Managing Allergies During Pregnancy Isn’t Optional - It’s Necessary
If you’re pregnant and dealing with sneezing, itchy eyes, or a runny nose that won’t quit, you’re not alone. About 20% of pregnant women experience worsened allergies or new-onset allergic rhinitis during pregnancy. But here’s the real question: can you take antihistamines safely - and if so, which ones?
The answer isn’t simple. Some antihistamines have been used for decades with no clear link to birth defects. Others have less data, but what’s out there is mostly reassuring. The key isn’t avoiding all medication - it’s choosing the right one at the right time.
First-Generation vs. Second-Generation: What’s the Difference?
Not all antihistamines are the same. They’re split into two groups based on how they affect your brain.
First-generation antihistamines - like chlorpheniramine (ChlorTrimeton) and diphenhydramine (Benadryl) - cross the blood-brain barrier. That’s why they make you drowsy. They’ve been around since the 1940s and 1950s. Millions of pregnant women have taken them. Studies tracking birth outcomes show no consistent pattern of birth defects. The American College of Obstetricians and Gynecologists (ACOG) lists chlorpheniramine as a safe option.
Second-generation antihistamines - like loratadine (Claritin) and cetirizine (Zyrtec) - don’t cause drowsiness because they barely enter the brain. They’re newer, so there’s less long-term data, but the evidence we have is strong. A large CDC study of over 10,000 pregnancies found no increased risk of major birth defects with loratadine or cetirizine. The Mayo Clinic and the American College of Allergy, Asthma & Immunology both recommend these as first-line choices for mild symptoms.
Which Antihistamines Are Safest in Pregnancy?
Based on decades of use and recent studies, these three are the most trusted:
- Chlorpheniramine - The oldest, most studied. Safe in all trimesters. Side effect? Drowsiness. Best taken at night.
- Loratadine - Non-sedating. Taken once daily. No increased risk of heart defects, cleft palate, or other major issues in multiple studies.
- Cetirizine - Also non-sedating for most people. Data from over 1,500 pregnancies show no safety red flags.
These are the ones your OB-GYN or allergist will likely suggest first. They’re available over the counter, but don’t assume that means they’re risk-free. Always check with your provider before starting anything.
What About the Newer Ones? Fexofenadine, Levocetirizine, Desloratadine
Fexofenadine (Allegra), levocetirizine (Xyzal), and desloratadine (Clarinex) are newer second-generation options. They’re marketed as even less sedating, but pregnancy data is limited. A few small studies haven’t raised alarms, but they’re not yet recommended as first-line choices. If your doctor prescribes one, it’s likely because you’ve tried the others and they didn’t work.
Don’t self-experiment. These aren’t proven safer - just newer. Stick with the well-studied options unless your provider says otherwise.
The Big Red Flag: Pseudoephedrine and Decongestants
Many allergy meds combine antihistamines with decongestants like pseudoephedrine. That’s where things get risky.
Pseudoephedrine - found in Sudafed and many multi-symptom cold/allergy pills - has been linked to a small but real increase in abdominal wall defects (like gastroschisis) when taken during the first trimester. The ACOG says avoid it entirely in the first 12 weeks. After that, it may be considered at low doses (30-60 mg every 4-6 hours, max 240 mg/day) if you have severe congestion and no high blood pressure.
Always read labels. If a product says “sinus relief,” “cold + flu,” or “allergy + congestion,” it likely contains pseudoephedrine or phenylephrine. Skip them unless your doctor says yes.
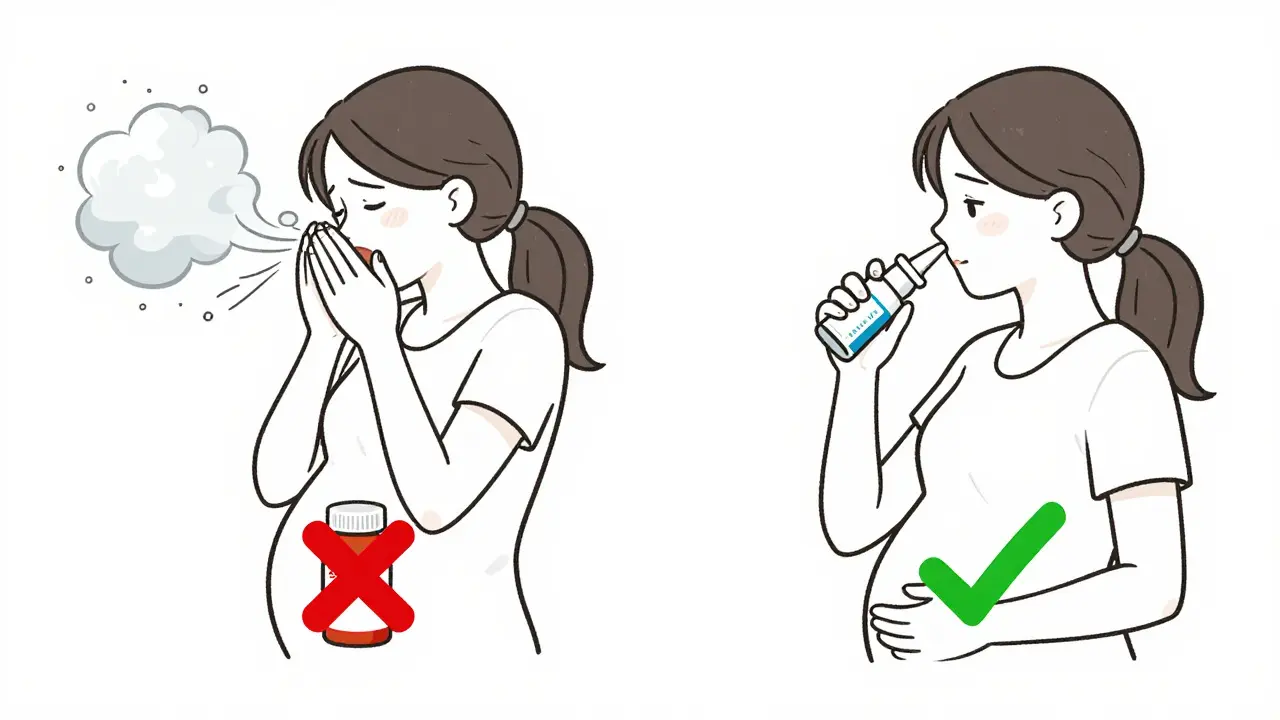
Nasal Sprays: A Better Option for Moderate to Severe Symptoms
