unverified medical histories. The FDA has issued warnings. This is not a DIY procedure.
Tarun Sharma
December 26 2025
The dosage guidance is accurate. Two to three soft stools daily is the target. Many patients misunderstand this as a requirement for diarrhea. It is not. Consistency matters more than frequency.
Art Van Gelder
December 27 2025
You know what’s wild? We’ve been treating hepatic encephalopathy like it’s a broken pipe - just flush the ammonia out. But what if the problem isn’t the pipe? What if it’s the whole damn plumbing system? The gut microbiome isn’t just a bystander - it’s the foreman. And we’ve been firing it with antibiotics while ignoring the blueprint. Rifaximin helps, sure. But FMT? That’s not medicine. That’s a reset button. And honestly? I think we’re going to look back at lactulose the way we look at bloodletting. Just a stopgap while we wait for the real cure - the one that reprograms the gut-brain axis, not just flushes it.
Jim Brown
December 27 2025
The metaphysical implications of hepatic encephalopathy are profound. The liver, traditionally regarded as the seat of courage in classical humoral theory, is now revealed as the silent architect of cognition. When it falters, the mind does not merely falter - it dissolves into the chemical fog of its own betrayal. To treat HE is not merely to administer lactulose, but to reconcile the body’s silent rebellion against its own decay. We are not treating a disease; we are negotiating with mortality.
Vikrant Sura
December 28 2025
Eh. It's all just hype. People get confused because they're old or drunk. Lactulose is just a laxative. Why are we making this so complicated?
Kathryn Weymouth
December 30 2025
I appreciate the thoroughness of this post, particularly the clarification between HE and dementia. Too often, families are told their loved one has Alzheimer’s when it’s actually reversible liver dysfunction. Early detection saves not only cognition but also dignity.
Julie Chavassieux
December 31 2025
I’ve seen this before. Someone’s grandmother starts forgetting names, then they say it’s HE. But what if it’s just aging? What if it’s depression? What if it’s the meds? You’re making this sound like a diagnosis you can just Google. It’s not. It’s complex. And you’re oversimplifying.
Sai Keerthan Reddy Proddatoori
January 1 2026
America thinks it can fix everything with pills. In India, we know the truth: the liver heals with clean food, no sugar, no alcohol. Why are you paying $1200 for a pill when your grandpa used to drink neem water? This is cultural surrender.