Steroid Hyperglycemia Insulin Adjustment Calculator
How Steroids Affect Insulin Needs
Steroid therapy significantly increases insulin requirements. For prednisone 20mg or higher daily, experts recommend increasing total daily insulin by 30-50%.
Basal insulin should increase by 20-30%, and mealtime insulin by 50-100% (especially for breakfast and lunch).
Important: This calculator provides general guidance. Always consult your healthcare provider before adjusting medications.
Enter your current insulin dose and steroid dose to see recommended adjustments
Important Note: This tool is for educational purposes only. Always follow your healthcare provider's specific recommendations for insulin adjustments during steroid therapy.
Why Steroids Make Blood Sugar Spike in People with Diabetes
When you’re on steroids like prednisone or hydrocortisone, your blood sugar doesn’t just go up-it can go skyrocketing. This isn’t normal diabetes behavior. It’s steroid hyperglycemia, a direct side effect of glucocorticoids disrupting how your body handles sugar. Even if you’ve never had diabetes before, a short course of steroids can push your glucose levels into dangerous territory. And if you already have type 1 or type 2 diabetes, it’s like turning up the volume on a broken alarm-your body can’t keep up.
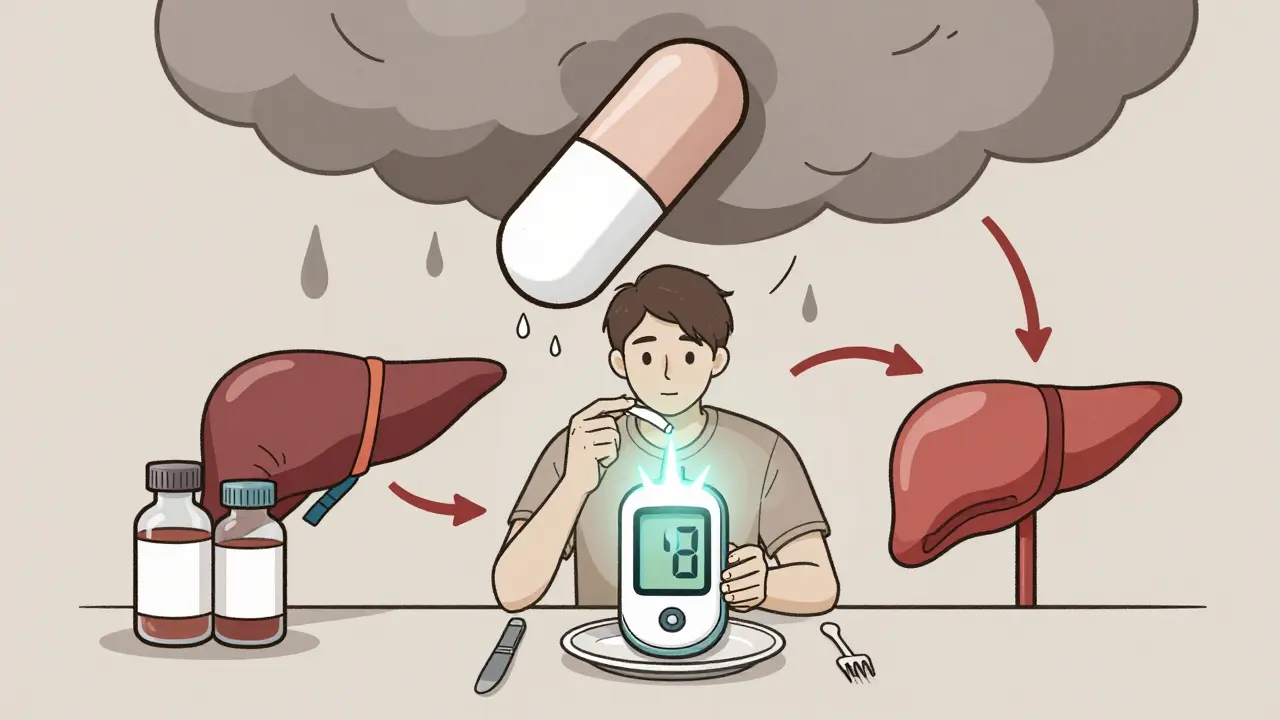
Steroids don’t just make you hungrier. They attack insulin’s ability to do its job. They block insulin from helping muscle and fat cells soak up glucose. They tell your liver to dump more sugar into your bloodstream. And they quiet down your pancreas so it doesn’t release enough insulin when you need it. The result? Your blood sugar spikes hardest after meals-especially breakfast and lunch-because that’s when the steroid hits its peak.
