What’s Really Happening When Your MS Symptoms Flare Up?
You wake up with blurred vision. Your leg feels heavy. You can’t hold a cup steady. It feels like another relapse-another step backward. But what if it’s not? What if your body isn’t having a new attack, but just reacting to something simple, like a hot shower or a urinary infection? This confusion is more common than you think. In fact, up to one in four people with MS mistake a pseudorelapse for a real relapse. And the consequences? Unnecessary steroids, hospital visits, and even serious side effects like mood swings, high blood sugar, or worse.
True relapses and pseudorelapses look almost identical on the surface. Both involve sudden worsening of old symptoms or new ones. But underneath? They’re completely different. One is inflammation attacking your nervous system. The other is your damaged nerves temporarily failing under stress. Mixing them up doesn’t just waste time-it puts your health at risk.
What Exactly Is a True MS Relapse?
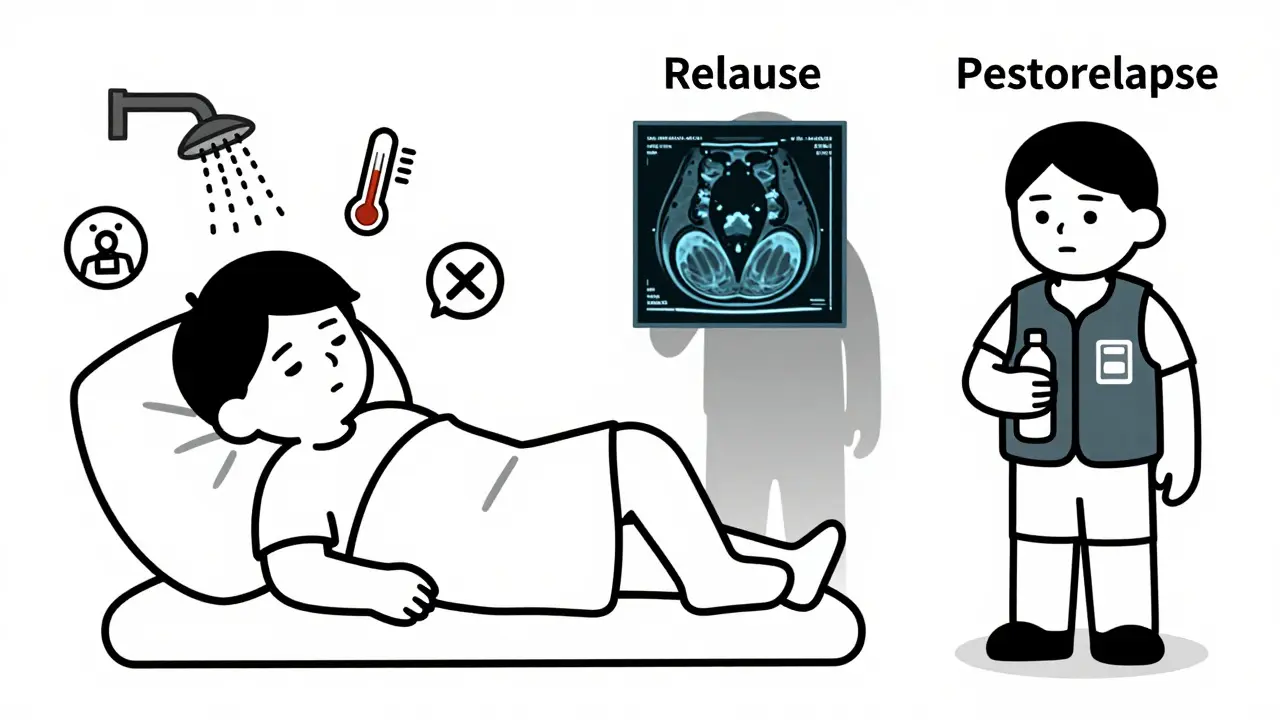
A real MS relapse means your immune system has launched a new attack on your central nervous system. It’s not just feeling tired or overheated. It’s actual inflammation causing new damage-new lesions forming on your brain or spinal cord. These attacks cause symptoms that last at least 24 to 48 hours, often longer. They can include sudden weakness, loss of balance, vision problems, numbness, or trouble urinating. And they don’t come from outside triggers like fever or heat.
