Learn how consistent vitamin K intake stabilizes warfarin therapy, improves INR control, and reduces complications with practical diet tips and tools.
Dietary Consistency: What It Means and Why It Matters for Medication Safety
When you hear dietary consistency, the regular pattern of food intake in terms of texture, timing, and nutritional content that affects how drugs are absorbed in the body. Also known as eating patterns, it isn’t just about eating healthy—it’s about eating the same way every day so your meds work the way they’re supposed to. If you skip breakfast one day and eat a big fatty meal the next, that change can mess with how your body handles your prescription. It’s not magic. It’s chemistry.
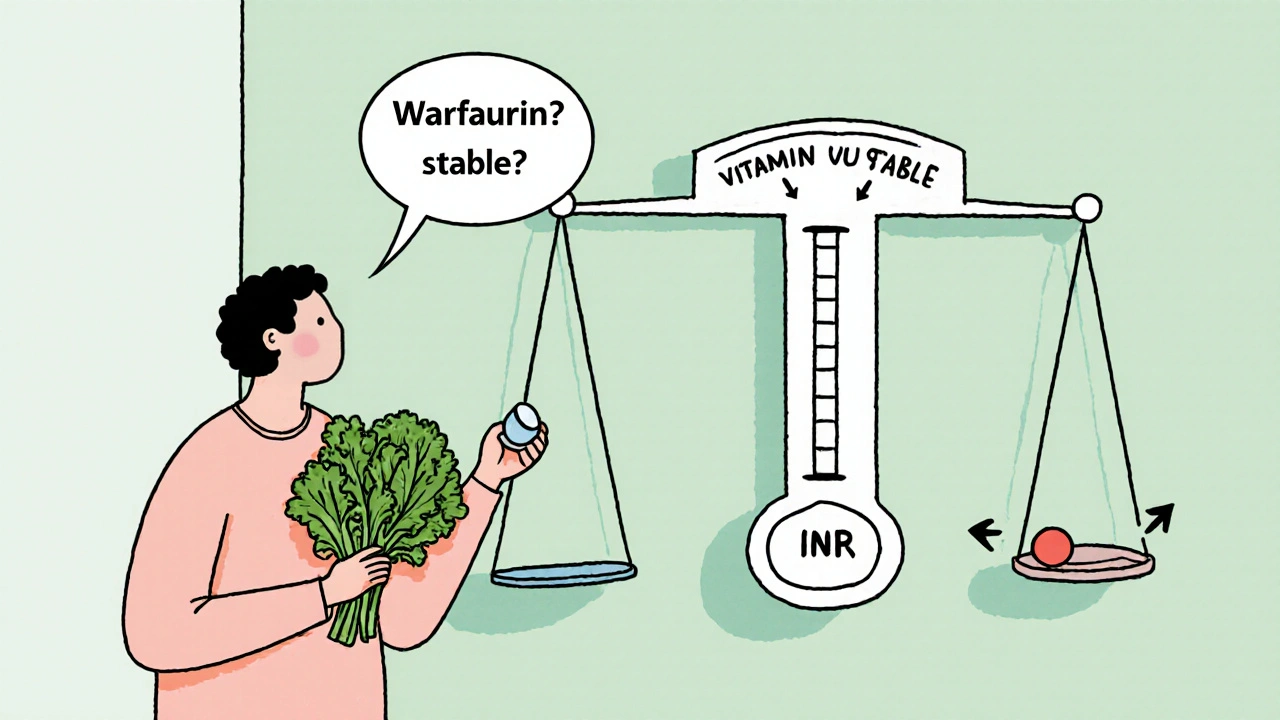
Take warfarin, a blood thinner that reacts strongly to vitamin K levels in food. If you eat lots of spinach one week and almost none the next, your INR levels swing. That’s dangerous. Same with thyroid meds, like levothyroxine, which absorb poorly if taken with coffee, calcium, or high-fiber meals. Even small shifts—like switching from oatmeal to toast for breakfast—can make your dose less effective. Your body doesn’t care if you’re busy or tired. It just reacts to what’s in your stomach.
It’s not just about vitamins or fiber. food-drug interactions, how meals change the way medicines enter your bloodstream happen with common drugs like antibiotics, blood pressure pills, and even antidepressants. Grapefruit juice? It can turn a safe dose of statins into a toxic one. High-fat meals can delay or boost absorption of some ED meds like tadalafil or vardenafil. Even something as simple as drinking milk with your doxycycline can stop it from working. These aren’t rare cases. They’re everyday risks.
People often think if they take their pill with water, they’re fine. But water doesn’t fix inconsistent eating. If you’re on chemo like capecitabine, your mouth sores get worse if you eat spicy or acidic foods on some days and soft meals on others. Your gut doesn’t get a break. Same with people managing diabetes—blood sugar swings from inconsistent meals make insulin dosing a guessing game. Dietary consistency isn’t about being perfect. It’s about being predictable.
Pharmacists don’t just ask if you take your meds. They ask what you eat. Why? Because nutrient interactions, how vitamins, minerals, and fats compete with or block drug absorption are real. Iron supplements can block thyroid meds. Magnesium can reduce antibiotics. Even protein intake affects how some drugs bind in your blood. You don’t need to count calories. You need to keep your routine steady.
Look at the posts here. You’ll find guides on how to safely buy generic warfarin, how lisinopril causes coughs, how capecitabine triggers mouth sores, and how thyroid meds interact with food. They all tie back to one thing: your daily eating habits. No pill works the same if your diet changes every day. The goal isn’t to eat bland food forever. It’s to find a rhythm that lets your meds do their job—without surprises.
What you eat matters more than you think. And if you’re on more than one prescription, your plate is part of your treatment plan. The articles below show you exactly how food, timing, and texture affect your meds—so you can avoid side effects, save money on failed treatments, and stay in control.