How Much Higher Will Your Blood Sugar Go?
It’s not guesswork. Studies show that if you’re taking 50 mg of hydrocortisone daily (or its equivalent in prednisone), your chance of needing insulin or other meds jumps by over 3 times. At 100 mg, it’s nearly 6 times higher. And if you’re on more than 120 mg? Your risk is over 10 times greater than someone not on steroids.
At hospitals, more than half of patients on high-dose steroids develop high blood sugar. Nearly 9 out of 10 have at least one episode where glucose hits over 180 mg/dL. And here’s the kicker: if you’re measuring only your fasting glucose, you’re missing up to 20% of the problem. Steroid spikes happen after eating, not overnight. So if you’re only checking your sugar in the morning, you’re flying blind for most of the day.
Who’s Most at Risk?
Not everyone reacts the same. If you already have type 2 diabetes, you’re more likely to crash into hyperglycemia. Age matters too-people over 65 are hit harder. Being overweight (BMI over 30) adds fuel to the fire. And if you’ve had prediabetes before, your body is already struggling. Add in other drugs like tacrolimus (common after transplants), and your risk shoots up another 35-45% because it shuts down insulin production even more.
Low magnesium? That’s another hidden trigger. For every 0.1 mg/dL drop in your magnesium level, your chance of high blood sugar goes up by 10-15%. Chronic hepatitis C? That doubles your risk. Even your timing matters. If you take your steroid in the morning, your sugar spikes 4 to 8 hours later. That’s why breakfast and lunch are the big battles-not dinner.
How to Adjust Insulin: The Real-World Protocol
If you’re on insulin and start steroids, you’re going to need more. A lot more. Experts like Dr. Guillermo Umpierrez recommend increasing your total daily insulin by 30-50% right away if you’re on 20 mg or more of prednisone daily. But here’s what most people get wrong: they just crank up their long-acting insulin. That’s not enough.
You need a basal-bolus approach. That means:
- Boost your basal (background) insulin by 20-30%
- Jump your mealtime insulin by 50-100%, especially for breakfast and lunch
Why? Because steroids hit hardest after those meals. If you’re on dexamethasone (which lasts 36-72 hours), you’ll need steady higher doses all day. But if you’re on prednisone or hydrocortisone (shorter acting), you can time your insulin spikes to match the steroid surge. No need to overdo dinner insulin-your steroid’s already worn off by then.
What About Oral Diabetes Medications?
Metformin? It helps a little, but it’s not enough. Most people on steroids need insulin-even if they’ve never used it before. Sulfonylureas? Risky. They force your pancreas to pump out more insulin, but steroids are already crushing your pancreas’s ability to respond. You could end up with wild swings: high after meals, then crashing later.
GLP-1 agonists like semaglutide? They’re not recommended during active steroid use. The body’s stress response overrides their effects. SGLT2 inhibitors? Avoid them. Steroids already raise your risk of dehydration and ketoacidosis. Adding an SGLT2i? That’s playing with fire.
Bottom line: insulin is the only reliable tool when steroids are in play. Oral meds are backup players at best.
The Taper Trap: Why Stopping Steroids Can Be More Dangerous
This is where most people get hospitalized. When the steroid dose drops, your body doesn’t instantly return to normal. Your insulin needs drop too-but if you don’t adjust, you’ll crash. A Johns Hopkins study found 18% of readmissions within 30 days of stopping steroids were due to hypoglycemia from unchanged insulin doses.
Every time your steroid dose goes down by 10 mg (prednisone equivalent), cut your total daily insulin by 10-20%. Don’t wait for your sugar to drop. Be proactive. If you were on 50 units of insulin daily during peak steroid use, and you drop from 40 mg to 30 mg of prednisone, reduce insulin by 5-10 units right away. Monitor closely. Your body is still adjusting.