When a true relapse happens, an MRI usually shows new or active lesions. That’s the smoking gun. It confirms that your immune system is actively destroying myelin-the protective coating around your nerves. These relapses can leave behind lasting damage. Each one increases your risk of long-term disability, especially if they happen often or are severe.
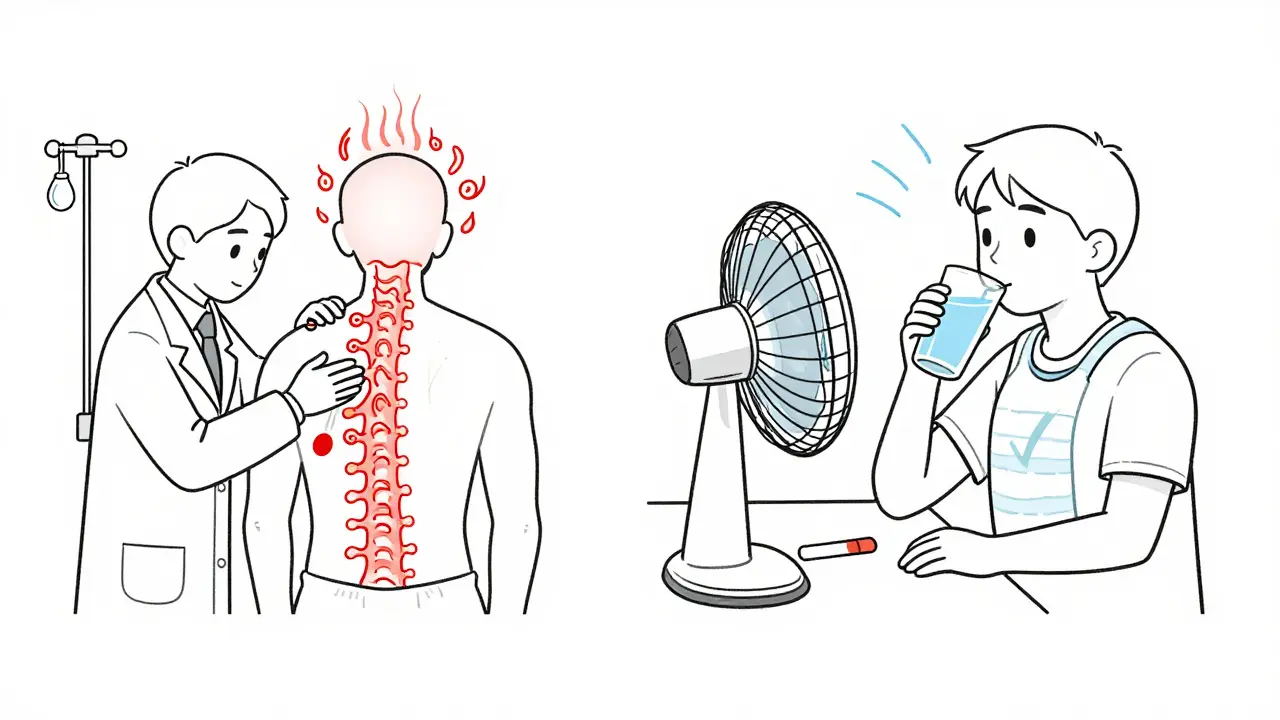
Treatment? High-dose steroids, usually given through an IV over 3 to 5 days. Methylprednisolone is the go-to drug. It doesn’t cure anything, but it can speed up recovery by calming the inflammation. About 70 to 80% of people see some improvement. But only about half fully bounce back. That’s why doctors only use steroids when symptoms are truly disabling-like when you can’t walk, your bladder stops working, or your vision is gone.
What Is a Pseudorelapse? (And Why It’s Not a Relapse)
A pseudorelapse-sometimes called a pseudoexacerbation-isn’t inflammation. It’s not new damage. It’s your existing nerve damage acting up because something in your body has changed. Think of it like a frayed wire that works fine until it gets too hot or wet. Suddenly, it shorts out. But once you fix the heat or moisture, it works again.
These episodes last less than 24 hours. Symptoms fade fast once the trigger is gone. No new lesions appear on MRI. No immune system activity. Just your nervous system temporarily struggling under pressure.
