When your liver gets scarred, it doesn’t heal the way your skin does. Instead of repairing itself, it builds hard, fibrous tissue that blocks blood flow and stops it from doing its job. This isn’t just a minor problem-it’s cirrhosis, the final stage of chronic liver damage. And once it sets in, the damage is permanent. But here’s the thing: many people don’t know they have it until it’s too late. That’s because cirrhosis sneaks up on you. You might feel fine for years while your liver quietly turns to scar tissue.
What Exactly Is Cirrhosis?
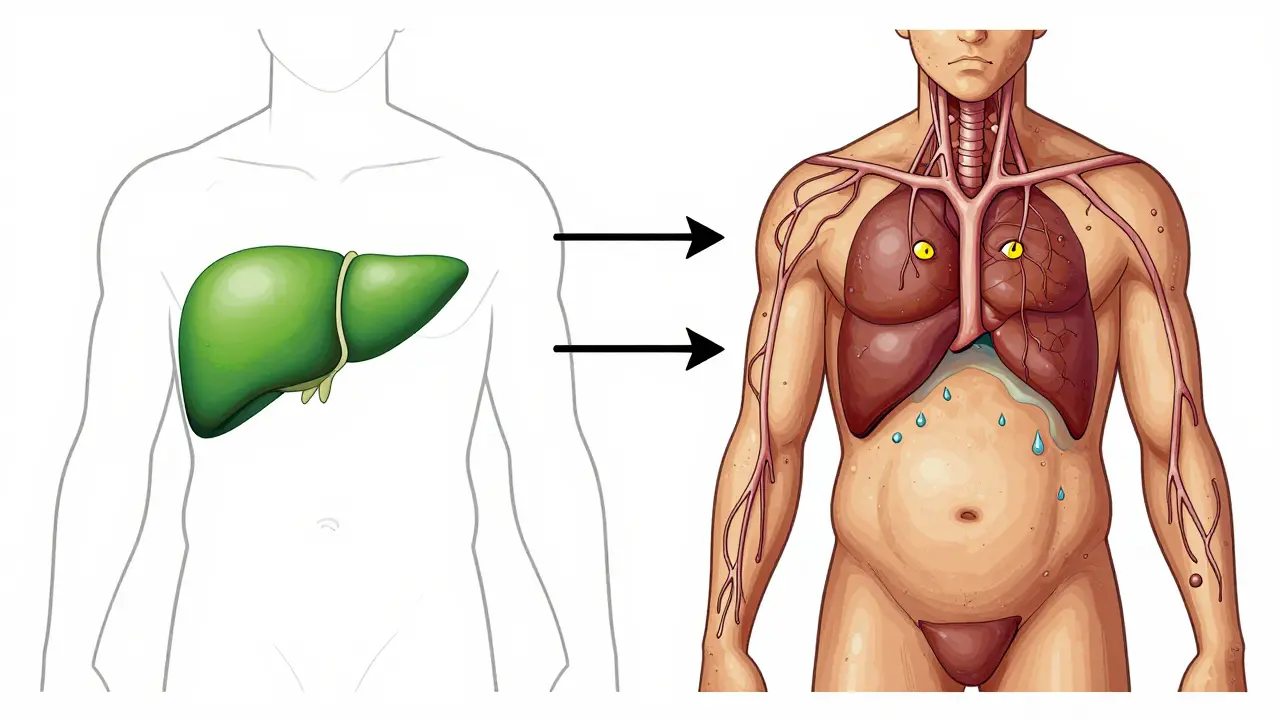
Cirrhosis isn’t a disease on its own. It’s the end result of long-term liver injury. Think of your liver as a factory. It cleans your blood, makes proteins, stores energy, and helps digest food. When something keeps damaging it-alcohol, hepatitis, fat buildup-the liver tries to fix itself. But over time, the repair process goes wrong. Healthy cells die. Scar tissue takes over. The liver becomes lumpy, stiff, and can’t function properly. The term comes from the Greek word for "tawny yellow," which is what a damaged liver looks like under a microscope. By the time scarring is visible on scans or blood tests, it’s already advanced. Around 0.15% to 1% of people worldwide have cirrhosis. In the U.S., it’s one of the top 10 causes of death. And the numbers are rising-not because of more alcohol, but because of fatty liver disease. Non-alcoholic fatty liver disease (NAFLD) now causes nearly a quarter of all cirrhosis cases, surpassing alcohol as the main driver.Compensated vs. Decompensated: The Two Faces of Cirrhosis
Not all cirrhosis is the same. There are two stages, and the difference between them can mean the difference between living well and fighting for your life. In compensated cirrhosis, your liver is scarred, but it’s still doing enough to keep you alive. You might feel tired, or have mild discomfort, but no major symptoms. Many people are diagnosed this way-during a routine blood test that shows high liver enzymes or low platelets. At this stage, your 5-year survival rate is still 80-90%. That’s because you still have time to act. Stop drinking. Lose weight. Treat hepatitis C. These steps can slow or even halt further damage. But if the damage keeps going, you cross into decompensated cirrhosis. That’s when the liver can’t keep up anymore. Symptoms hit hard: fluid builds up in your belly (ascites), your skin and eyes turn yellow (jaundice), you get confused or forgetful (hepatic encephalopathy), or you start vomiting blood from swollen veins in your esophagus (varices). At this point, your survival rate drops to 20-50% within five years. And no medication can reverse it. Doctors use two scoring systems to track how bad it is: Child-Pugh and MELD. Child-Pugh looks at bilirubin, albumin, clotting time, ascites, and brain function. MELD uses creatinine, bilirubin, and INR (a blood clotting measure). A MELD score above 15 means you’re at serious risk of dying without a transplant. A score above 20? You’re on the urgent list.What Causes Cirrhosis?
It’s not just alcohol. While heavy drinking is still a major cause, it’s no longer the #1 one. Here’s what actually leads to cirrhosis today:- Non-alcoholic fatty liver disease (NAFLD/NASH): Fat builds up in the liver, triggers inflammation, and turns into scar tissue. Often linked to obesity, diabetes, and high cholesterol.