Dr. Robert Rushakoff at UCSF saw 22% of patients develop severe low blood sugar during tapering because their insulin wasn’t scaled back. This isn’t rare. It’s predictable. And it’s preventable.
Monitoring: More Than Just Fingersticks
Checking your sugar four times a day isn’t optional-it’s essential. Check fasting, then 2 hours after breakfast, lunch, and dinner. If your glucose is over 180 mg/dL at any point, adjust your next mealtime insulin. Don’t wait for a pattern to emerge. Act fast.
Continuous glucose monitors (CGMs) are game-changers. A Dexcom study showed CGM users adjusted insulin doses 37% more accurately than those using fingersticks. Why? Because you see the spikes as they happen-not hours later. You see the lag between steroid dose and sugar peak. You catch the drop during tapering before it becomes dangerous.
Apps like Glytec’s eGlucose Management System are now used in 68% of major U.S. hospitals. They link steroid dosing schedules to insulin recommendations in real time. If your doctor hasn’t mentioned CGM or a digital tool, ask. It’s not luxury-it’s safety.

What Hospitals Are Doing Right (And What You Should Ask For)
Top hospitals now have steroid-specific glycemic protocols. The EndoTool System, used in nearly 300 U.S. hospitals, cuts hyperglycemia by 27% by automatically adjusting insulin based on steroid dose, weight, and glucose trends. The Joint Commission now requires hospitals to have these protocols in place.
If you’re admitted and on steroids, ask: “Do you have a steroid hyperglycemia protocol?” If they say no, push. Your blood sugar control isn’t an afterthought-it’s critical to your recovery. Even outpatient clinics should have a plan. A 2022 CMS report found 22% of steroid-treated patients had preventable complications because no one had a clear plan.
What’s Next: The Future of Steroid-Driven Blood Sugar Control
Machine learning is stepping in. The 2023 ADVANCE trial used an algorithm that predicted insulin needs with 85% accuracy by factoring in steroid dose, BMI, and baseline HbA1c. It slashed hyperglycemia episodes by 41%. Now, pilot programs at Mayo Clinic are integrating CGM data with EHRs to auto-suggest insulin changes as steroids are given.
By 2027, the American Diabetes Association expects 75% of U.S. hospitals to have formal steroid hyperglycemia protocols. But until then, it’s on you-and your care team-to demand it. Don’t let steroid therapy become a diabetes emergency. Know the risks. Track your numbers. Adjust early. And never assume your insulin needs stay the same.
Key Takeaways
- Steroid hyperglycemia is common, predictable, and dangerous if ignored.
- Insulin needs rise 30-50% with moderate steroid doses-basal and bolus both need increases.
- Post-meal glucose (not fasting) is the real indicator of steroid impact.
- Oral diabetes meds are usually insufficient; insulin is the gold standard.
- Reducing insulin during steroid taper is just as important as increasing it.
- CGMs dramatically improve safety and accuracy during steroid therapy.
- Always ask if your hospital or clinic has a steroid hyperglycemia protocol.
Can steroids cause diabetes in someone who never had it before?
Yes. Steroid-induced diabetes (SIDM) can develop in people with no prior history of diabetes. It’s most common with high-dose, long-term steroid use-especially in those over 65, overweight, or with a family history of diabetes. Blood sugar usually returns to normal after stopping steroids, but some people develop permanent type 2 diabetes if their pancreas was already struggling.
How long does steroid-induced high blood sugar last?
It lasts as long as the steroid is active in your system. For short-acting steroids like prednisone or hydrocortisone, glucose levels may stay high for 2-4 days after the last dose. For long-acting ones like dexamethasone, it can take a week or more. Blood sugar typically normalizes within 1-2 weeks after stopping steroids completely, but insulin adjustments must be made gradually during tapering to avoid lows.
Should I stop my diabetes meds when I start steroids?
No. Never stop your medications without medical supervision. Most people need to add insulin, not stop oral meds. Metformin can usually continue, but sulfonylureas and SGLT2 inhibitors may need to be paused. Always consult your doctor-your steroid dose, diabetes type, and overall health determine what’s safe.
Is it safe to use insulin with steroids if I have type 1 diabetes?
