Statin Muscle Symptoms Checker
This tool helps determine if your muscle symptoms are likely statin-induced myopathy or neuropathy. Remember: This is for informational purposes only and not a medical diagnosis. Always consult your doctor for proper evaluation.
Many people on statins start noticing muscle cramps, aches, or tingling and immediately worry: is this the statin? Or is it something else? The truth is, not all muscle discomfort on statins is the same. Some is myopathy-a problem in the muscle itself. Others may be neuropathy-a nerve issue. Mixing them up can lead to the wrong decision: stopping a life-saving drug, or ignoring a real nerve problem.
What Statin Myopathy Really Feels Like
Statin-associated myopathy doesn’t usually hit with sudden, sharp pain. It creeps in. You might notice your legs feel heavier climbing stairs. Getting up from a chair takes more effort. Your shoulders ache when you reach for a high shelf. These aren’t random twitches-they’re signs of weakness in your proximal muscles: thighs, hips, shoulders, and upper arms. The key clue? The pain is usually bilateral. Both legs, both arms. It’s not one-sided like a pinched nerve. And unlike a pulled muscle, it doesn’t improve with rest. In fact, it gets worse with activity. Most people don’t realize how much they’ve slowed down until they compare how they moved six months ago. Creatine kinase (CK) levels are often only slightly raised-or even normal. That’s why many doctors miss it. A CK level above four times the upper limit of normal is a red flag, but most cases fall below that. The real diagnosis comes from timing: symptoms started within weeks of beginning or increasing the statin dose. They got better after stopping. And if you restart the same statin? They come back, usually faster and worse. Why does this happen? Statins block HMG-CoA reductase, the same enzyme your liver uses to make cholesterol. But your muscles use that enzyme too. When it’s blocked, your muscle cells make less coenzyme Q10-by up to 40% in just 30 days. That’s like cutting off the fuel supply to your muscle engines. Mitochondria start to fail. Calcium leaks out of storage. Muscle fibers break down slowly, without swelling or redness. That’s why blood tests for inflammation (like CRP) are normal.Neuropathy: When the Nerves Are the Problem
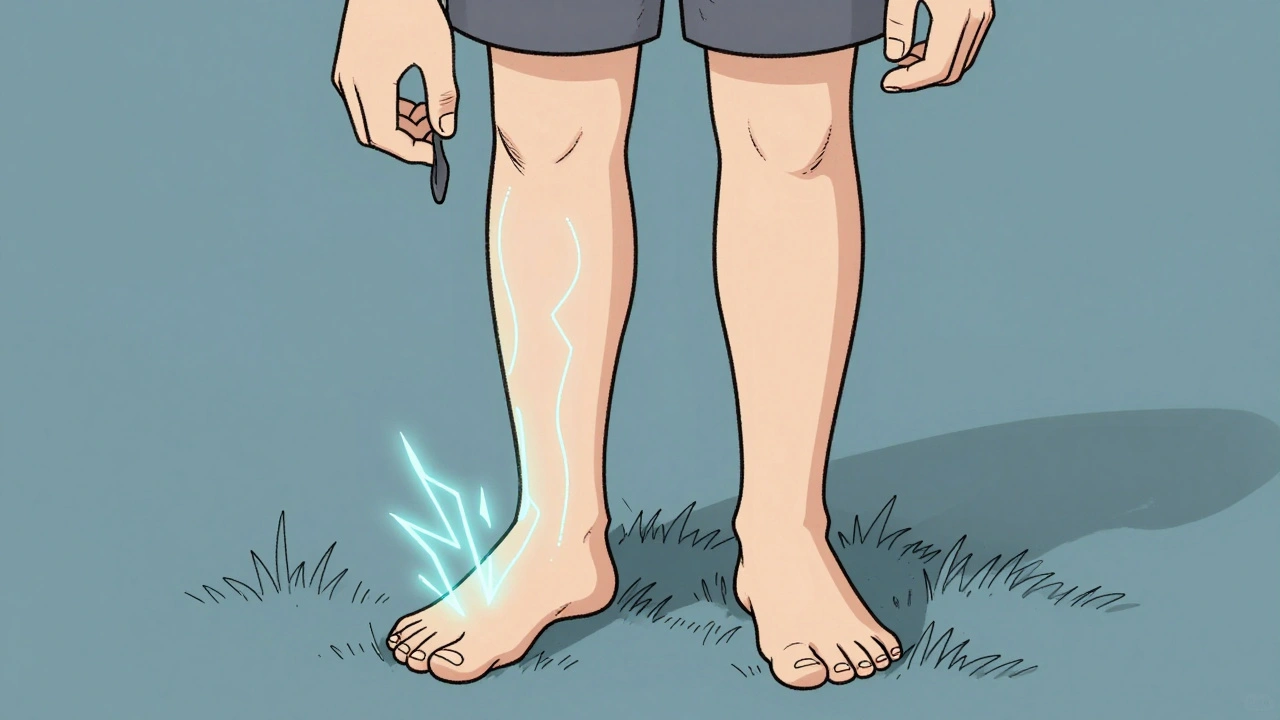
