Anticholinergic Burden Calculator
How This Works
Select medications you're taking. Each has a score (0-3) based on anticholinergic strength. Total score indicates your risk level:
- Score 0-1 Low Risk
- Score 2 Moderate Risk
- Score 3+ High Risk
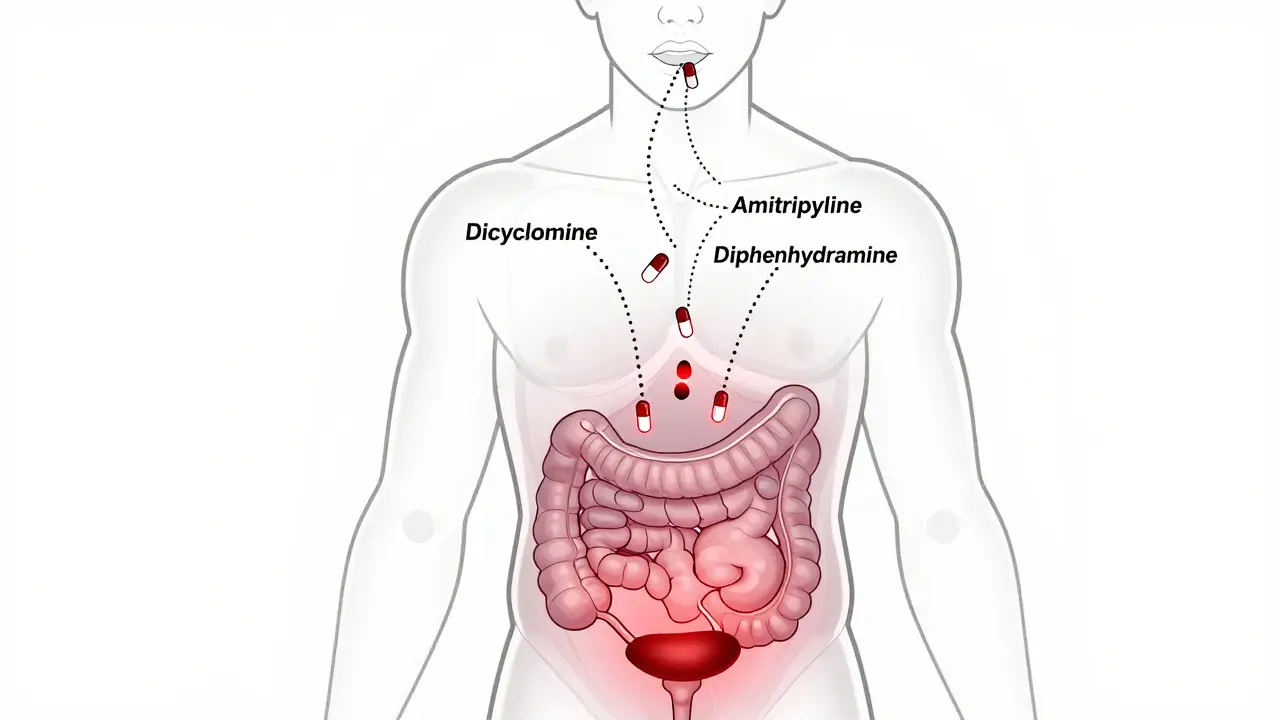
When you take an antispasmodic like dicyclomine or hyoscine for stomach cramps or irritable bowel syndrome, you might not realize you’re also taking a drug that can clash dangerously with other medications you’re already on. These drugs work by blocking acetylcholine - a chemical your body uses to control muscle contractions in the gut, bladder, and even your eyes. But when that same chemical is also being blocked by other pills you’re taking - like allergy meds, antidepressants, or sleep aids - things can go wrong fast.
How Anticholinergic Antispasmodics Work
Anticholinergic antispasmodics like dicyclomine and hyoscine stop muscles from spasming by blocking muscarinic receptors. These receptors normally get activated by acetylcholine to make your intestines contract, your bladder empty, or your salivary glands produce saliva. When you take these drugs, you get relief from cramps - but you also get side effects like dry mouth, constipation, blurred vision, and trouble urinating. These aren’t just annoyances. They’re signs the drug is working - and also signs it’s affecting more than just your gut.