If antihistamines alone aren’t enough, nasal sprays are often the next step - and they’re safer than oral meds.
Corticosteroid sprays like budesonide (Rhinocort), fluticasone (Flonase), and mometasone (Nasonex) are considered safe in all trimesters. They work locally in the nose, so very little enters your bloodstream. The American Academy of Family Physicians rates them as safe (evidence rating B), and the Mayo Clinic recommends them for moderate to severe allergic rhinitis.
Use them daily, not just when symptoms flare. It takes a few days to build up full effect. And don’t use them with decongestant sprays (like oxymetazoline) - those can cause rebound congestion and aren’t recommended during pregnancy.
When Should You Skip Antihistamines Altogether?
You don’t need medication for every sniffle. Mild symptoms can often be managed with:
- Saline nasal rinses
- Keeping windows closed during high pollen seasons
- Using HEPA filters at home
- Washing bedding weekly in hot water
- Showering after being outside
But if your allergies are keeping you awake, stopping you from eating, or making you anxious - that’s when treatment becomes necessary. Untreated severe rhinitis can lead to sinus infections or worsen asthma. And uncontrolled asthma during pregnancy carries far greater risks than taking a safe antihistamine.

What About Natural Remedies or Herbal Supplements?
Don’t assume “natural” means safe. Butterbur, stinging nettle, and quercetin are sometimes promoted for allergies, but there’s no solid safety data for them in pregnancy. Some herbs can stimulate uterine contractions or interfere with hormone levels.
The American College of Obstetricians and Gynecologists explicitly advises against using herbal supplements without medical approval. Stick to what’s been studied - not what’s trendy.
What to Do If You Took an Antihistamine Before Knowing You Were Pregnant
If you took diphenhydramine or loratadine in the first few weeks before you knew you were pregnant, don’t panic. The critical window for major birth defects is between weeks 3 and 8. Most antihistamines don’t cause harm even if taken then.
Studies show no increased risk of malformations from early exposure to chlorpheniramine, loratadine, or cetirizine. The key is to stop taking anything unnecessary going forward and talk to your provider. They’ll likely just monitor your pregnancy normally.
Bottom Line: Your Best Moves
- For mild symptoms: Try loratadine or cetirizine first. They’re non-sedating and well-studied.
- If you need something stronger: Add a corticosteroid nasal spray like fluticasone.
- For nighttime relief: Chlorpheniramine is okay, but expect drowsiness.
- Avoid: Any product with pseudoephedrine or phenylephrine in the first trimester.
- Never: Take herbal supplements or combination cold/allergy pills without checking with your doctor.
The goal isn’t to live without medication. It’s to live well - without risking your baby’s health. If your allergies are controlling your life, talk to your OB-GYN or an allergist. There’s a safe, effective option out there for you.
Is it safe to take Zyrtec (cetirizine) while pregnant?
Yes, cetirizine (Zyrtec) is considered safe during pregnancy. Multiple studies involving over 1,500 pregnant women have not found an increased risk of birth defects or complications. It’s one of the most commonly recommended second-generation antihistamines by the Mayo Clinic and the American College of Allergy, Asthma & Immunology. Take the lowest effective dose - usually 10 mg once daily.
Can I take Benadryl (diphenhydramine) in pregnancy?
Benadryl is generally considered safe in pregnancy, especially for short-term use. It’s been used for decades with no clear link to birth defects. But it causes drowsiness, which can affect daily function and increase fall risk. It’s best used occasionally, not daily, and only if needed - like for nighttime relief or a bad allergic reaction.