If your cramps feel more like burning, tingling, or electric shocks in your feet or hands, especially at night, you might be dealing with neuropathy. This isn’t muscle weakness-it’s nerve damage. You might drop things more often. Your toes feel numb in socks. Walking barefoot on grass feels strange, like you’re not fully connected to the ground. Neuropathy follows a stocking-glove pattern: symptoms start in the toes and fingers, then creep up the limbs. It’s not symmetric in the same way myopathy is-it’s more about sensation than strength. You can still lift your leg, but you can’t feel if your shoe is twisted. Here’s the twist: the evidence on statins causing neuropathy is messy. Some studies say yes. Others say no. A 2019 study of over 600 people found that those on statins were less likely to have unexplained peripheral neuropathy. Why? Maybe statins reduce inflammation that damages nerves. Or maybe the cholesterol-lowering effect helps protect nerve membranes. But there’s also a theory that statins lower LDL too much, starving nerves of vitamin E, which they need to stay healthy. The only way to be sure? Electrodiagnostic testing. Nerve conduction studies can show if sensory nerves are firing weakly. If your nerve signals are slow or absent, that’s axonal neuropathy. If the signals are strong but delayed, it’s demyelinating. Statins don’t cause demyelination. If your test shows that, look elsewhere-like diabetes or autoimmune disease.How to Tell the Difference
You can’t rely on symptoms alone. But here’s what to look for:- Location: Myopathy = hips, thighs, shoulders. Neuropathy = feet, hands.
- Feeling: Myopathy = dull ache, heaviness, weakness. Neuropathy = burning, pins and needles, numbness.
- Strength: Myopathy = you struggle to rise from a chair or lift your arms. Neuropathy = you can move fine, but you don’t feel what you’re touching.
- CK levels: Myopathy = often elevated (even mildly). Neuropathy = always normal.
- Response to stopping: Myopathy = improves in weeks. Neuropathy = may not improve, or gets worse if the cause is something else.
What to Do Next
If you’re on a statin and have new muscle symptoms:- Don’t stop cold. Stopping statins without a plan raises your risk of heart attack or stroke. Talk to your doctor first.
- Get a CK test. Even if it’s only slightly high, it’s a clue.
- Check for other causes. Thyroid problems, alcohol use, or vitamin D deficiency can mimic statin myopathy. Rule them out.
- Consider nerve testing. If symptoms are sensory (burning, numbness), ask for nerve conduction studies.