- Chronic hepatitis B or C: Viruses that attack the liver. Hepatitis C used to be the top cause, but new antiviral drugs can cure it-before it turns to cirrhosis.
- Alcohol-related liver disease: More than 3 drinks a day for men, 2 for women, over many years. Even if you don’t feel drunk, the damage adds up.
- Autoimmune hepatitis: Your immune system attacks your liver by mistake.
- Primary biliary cholangitis (PBC): A rare disease where bile ducts slowly die, causing backup and scarring.
- Genetic disorders: Like hemochromatosis (too much iron) or Wilson’s disease (too much copper).
How Do You Know If You Have It?
Symptoms are often silent until it’s too late. But here are signs that shouldn’t be ignored:- Constant fatigue-even after sleeping
- Unexplained weight loss or muscle wasting
- Itchy skin
- Swelling in legs or belly
- Dark urine, pale stools
- Confusion, trouble focusing, slurred speech
- Bruising or bleeding easily
- Blood tests: High bilirubin, low albumin, low platelets, high INR.
- Imaging: Ultrasound, MRI, or elastography. Elastography measures liver stiffness-over 12.5 kPa usually means cirrhosis.
- Biopsy: Still the gold standard, but less common now. A tiny needle takes a sample. It’s invasive, but gives the clearest picture.
Can Cirrhosis Be Reversed?
No. Once scar tissue forms, it doesn’t disappear. But here’s the hope: you can stop it from getting worse. If you’re in the compensated stage, quitting alcohol, losing weight, controlling diabetes, or curing hepatitis C can stop progression. Some studies show that with early intervention, fibrosis can even improve slightly. But once you’re in decompensated cirrhosis, no drug on the market can fix the scarring. There’s a new drug, obeticholic acid, approved for PBC-related cirrhosis. And in 2023, a phase 3 trial for simtuzumab showed a 30% reduction in fibrosis progression in NASH patients. But these are still experimental. They don’t reverse cirrhosis-they slow it down. And they’re not for everyone. The truth? The only cure for advanced cirrhosis is a liver transplant.Liver Transplantation: The Only Real Cure
A liver transplant is the only way to fully restore function when cirrhosis has destroyed the organ. In the U.S., about 40% of all liver transplants are for cirrhosis. In 2022, 8,780 transplants were done-but 14,300 people were waiting. That means about 12% of people on the list die each year before getting a liver. The MELD-Na score (an updated version of MELD) determines who gets priority. Higher scores = higher priority. It’s not about how long you’ve been waiting-it’s about how close you are to dying. That’s harsh, but it’s the only fair system when organs are scarce. New tech is helping. Machines that keep donor livers alive and beating outside the body (normothermic perfusion) have increased the number of usable livers by 22%. That’s huge. More livers mean more lives saved. But transplants aren’t a magic fix. You’ll need lifelong immunosuppressants to prevent rejection. You’ll need regular checkups. You’ll need to avoid alcohol, certain foods, and infections. And the cost? Around $350,000 for the surgery alone-not including follow-up care. Still, survival rates are good. Over 80% of patients live at least five years after transplant. Many go back to work, travel, even have kids. One Reddit user wrote: “Six months after transplant, the mental fog finally lifted. I forgot what it felt like to think clearly.”