What’s the safest antihistamine for allergy relief in the first trimester?
Chlorpheniramine and loratadine are the safest choices in the first trimester. Chlorpheniramine has the most long-term data, while loratadine is non-sedating. Avoid decongestants like pseudoephedrine entirely during this time. If symptoms are mild, try saline rinses and avoiding triggers first.
Are nasal sprays safer than oral antihistamines during pregnancy?
Yes, corticosteroid nasal sprays like Flonase and Rhinocort are often safer than oral antihistamines because they act locally in the nose. Very little of the medication enters your bloodstream, so there’s minimal fetal exposure. They’re recommended for moderate to severe symptoms and are safe to use in all three trimesters.
Can antihistamines cause miscarriage?
There is no consistent evidence that antihistamines like loratadine, cetirizine, or chlorpheniramine increase the risk of miscarriage. Large studies, including those from the CDC’s National Birth Defects Prevention Study, have not found a link. The bigger risk comes from uncontrolled allergies that lead to poor sleep, stress, or asthma flare-ups - all of which can affect pregnancy outcomes.
What to Do Next
If you’re pregnant and struggling with allergies, don’t suffer in silence. Talk to your OB-GYN or a board-certified allergist. Bring a list of everything you’ve taken - even over-the-counter stuff. They’ll help you match your symptoms with the safest, most effective treatment.
And remember: managing your allergies isn’t selfish - it’s essential. Better sleep, better breathing, and less stress mean a healthier pregnancy for you and your baby.

9 Comments
Michael Burgess
January 3 2026
I took Zyrtec all through my first pregnancy and it was a game-changer. No more 3 a.m. sneezing fits, no more puffy eyes. My OB said it was one of the safest options, and honestly? I’d do it again. Sleep > suffering.
veronica guillen giles
January 4 2026
Oh wow, so now we’re giving out medical advice like it’s a TikTok trend? 🙄 I took Benadryl because I was too tired to care - and my kid’s fine. But hey, if you wanna spend $80 on a consult just to ask if it’s okay to breathe, go ahead.
Haley Parizo
January 6 2026
The real issue isn’t the antihistamines - it’s how we’ve turned pregnancy into a high-stakes compliance test. You’re not a lab rat. You’re a person. If you need relief, take the well-studied meds. If you’re scared, talk to a real doctor - not a Reddit algorithm that thinks ‘CDC study’ = gospel.
Shanahan Crowell
January 6 2026
I love how this post doesn’t just list drugs - it gives context. Like, yeah, nasal sprays are safer because they don’t flood your system. That’s the kind of nuance we need. So many people panic and suffer needlessly. This is the kind of info that saves lives.
Hank Pannell
January 8 2026
Let’s deconstruct the pharmacological hierarchy here: first-gen antihistamines = historical precedent + robust epidemiological backing; second-gen = pharmacokinetic elegance + emerging longitudinal data. The risk-benefit calculus favors loratadine/cetirizine not because they’re ‘newer,’ but because they minimize CNS penetration - which, neurologically, reduces teratogenic potential. That’s not marketing - that’s pharmacodynamics. And yes, nasal corticosteroids are the gold standard for localized inflammation control. The blood-brain barrier isn’t just a buzzword - it’s a biological firewall.
Tiffany Channell
January 9 2026
Funny how everyone’s so chill about Zyrtec but won’t touch a single drop of vitamin D without a 12-page consent form. Meanwhile, Big Pharma’s been quietly funding ‘safe pregnancy’ studies for decades. Coincidence? Or is this just another way to keep pregnant women docile while they profit off your fear?
Ian Detrick
January 9 2026
There’s a deeper truth here: we don’t treat pregnancy like a medical condition - we treat it like a moral experiment. If you take a pill, you’re reckless. If you suffer silently, you’re noble. But the body doesn’t care about virtue signals. It just wants to breathe. And if antihistamines let you do that without fear? That’s not weakness. That’s wisdom.
Angela Goree
January 10 2026
I’m from Texas - we don’t mess around with ‘maybe safe.’ If it’s not FDA-approved for pregnancy, it’s a no-go. And if you’re using ‘studies’ to justify taking meds, you’re already on the slippery slope. My sister took Benadryl and her baby had a minor heart murmur - coincidence? Maybe. But I’m not gambling. Saline rinse. Humidifier. NO PILLS. EVER.
Angela Fisher
January 12 2026
You know what’s really scary? That this whole post is probably funded by Big Pharma. They’ve been pushing these ‘safe’ antihistamines for years - same way they pushed SSRIs in the 90s. Now look at how many kids are on ADHD meds. The CDC says ‘no link’ - but who funds the CDC? And why is there no long-term study on kids whose moms took cetirizine for 9 months? Hmm. Coincidence that the same companies make the drugs AND the ‘guidelines’? I’m not taking anything. Not even saline. I’m going full primal. No screens. No meds. No compromises.