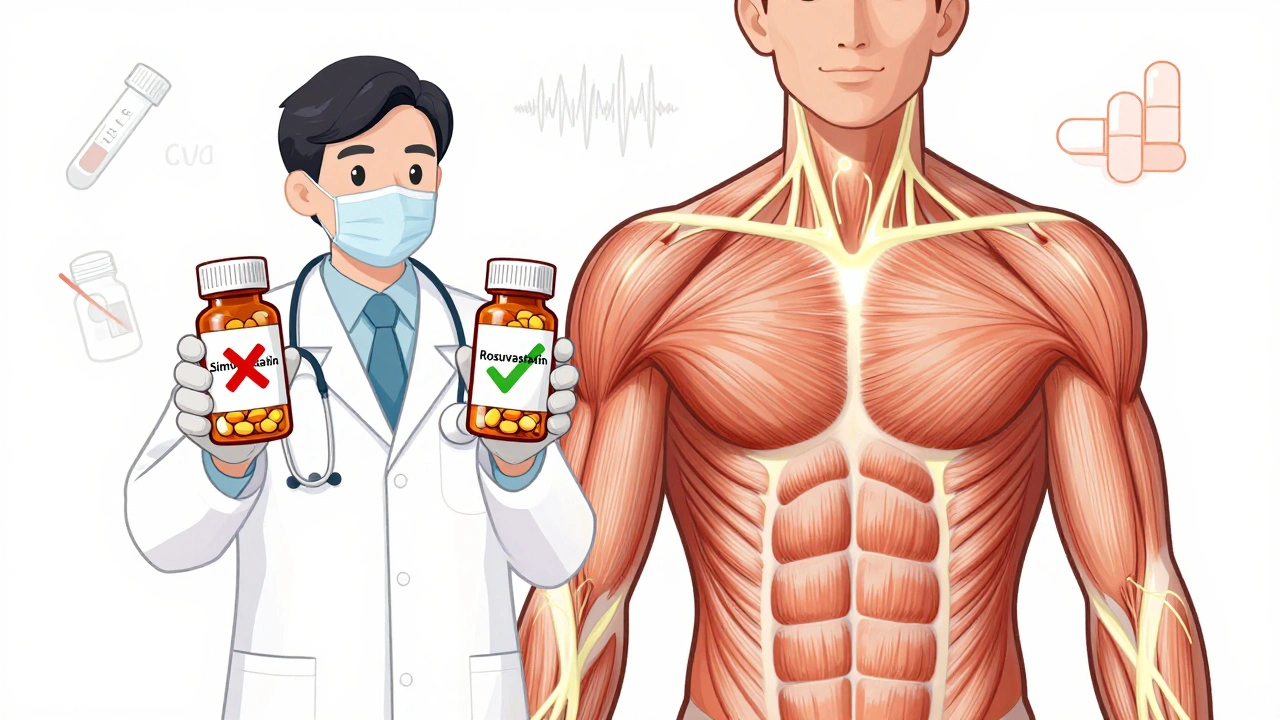
- Try a different statin. If it’s myopathy, switching from simvastatin to pravastatin or rosuvastatin works for about 60% of people. Hydrophilic statins are less likely to enter muscle cells.
- Use non-statin options. If you truly can’t tolerate any statin, ezetimibe or PCSK9 inhibitors can lower LDL just as well. They don’t cause myopathy.
Who’s at Higher Risk?
Some people are more likely to get muscle problems on statins:- Women over 65
- People taking statins with fibrates (like gemfibrozil)
- Those with kidney or liver disease
- People with the SLCO1B1 gene variant (this affects how the body clears simvastatin)
- Those on high doses-especially 80mg of simvastatin
What About CoQ10 Supplements?
You’ve probably seen ads for CoQ10 to “prevent statin muscle pain.” The science doesn’t back it up. A 2015 JAMA study gave CoQ10 to 44 people with statin-related muscle pain. Half got placebo. After 30 days, there was no difference in pain levels. CoQ10 might help some, but it’s not a magic fix.When to See a Neurologist
If your symptoms don’t improve after 2-3 months of stopping the statin, it’s time. That’s not just “waiting it out.” That’s a signal that something else is going on. Maybe you had mild neuropathy before you started the statin, and it got worse because you were less active. Maybe you developed a new autoimmune condition. Or maybe it’s something else entirely. Don’t let a doctor brush it off as “just aging.” Muscle weakness isn’t normal at any age. And numbness in your feet isn’t something you just live with.Bottom Line
Muscle cramps on statins are common-but not always caused by statins. Myopathy is real, and it’s treatable. Neuropathy is trickier, and the link to statins is still debated. The key is to test, not guess. Check CK. Test nerves. Rule out other causes. Don’t stop your statin without a plan. And don’t assume every ache is the statin’s fault. Your heart needs protection. Your muscles need care. You don’t have to choose one over the other. With the right diagnosis, you can keep both.Can statins cause permanent muscle damage?