What Can You Do If You Have Cirrhosis?
If you’ve been diagnosed, here’s what matters most:- Stop alcohol completely. Even one drink can speed up damage.
- Watch your sodium. Less than 2,000 mg a day. No processed food, canned soup, or salty snacks.
- Get vaccinated. Hepatitis A and B, flu, pneumonia. Your immune system is weak.
- Take prescribed meds. Spironolactone for fluid, lactulose for brain fog, antibiotics if you get infections.
- See a liver specialist. Not your general doctor. A hepatologist. They know the latest protocols.
- Join a support group. The American Liver Foundation has nurse navigators you can call at 1-800-GO-LIVER.
The Future: What’s Next?
Researchers are working on ways to reverse scarring. Stem cell therapies, lab-grown liver tissue, and artificial livers are in early human trials. One 2023 study showed hepatocyte transplants (injecting healthy liver cells) lowered MELD scores by 40% in six months. That’s promising. But the biggest change? Personalized medicine. Instead of treating everyone with cirrhosis the same, doctors will soon test for molecular signatures-like which genes are active in your scar tissue. That could tell you if you’re likely to progress fast, or if you’ll respond to a new drug. For now, though, the best defense is early detection. If you’re overweight, diabetic, or have a history of heavy drinking, get your liver checked. A simple ultrasound and blood test could save your life.Can cirrhosis be reversed with diet and exercise?
Diet and exercise can stop cirrhosis from getting worse, especially in the early (compensated) stage. Losing weight, cutting sugar, and avoiding alcohol can reduce fat in the liver and lower inflammation. But once scar tissue has formed, it doesn’t go away. No amount of salads or running will undo the scarring. The goal is to prevent further damage and avoid progression to liver failure.
Is a liver transplant the only cure for cirrhosis?
Yes, for advanced cirrhosis, a liver transplant is the only cure. Medications can manage symptoms and slow progression, but they can’t remove scar tissue or restore full liver function. Transplant replaces the damaged liver with a healthy one, allowing normal function to return. Survival rates are high-over 80% at five years-but it requires lifelong medication and strict follow-up care.
What are the signs that cirrhosis is getting worse?
Signs of worsening cirrhosis include swelling in the belly or legs, yellowing of the skin or eyes, confusion or memory problems, vomiting blood, black or tarry stools, and extreme fatigue. These mean the liver is failing and you’ve entered decompensated cirrhosis. These are medical emergencies. Call your doctor immediately if you notice any of these.
Can you live a normal life with cirrhosis?
Yes-if it’s caught early. Many people with compensated cirrhosis live for decades with no major symptoms, as long as they avoid alcohol, manage their weight, and follow their doctor’s advice. Even after a transplant, many return to work, travel, and normal activities. But it requires discipline: regular checkups, medication, and lifestyle changes. It’s not a free pass-it’s a lifelong commitment.
How do you get on the liver transplant list?
You need a referral from your doctor to a transplant center. There, you’ll go through a full evaluation: blood tests, imaging, heart and lung checks, mental health screening, and social support assessment. If approved, your MELD-Na score determines your place on the list. Higher scores mean higher priority. You can be listed at multiple centers to increase your chances. But you must stay healthy enough to receive a transplant-no alcohol, no smoking, no drug use.

15 Comments
Becky Baker
December 26 2025
They say cirrhosis is silent until it’s too late? Yeah, well my uncle ignored his fatty liver for 10 years because he thought ‘I don’t drink much’ - turns out soda and pizza are just as bad. Now he’s on the transplant list and they won’t even take him because he’s still got 20 lbs to lose. Wake up, people.