Common triggers? Here’s what actually causes most pseudorelapses:
- Heat-Hot showers, sunny days, exercise, even a fever. Up to 41% of people with MS report heat as their main trigger. This is called Uhthoff’s phenomenon. If you’ve had optic neuritis before, you’re especially likely to notice your vision blur when you get warm.
- Infections-Urinary tract infections (UTIs) are the #1 trigger, causing 67% of pseudorelapses. Colds, flu, and even a mild sinus infection can do it too.
- Stress-Emotional or physical stress can raise your body’s cortisol and adrenaline, which can make nerve signals stutter.
- Metabolic changes-Low sodium, high blood sugar, or dehydration can mess with how nerves fire.
- Physical overexertion-Pushing too hard during rehab or daily tasks can overload damaged nerves.
Here’s the kicker: you don’t need steroids for any of this. In fact, giving them to someone having a pseudorelapse is like using a sledgehammer to fix a loose screw. It doesn’t help-and it can hurt.
Why Steroids Don’t Work for Pseudorelapses (And Why They’re Dangerous)
Steroids work by suppressing inflammation. But pseudorelapses have no inflammation. So steroids do nothing to fix the real problem-heat, infection, stress. All they do is flood your body with synthetic hormones.
Studies show that 30 to 40% of people with MS get unnecessary steroid treatments because their pseudorelapse was mistaken for a true relapse. And the side effects? They’re real:
- 25% develop high blood sugar-even if they’ve never had diabetes before.
- 40% can’t sleep.
- 30% feel anxious, irritable, or even depressed.
- Some get mood swings so bad they end up in psychiatric care.
- Your immune system gets weaker, making you more likely to catch the next infection.
One nurse with MS on Reddit shared a story about five patients she saw in a year who got IV steroids for UTIs. One developed steroid-induced psychosis and had to be hospitalized. That’s not rare. It’s preventable.
And it’s expensive. In the U.S. alone, unnecessary steroid treatments for pseudorelapses cost over $12 million a year. That’s money spent on drugs, hospital stays, and managing side effects-all for a problem that could’ve been fixed with a cool shower and a UTI test.
How to Tell the Difference: A Simple 3-Step Check
Knowing whether it’s a relapse or pseudorelapse can save you from unnecessary treatment. Here’s what to do:
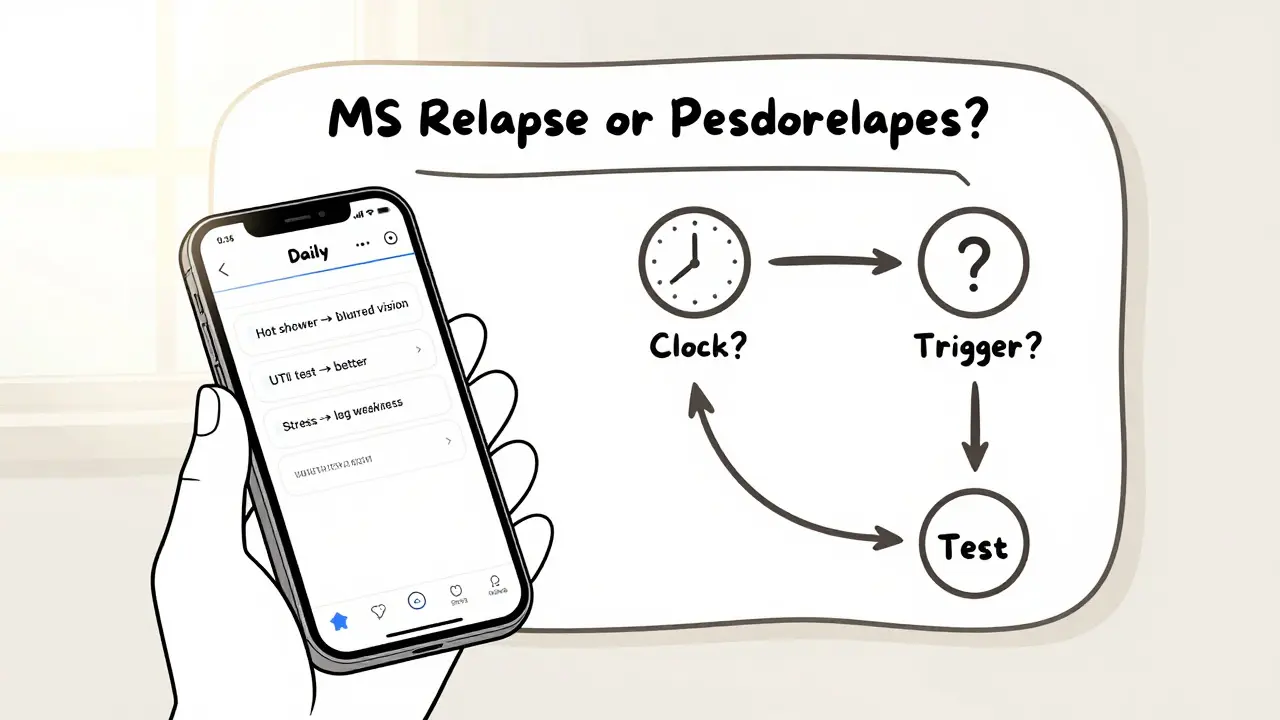
- Check the clock. Did symptoms last less than 24 hours? If yes, it’s likely a pseudorelapse. True relapses last days to weeks.