In rare cases, yes-especially if statin myopathy progresses to rhabdomyolysis, where muscle tissue breaks down and releases harmful proteins into the blood. But this is extremely uncommon, affecting fewer than 1 in 10,000 people on standard doses. Most muscle symptoms resolve completely within weeks of stopping the statin. Permanent damage usually only happens if symptoms are ignored for months and the person continues taking the drug.
Is it safe to restart a statin after muscle cramps?
It often is, but not the same one. About 60% of people who had muscle pain on one statin can tolerate a different one, especially hydrophilic types like pravastatin or rosuvastatin. Start with a low dose and increase slowly. If pain returns, stop immediately and consider non-statin options like ezetimibe or PCSK9 inhibitors.
Do all statins cause muscle problems equally?
No. Lipophilic statins like simvastatin and atorvastatin enter muscle cells more easily and are more likely to cause myopathy. Hydrophilic statins like pravastatin and rosuvastatin stay mostly in the liver and are much gentler on muscles. High doses of simvastatin (80mg) carry the highest risk.
Can statins cause numbness in hands and feet?
Possibly, but the evidence is conflicting. Some patients report numbness, and there are biological reasons why statins might affect nerves-like lowering vitamin E or cholesterol needed for nerve membranes. But large studies haven’t confirmed this as a common side effect. If numbness appears, it’s essential to rule out diabetes, vitamin B12 deficiency, or other causes before blaming the statin.
Should I take CoQ10 with my statin to prevent cramps?
There’s no strong evidence that CoQ10 supplements prevent or reduce statin-related muscle pain. A major 2015 study found no difference between CoQ10 and placebo. While it’s generally safe, don’t rely on it as a solution. Focus instead on identifying the true cause of your symptoms and choosing the right statin-or alternative therapy-if needed.
What are the alternatives to statins if I can’t tolerate them?
Ezetimibe lowers LDL by about 15-20% and is well-tolerated. PCSK9 inhibitors (alirocumab, evolocumab) can lower LDL by 50-60% and are given as monthly injections. Both are proven to reduce heart attack and stroke risk. They don’t cause muscle problems. For many people, these are better long-term options than struggling with statin side effects.
14 Comments
Inna Borovik
December 6 2025
Let’s be real-most doctors don’t even check CK levels before blaming statins. I’ve seen patients get dropped from their meds based on anecdotal complaints while ignoring diabetes, B12 deficiency, or even spinal stenosis. The real issue isn’t the statin-it’s the lazy diagnostics. CoQ10? A placebo with a markup. If your doctor can’t interpret a basic lipid panel, why trust them with your nerves?
Arjun Deva
December 7 2025
Statins are a pharmaceutical scam designed to keep you dependent. They lower cholesterol, sure-but they also drain your mitochondria, fry your nerves, and make you weak so you need MORE drugs. The FDA knows. The drug reps know. Your doctor? Probably gets kickbacks. CoQ10 doesn’t work because they don’t want it to work. They’d rather sell you a $1,200 injection than admit the statin is poisoning you.
Rashmi Gupta
December 8 2025
Actually, I think this whole article is wrong. I’ve been on statins for 12 years, never had a cramp, and my CK’s always normal. Meanwhile, my neighbor dropped statins and now his neuropathy got worse. Coincidence? Maybe. But I’d bet it’s because he stopped moving and gained weight. It’s not the drug-it’s the lifestyle. Stop blaming pills for your laziness.