The problem isn’t just the drug itself. It’s what happens when you add another anticholinergic on top. Many common medications have the same mechanism. Amitriptyline for nerve pain. Diphenhydramine (Benadryl) for allergies. Oxybutynin for overactive bladder. Even some antipsychotics and Parkinson’s meds. Each one adds to the total anticholinergic load in your body. It’s like turning up the volume on the same warning signal over and over - until it becomes a scream.
Common and Dangerous Interactions
One of the most frequent and dangerous combinations is antispasmodics with antidepressants. A patient on dicyclomine for IBS might be prescribed amitriptyline for chronic pain. Both are anticholinergic. Together, they can cause severe constipation, urinary retention, confusion, and even delirium - especially in older adults. One user on Drugs.com reported that after starting amitriptyline, their dicyclomine stopped working and they became constipated for weeks. That’s not a coincidence. It’s additive toxicity.
Another risky mix: antispasmodics with over-the-counter sleep aids or allergy pills. Diphenhydramine, doxylamine, and chlorpheniramine are all strong anticholinergics. Taking them with hyoscine or oxybutynin can lead to extreme drowsiness, dizziness, and impaired thinking. A Reddit pharmacist shared that in just one month, they had to step in on three cases where patients were prescribed multiple anticholinergic drugs by different doctors - none of them knew the risks.
Even something as simple as an antihistamine for a cold can turn a manageable side effect into a medical emergency. Older adults are especially vulnerable. The American Geriatrics Society Beers Criteria® lists dicyclomine and oxybutynin as potentially inappropriate for people over 65 because of their high anticholinergic burden. Studies show that when people over 65 take three or more anticholinergic drugs, their risk of dementia increases by up to 50% over 10 years.

Why This Is Getting Worse
It’s not just about pills you take on purpose. Many people don’t realize they’re taking anticholinergic drugs at all. Cold medicines, motion sickness patches, even some skin creams contain anticholinergic ingredients. A 2023 study in JAMA Internal Medicine found that 43% fewer harmful combinations occurred when doctors used a digital tool that flagged anticholinergic interactions in real time. That tool - the University of Washington’s Anticholinergic Burden Calculator 2.0 - now integrates with major electronic health records. It scores every medication on a scale of 0 to 3 based on how strong its anticholinergic effect is. A score above 2 means you’re at high risk.
Doctors used to prescribe these drugs without thinking twice. Now, guidelines from the American Gastroenterological Association say 68% of gastroenterologists avoid anticholinergic antispasmodics as first-line treatment. They’re switching to alternatives like peppermint oil capsules, calcium channel blockers (like cinnarizine), or even low-dose SSRIs - all with fewer interaction risks.
What You Should Do
If you’re taking an antispasmodic, here’s what you need to do right now:
- Make a full list of every medication you take - including OTC pills, supplements, and patches. Don’t forget the sleep aid you take once a week or the allergy pill you use in spring.
- Check each one on the Anticholinergic Burden Scale. You can find the list online through the University of Washington or ask your pharmacist. Medications like amitriptyline, oxybutynin, and diphenhydramine are all high-risk.
- Add up the score. If your total is 2 or higher, talk to your doctor. You might not need all of them.
- Ask about alternatives. Is there a non-anticholinergic option for your cramps? Peppermint oil has been shown in trials to be as effective as dicyclomine for IBS - with zero anticholinergic effects.
Don’t wait for symptoms to get bad. Dry mouth? Constipation? Blurry vision? Confusion? These aren’t just side effects. They’re warning signs your body is overloaded. One study found that 69% of patients on high-dose dicyclomine (160 mg/day) had adverse events - compared to just 16% on placebo. That’s not normal. That’s a red flag.
The Future Is Changing
Prescriptions for anticholinergic antispasmodics have dropped 22% since 2018. Meanwhile, non-anticholinergic options are up 37%. Why? Because doctors are finally seeing the cost. These drugs aren’t just risky - they’re outdated. Newer agents in Phase III trials are designed to act only in the gut, not the brain. That means they can stop cramps without causing confusion or memory problems.