- Look for triggers. Did you have a fever? Take a hot shower? Urinate less than usual? Feel stressed? Track these. Keep a daily log-even a simple note on your phone helps.
- Test for infections. If you feel off, get a urine test. UTIs are sneaky. You might not feel pain, but your body is fighting an infection. That’s enough to trigger a pseudorelapse.
If you’re still unsure, your neurologist might order an MRI. New lesions? That’s a true relapse. No new lesions? It’s probably a pseudorelapse.
There’s also a new tool called the MS-Relapse Assessment Tool (MS-RAT). It uses your symptoms, temperature, and how much your daily life is affected to give a probability score. It’s 92% accurate in early testing. Ask your doctor if they use it.
What to Do When You Have a Pseudorelapse
You don’t need drugs. You need solutions.
- For heat: Use cooling vests, drink cold water, stay in air conditioning, avoid hot tubs and saunas. Many people with MS swear by cooling neck wraps-they work fast.
- For UTIs: Drink water, get tested, and take antibiotics if needed. Don’t wait. UTIs can make you feel awful even without a fever.
- For stress: Rest. Breathe. Talk to someone. Sometimes just taking a day off helps your nervous system reset.
- For fatigue: Don’t push through. Overexertion makes symptoms worse. Pace yourself.
One person on MyMSTeam said, “When my leg gave out during a heatwave, my neurologist told me to put on my cooling vest. Within two hours, I could walk again. No IV, no side effects.” That’s the power of knowing the difference.
Why This Matters for Long-Term Health
True relapses add up. Each one can leave behind permanent damage. That’s why disease-modifying therapies (DMTs) are so important-they reduce how often these attacks happen.
Pseudorelapses? They don’t cause damage. They don’t make MS worse. But they can still mess with your life. Especially if you’re older or already have disability. Some people over 55 don’t fully bounce back after a pseudorelapse-not because their MS got worse, but because their body’s weaker. They get deconditioned. That’s why staying active-even gently-is crucial.
Also, the more you learn about your triggers, the more control you have. You stop fearing every symptom. You stop rushing to the ER. You start managing your life, not just reacting to it.
What Doctors Should Be Doing (And Often Aren’t)
Specialized MS neurologists get it right 85% of the time. General neurologists? Only 60%. Primary care doctors? Just 45%. That’s a huge gap.
Guidelines from the American Academy of Neurology say: before calling it a relapse, rule out fever, infection, and metabolic issues. But too many clinics skip this step. Patients get steroids because it’s easier than testing.
Ask your doctor: “Could this be a pseudorelapse? Have you checked for infection or heat exposure?” If they haven’t thought about it, it’s time to have that conversation.
There are tools out there-like the ARMS questionnaire-that help measure how much your symptoms are affecting your daily life. If your score is below 4, it’s less likely to be a true relapse. Bring it up. Ask for it.
Final Takeaway: Know Your Body, Not Just Your Diagnosis
MS isn’t just about relapses. It’s about understanding your body’s signals. A flare-up isn’t always a sign your disease is progressing. Sometimes, it’s just your body saying, “I’m too hot,” or “I need to pee,” or “I’m stressed out.”