Andrew Frazier
December 9 2025
USA has the best healthcare system in the world, and yet we let people whine about muscle cramps? Back in my day, we just took our medicine and worked through pain. You think your body’s fragile? Go lift a tractor tire. Statins save lives. If you can’t handle a little ache, maybe you shouldn’t be on the planet. Also, CoQ10 is a scam sold by yoga moms.
Nava Jothy
December 9 2025
OMG I’ve been waiting for someone to explain this!!! 🙌 I had burning feet for 8 months, thought it was statins, went off them… and then my neurologist found I had B12 deficiency AND prediabetes. The statin was a red herring. My doctor didn’t even test my B12 for 6 months. I’m so mad. But also… relieved? Like, why is this so hard to figure out?? 😭
olive ashley
December 10 2025
Here’s the thing nobody says: statins don’t cause myopathy. The pharmaceutical industry just wants you to think they do so they can sell you more expensive drugs. They know the real culprit is glyphosate in your food, EMFs from your phone, and mold in your house. CoQ10? Useless. But if you take magnesium, vitamin D, and quit gluten? Your legs will thank you. I’ve seen it. The system doesn’t want you to know this.
Ibrahim Yakubu
December 10 2025
My cousin in Lagos got statins after his heart attack. He started having leg pain. He went to a clinic. Doctor said ‘it’s the medicine’. He stopped. Two weeks later, he had a stroke. Now he’s paralyzed. Statins aren’t the problem-ignorance is. If you feel pain, don’t stop. Go to a specialist. Don’t listen to Reddit. Your life depends on it.
Dan Cole
December 11 2025
There is a metaphysical dimension to statin-induced myopathy that transcends biochemical reductionism. The muscle is not merely a tissue-it is an expression of the organism’s will to persist. When HMG-CoA reductase is inhibited, the body’s ontological integrity is compromised. CoQ10 supplementation is a bandage on a ruptured artery of meaning. The real question: Are we treating disease-or denying mortality? The answer lies not in CK levels, but in the silence between breaths.
Max Manoles
December 12 2025
I’ve been on rosuvastatin for 5 years. Had mild shoulder ache for a few weeks after starting. Got my CK checked-slightly elevated. Switched to pravastatin. Ache gone in 3 weeks. No CoQ10. No miracle diets. Just science. If you’re worried, get tested. Don’t guess. And if your doctor won’t order a CK? Find a new one. This isn’t rocket science.
Jackie Petersen
December 12 2025
Statins are part of the globalist agenda to depopulate the elderly. They’re in the water, the bread, the vaccines. You think your cramps are random? Think again. The CDC knows. The WHO knows. But they won’t tell you because they profit from your fear. CoQ10 is banned in 37 countries because it interferes with their control. Wake up.
Annie Gardiner
December 13 2025
Wait-so you’re saying I might’ve been misdiagnosed? I stopped statins because of foot numbness, and now my cholesterol’s through the roof. But I also got diagnosed with MS last year… so maybe it was that all along? I feel so stupid. But also… kind of relieved? Like, maybe I didn’t ruin my health by quitting?
Kumar Shubhranshu
December 14 2025
CK normal? Numb feet? Stop statin. Get B12. Get HbA1c. Done. No drama. No supplements. Just test. If you don’t, you’re just wasting your doctor’s time.
Mayur Panchamia
December 16 2025
Statins? Pfft. I’ve been on them since 2010-simvastatin 80mg-and I run marathons. My legs feel like steel cables. People who whine about cramps? They’re the same ones who eat McDonald’s, sit all day, and then blame Big Pharma. Get off your couch. Lift something. Drink water. Stop being a victim. Statins don’t break people-laziness does.
Akash Takyar
December 17 2025
Thank you for this clear, well-researched breakdown. I’ve been a primary care physician for 22 years, and I’ve seen too many patients panic and stop their statins out of fear-not facts. The distinction between myopathy and neuropathy is critical, and too few clinicians take the time to explain it. I always tell my patients: ‘If your muscles feel heavy and weak, check CK. If your feet feel like they’re wrapped in plastic, check nerves and B12.’ Simple. Effective. Life-saving. Let’s stop the noise and focus on the data.