Regulators are catching up too. The European Medicines Agency now requires all anticholinergic antispasmodic packaging to warn about interactions with CNS depressants. The FDA has boxed warnings for use in glaucoma, myasthenia gravis, and urinary blockage - especially when combined with MAO inhibitors.
By 2027, experts predict less than 20% of antispasmodic prescriptions will be anticholinergic. They’re not disappearing - but they’re becoming niche. Used only when absolutely necessary, and only after every other option has been tried.
Final Advice
If you’re on an antispasmodic, don’t assume it’s safe just because your doctor prescribed it. Many of these drugs were approved decades ago, before we understood how dangerous polypharmacy can be. Your pharmacist is your best ally here. Bring your full med list to every appointment. Ask: "Is this drug adding to my anticholinergic load?" If the answer is yes, ask: "Is there a safer way to get the same result?"
The goal isn’t to stop treatment. It’s to stop unnecessary risk. There are better, safer ways to manage cramps and spasms today. You don’t have to live with dry mouth, confusion, or constipation just because you were prescribed an old-school drug. Ask questions. Push for alternatives. Your brain and your gut will thank you.
8 Comments
Cassandra Collins
December 15 2025
lol so now even my grandma's benadryl is gonna kill me?? i swear the pharma companies are just poisoning us slowly so we gotta buy more meds for the side effects they made up. they dont want you healthy they want you hooked. 🤡
Dylan Smith
December 15 2025
Ive been on dicyclomine for 8 years and never realized how many other things in my cabinet were adding to the load. My sleep aid my allergy pills even that motion sickness patch i keep in my glovebox. All of them. I just checked the uw calculator and im at 4. Thats insane. I need to talk to my doc tomorrow
Mike Smith
December 17 2025
This is an exceptionally well-researched and clinically vital post. The aggregation of anticholinergic burden is one of the most underappreciated iatrogenic risks in geriatric and polypharmacy populations. The 50% increased dementia risk over a decade is not merely statistical-it is a public health emergency. I urge all clinicians to implement the University of Washington calculator as standard practice. Patient safety must precede convenience.
Ron Williams
December 17 2025
I work in a pharmacy and see this every week. Someone comes in with a script for oxybutynin and then pulls out three OTC meds from their bag-Benadryl, NyQuil, and that weird sleep gummy with diphenhydramine. We have to sit them down and explain why their brain feels like mush. It’s not their fault. The system’s broken. But at least now we have tools to fix it.
Kitty Price
December 17 2025
peppermint oil changed my life 🌿 no more dry mouth no more brain fog just chill vibes and happy gut. i told my dr and she was like 'oh yeah weve been pushing that for years' why didnt anyone tell me sooner??
Colleen Bigelow
December 18 2025
This is all part of the globalist medical elite’s plan to control our bodies. They want you dependent on their drugs so you’ll never question the system. The real cure for IBS is fasting and prayer. They banned the ancient remedies because they don’t make money off them. You think your doctor cares about you? They get paid per script. Wake up. The FDA is just a front for Big Pharma. I’ve seen the documents.
Billy Poling
December 20 2025
It is imperative to recognize that the escalation of anticholinergic burden is not merely a pharmacological concern but a systemic failure in prescriptive oversight. The proliferation of polypharmacy, particularly in the context of fragmented healthcare delivery, has resulted in a dangerous normalization of additive toxicity. The absence of mandatory interaction screening protocols across electronic health record platforms constitutes a critical regulatory gap. Furthermore, the commercialization of over-the-counter anticholinergic agents without adequate consumer education represents a profound ethical lapse. A standardized national anticholinergic burden dashboard, integrated into all prescription and OTC labeling, should be enacted immediately.
Souhardya Paul
December 21 2025
I’m a GP and I’ve started using the UW calculator in every med review now. One patient was on amitriptyline, oxybutynin, and diphenhydramine for sleep. Total score: 6. She was confused all day. We switched her to cinnarizine and melatonin. Within two weeks she was lucid, sleeping better, and her constipation was gone. It’s not about taking drugs away-it’s about replacing them with smarter ones. This isn’t radical. It’s just good medicine.