Don’t let fear drive your treatment. Learn your triggers. Keep a simple log. Test for UTIs before assuming it’s a relapse. Ask for an MRI if you’re unsure. And never let someone push steroids on you without checking the basics first.
True relapses need steroids. Pseudorelapses need rest, cooling, and common sense. Getting it right doesn’t just save you money. It saves you from side effects, hospital visits, and unnecessary stress.
You know your body better than anyone. Trust it. Learn it. And don’t let a misdiagnosis steal your peace of mind.
10 Comments
Coy Huffman
February 3 2026
I used to panic every time my leg went numb. Then I started tracking heat and UTIs. Turned out 80% of my 'relapses' were just a hot shower or a sneaky infection. No steroids needed. Life got way easier. 🙌
Mandy Vodak-Marotta
February 4 2026
Okay but can we talk about how the medical system just defaults to steroids because it’s faster than doing the work? I had a nurse tell me to ‘just wait it out’ after my third steroid round for what turned out to be a UTI. I was 27 and felt like I was being treated like a drama queen. Meanwhile, my neurologist didn’t even ask if I’d peed in the last 24 hours. It’s not just about knowledge-it’s about listening. And if you’re a woman with MS? Good luck getting anyone to believe you’re not just ‘stressed’.
Amit Jain
February 5 2026
Simple rule: if you feel bad after a hot day or you haven’t peed in a while, cool down and drink water. Wait 12 hours. If still bad, call doc. No need to freak out. Most times it’s just your body saying ‘hey, chill’.
Keith Harris
February 6 2026
Oh wow, another ‘MS guru’ telling people to skip steroids like it’s some kind of wellness trend. Let me guess-you’ve never had a real relapse where you couldn’t walk or see? Steroids aren’t perfect, but they’re the only thing that stops permanent damage. You’re romanticizing pseudorelapses like they’re just ‘bad days’. Meanwhile, people who actually need steroids get called ‘overreacting’ because of some Reddit post. This is dangerous nonsense.
Kunal Kaushik
February 6 2026
This hit home. My sister had a pseudorelapse last summer-thought she was having a relapse, ended up with a UTI. She was so scared, cried for hours. Then she put on her cooling vest and drank 3 liters of water. Two hours later, she was cooking dinner again. No IV. No side effects. Just… care. ❤️
Harriot Rockey
February 7 2026
I love how this post doesn’t just say ‘here’s the science’ but actually gives you tools-like the MS-RAT and the 3-step check. I printed it out and taped it to my fridge. My partner now asks me ‘did you hydrate?’ before I even say I’m having symptoms. That’s the kind of support that changes lives. Thank you for writing this. 💪
rahulkumar maurya
February 9 2026
Let’s be real-most of these ‘pseudorelapse’ stories come from people who don’t want to take their DMTs seriously. If your body’s failing, you need aggressive intervention. Cooling vests? UTI tests? That’s the bare minimum. You’re not ‘managing’ MS-you’re just delaying the inevitable. Real MS patients don’t wait for triggers. They fight. Every. Single. Day.
Alec Stewart Stewart
February 9 2026
I’ve been living with MS for 12 years. I used to take steroids every time I felt off. Then I started journaling. Now I know: if I’ve been in the sun or skipped water, it’s heat. If I’m tired and my bladder feels weird, it’s probably infection. I don’t panic anymore. I check. I rest. I drink. And I’ve had zero new lesions in 5 years. Knowledge > fear.
Roshan Gudhe
February 10 2026
There’s a quiet dignity in learning your body’s language. MS doesn’t just attack nerves-it attacks your sense of control. But when you learn that a hot shower isn’t a death sentence, that a UTI isn’t a failure, you stop being a patient and become a person again. You don’t need to conquer your body. You just need to listen. And sometimes, that’s the bravest thing you can do.
Nathan King
February 12 2026
The empirical evidence supporting steroid use in acute relapses is well-documented in the Annals of Neurology and the Cochrane Database. To conflate pseudorelapses with relapses without objective neuroimaging constitutes a clinically unsound approach that risks undermining evidence-based neurology. While patient education is laudable, it must not supersede diagnostic rigor. The anecdotal preference for cooling vests over methylprednisolone, while emotionally resonant, lacks the methodological integrity required for therapeutic decision-making.