Yes, and it’s necessary. People with type 1 diabetes often need 50-100% more insulin during steroid therapy. The steroids worsen insulin resistance and can trigger diabetic ketoacidosis (DKA) if insulin is under-dosed. Frequent glucose checks and CGM are critical. Don’t reduce your insulin just because you’re eating less-you’re still fighting steroid-driven glucose production.
Why does my blood sugar spike after lunch but not dinner when I take steroids in the morning?
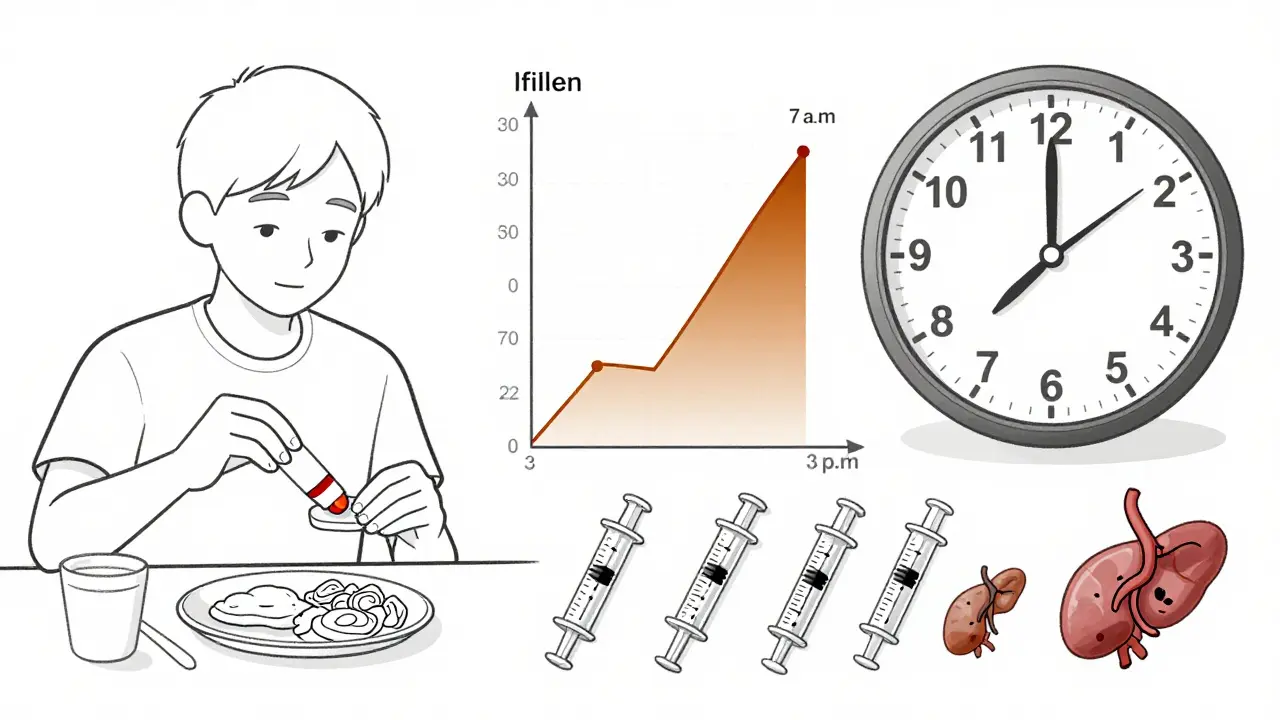
Steroids like prednisone peak in your bloodstream 4-8 hours after you take them. If you take your dose at 7 a.m., that peak hits around 11 a.m. to 3 p.m.-right when you’re digesting breakfast and lunch. Dinner happens after the steroid has mostly cleared, so your sugar stays more stable. That’s why insulin needs are highest for breakfast and lunch meals, not dinner.
Can magnesium supplements help lower blood sugar during steroid use?
Some evidence suggests yes. Low magnesium levels are linked to worse insulin resistance during steroid therapy. Each 0.1 mg/dL drop in magnesium raises hyperglycemia risk by 10-15%. If your levels are low, your doctor may recommend a supplement. But don’t self-prescribe-too much magnesium can cause diarrhea or interact with other meds. Get a blood test first.