Natasha Sandra
December 26 2025
OMG this is so important 😭 I just got my bloodwork back and my ALT was sky-high… I cut out sugar, started walking 30 mins a day, and I swear I already feel less foggy. You guys, your liver is a WORKHORSE. Treat it like your best friend, not your dumpster 😘
Erwin Asilom
December 28 2025
The data presented here is accurate and well-sourced. Non-alcoholic fatty liver disease has surpassed alcohol as the leading etiology of cirrhosis in the United States since 2018, per CDC and AASLD guidelines. Early intervention through dietary modification and metabolic management significantly reduces fibrosis progression. I recommend HbA1c, FibroScan, and lipid panel screening for all patients over 40 with BMI >25.
Sumler Luu
December 29 2025
I appreciate how this breaks it down without fearmongering. My mom was diagnosed with compensated cirrhosis last year. She’s on spironolactone, avoids salt like it’s poison, and sees her hepatologist every three months. She’s still gardening, still baking pies. It’s not a death sentence - just a serious lifestyle update.
Brittany Fuhs
December 29 2025
Of course the ‘experts’ downplay alcohol. It’s not the #1 cause anymore? Funny how the same people who blame capitalism for everything suddenly want to excuse poor choices with ‘NAFLD’. If you’re eating like a college freshman and drinking Diet Coke like water, don’t act surprised when your liver turns to concrete.
Sophia Daniels
December 30 2025
Let me be blunt: if you’re over 35, overweight, and still eating processed carbs like they’re going out of style - you’re already on the path to liver hell. And no, ‘I work out’ doesn’t cancel out 4 Twinkies a day. Your liver isn’t a trash compactor. It’s a sacred temple. And you? You’re the vandal with a soda can in one hand and a bag of chips in the other. Wake. Up.
Nikki Brown
December 31 2025
So many people think ‘I don’t drink’ means they’re safe. Honey, your 3pm latte with 3 pumps of syrup? That’s your new vodka. Your liver doesn’t care if it’s from a bar or a Starbucks. You’re not ‘healthy’ because you run marathons - you’re healthy if you stop feeding your body poison disguised as food. I’m not judging. I’ve been there.
Peter sullen
December 31 2025
It is imperative to underscore the significance of the MELD-Na scoring system as a statistically validated, objective metric for determining transplant prioritization. Furthermore, the advent of normothermic machine perfusion technology represents a paradigm shift in organ preservation efficacy, increasing graft viability by 22% according to the 2023 Journal of Hepatology meta-analysis. These advancements, while promising, remain underutilized in community hospitals.
Steven Destiny
January 2 2026
STOP WAITING. If you’ve got diabetes, obesity, or a family history - get your liver checked TODAY. Not next month. Not when you ‘feel worse.’ Right now. Your liver doesn’t ask for permission before it fails. You think you’re invincible? You’re not. I lost my brother at 42 because he ‘didn’t have time.’ Don’t be him.
Fabio Raphael
January 2 2026
I’ve been watching my dad go through this. He’s in compensated stage, still working, still laughing. But he’s scared. He doesn’t talk about it much. This post made me realize how little people understand - even doctors sometimes miss it. I’m taking him to a hepatologist next week. Maybe if more people knew this stuff, fewer families would be blindsided.
Amy Lesleighter (Wales)
January 3 2026
your liver dont care if you’re rich or poor. it just wants you to stop eating trash and drink water. if you do that early, it can heal a bit. if you wait? too late. no magic pills. just choices. simple.
Rajni Jain
January 5 2026
in india, most people dont even know what fatty liver is. they think only drunks get liver problems. my cousin had it at 28 - she was skinny, ate healthy, but drank too much juice. we got her tested and changed everything. now she’s fine. pls spread this message. not just in usa.
sakshi nagpal
January 5 2026
The implications of non-alcoholic steatohepatitis as the predominant etiological factor in cirrhosis necessitate a reevaluation of public health policy and clinical screening protocols. The confluence of metabolic syndrome, dietary fructose overload, and sedentary lifestyles constitutes a silent pandemic. Proactive intervention, rather than reactive management, must be prioritized by healthcare systems globally.
Sandeep Jain
January 7 2026
my uncle died from this. no one knew he had it till he collapsed. he was 52. he ate chips and soda every day. he thought he was fine because he didn’t drink. pls tell people. this is real.
roger dalomba
January 8 2026
So let me get this straight. The only cure is a transplant… which requires you to be healthy enough to qualify… which requires you to change your life… but you’re too lazy to do it until you’re dying. Classic.