What should I do if I’m on steroids and my blood sugar keeps crashing?
If you’re experiencing frequent lows, your insulin dose is likely too high for your current steroid level. This usually happens during tapering. Check your steroid dose: if you’ve reduced it, you need to reduce insulin too. Cut your total daily insulin by 10-20% for every 10 mg drop in prednisone equivalent. Use a CGM if possible, and keep fast-acting carbs on hand. Contact your doctor immediately if lows continue.
10 Comments
Sidhanth SY
January 30 2026
Man, I was on prednisone for a month last year and thought my sugar was just acting up. Turns out it was steroid hyperglycemia. Didn't know about the breakfast/lunch spike thing until I got a CGM. Game changer. Now I just bump my bolus before lunch and call it a day.
Adarsh Uttral
January 31 2026
so like... if u take steroid at 8am u gotta watch ur lunch n breakfast? why not just skip lunch lol jk dont do that
April Allen
February 1 2026
Steroid-induced insulin resistance operates via glucocorticoid receptor-mediated transcriptional repression of GLUT4 translocation and upregulation of hepatic gluconeogenic enzymes-namely PEPCK and G6Pase. The pharmacokinetic half-life of the glucocorticoid dictates the temporal profile of hyperglycemia, which is why short-acting agents like prednisone require meal-timed insulin boluses rather than basal-only adjustments. Most clinicians underdose bolus insulin because they're fixated on fasting glucose, missing the postprandial phenotypes entirely.
Niamh Trihy
February 3 2026
This is such an important post. I’ve seen so many patients get discharged on high-dose steroids without any glycemic plan. The taper trap is real-I had a patient crash into severe hypoglycemia after their dose dropped from 40mg to 30mg of prednisone. They didn’t adjust insulin. We had to admit them. Please, if you’re on steroids, work with your endo before you even start.
Donna Fleetwood
February 4 2026
YES. CGMs saved me. I used to think I was fine because my morning sugar was okay. Then I got a Dexcom and saw my lunch spikes hitting 280. I was so mad at myself for not knowing sooner. You don’t have to be perfect, just proactive. And yes, insulin is the MVP here-no shame in needing it.
Sazzy De
February 6 2026
My doc didn't mention any of this when I started prednisone. I just kept taking my metformin and figured it'd be fine. Big mistake. Sugar went nuts. Had to start insulin on the spot. Learned the hard way. CGM is not optional anymore. Seriously.
Gaurav Meena
February 7 2026
Bro this is gold 🙏 I’m a type 1 and got put on steroids after a flare-up. Went from 50 units to 110 in a week. My endo was like ‘yeah this is normal’ but no one told me why. Now I know it’s the liver dumping sugar and insulin resistance. Also-magnesium! My levels were low. Took a supplement and my spikes got a bit better. Thanks for the real talk!
Katie and Nathan Milburn
February 8 2026
It is of considerable clinical significance that the majority of outpatient diabetes management protocols fail to account for the temporal dynamics of glucocorticoid pharmacokinetics. The failure to implement basal-bolus insulin titration protocols in tandem with steroid dosing schedules constitutes a systemic gap in care delivery. The Joint Commission mandates such protocols, yet compliance remains inconsistent across institutions.
Natasha Plebani
February 8 2026
The paradox of steroid hyperglycemia is that it’s both predictable and perpetually underestimated. We know the mechanism, we know the timeline, we know the risk factors-yet we treat it like an emergency instead of a planned event. It’s not a complication; it’s a pharmacological consequence. Why do we wait for glucose to hit 300 before acting? We should be preemptive, not reactive. The algorithmic approaches in the ADVANCE trial aren’t futuristic-they’re necessary. If we can predict drug interactions in oncology, why not here?
calanha nevin
February 10 2026
When you’re tapering steroids, reduce insulin gradually but don’t wait for symptoms. Hypoglycemia during taper is preventable but often missed because providers assume the patient’s diabetes has returned to baseline. It hasn’t. The pancreas is still recovering. Monitor for 2 weeks after the last dose. Use CGM. If your hospital doesn’t have a protocol, request one. Your safety isn’t negotiable.