When women start experiencing hot flashes, night sweats, or mood swings during menopause, hormone therapy can make a real difference. But not all hormone treatments are the same. The right combination depends on your body, your history, and what you’re trying to avoid as much as what you’re trying to fix. Many women assume hormone therapy means taking one pill every day - but that’s only one option. There are different types of combinations, delivery methods, and generic versions that can change everything - from your risk of blood clots to whether you’ll have monthly bleeding.
Why Combination Therapy Matters
If you still have your uterus, you can’t take estrogen alone. It’s not safe. Estrogen makes the lining of your uterus grow. Left unchecked, that growth can turn into cancer. That’s why doctors combine estrogen with progestogen - a synthetic or natural form of progesterone - to protect the uterine lining. This isn’t optional. It’s a medical necessity. For women who’ve had a hysterectomy, estrogen-only therapy is fine. But for the rest, the combination is non-negotiable. The key is choosing the right kind of combination and the right way to take it.Two Main Types of Combined HRT
There are two main ways to combine estrogen and progestogen: sequential and continuous. Sequential combined HRT is for women who are still having periods or just stopped recently. You take estrogen every day, then add progestogen for the last 10 to 14 days of the month. This mimics your natural cycle. You’ll likely get a withdrawal bleed - kind of like a period - each month. It’s designed for women in perimenopause or early menopause who still have some hormonal rhythm left. Continuous combined HRT is for women who haven’t had a period for a full year. You take both hormones every single day, with no breaks. There’s no monthly bleed. This is the go-to for most postmenopausal women. It’s simpler, and studies show it lowers the risk of colon cancer by about 18% and type 2 diabetes by 21%, based on data from the Women’s Health Initiative. Choosing between them isn’t about preference - it’s about your body’s stage. Taking continuous HRT too early can cause unpredictable bleeding. Taking sequential HRT after a year without periods might not control symptoms as well.Generic Options You Can Actually Use
Most hormone therapy prescriptions today are generic. That’s because they’re cheaper - sometimes much cheaper - than brand names. And they work just as well. Common generic estrogens include:- Conjugated estrogens - 0.3mg, 0.45mg, or 0.625mg tablets. These are derived from horse urine and have been around for decades.
- Estradiol - 0.5mg or 1mg tablets. This is the same hormone your body naturally makes. Many doctors prefer it because it’s more bioidentical.
- Medroxyprogesterone acetate - 2.5mg, 5mg, or 10mg tablets. This is a synthetic progestin. It’s widely used but linked to slightly higher breast cancer risk.
- Micronized progesterone - 100mg or 200mg capsules. This is natural progesterone, made from plant sources. It’s gentler on the breasts and may lower cancer risk compared to synthetic versions.
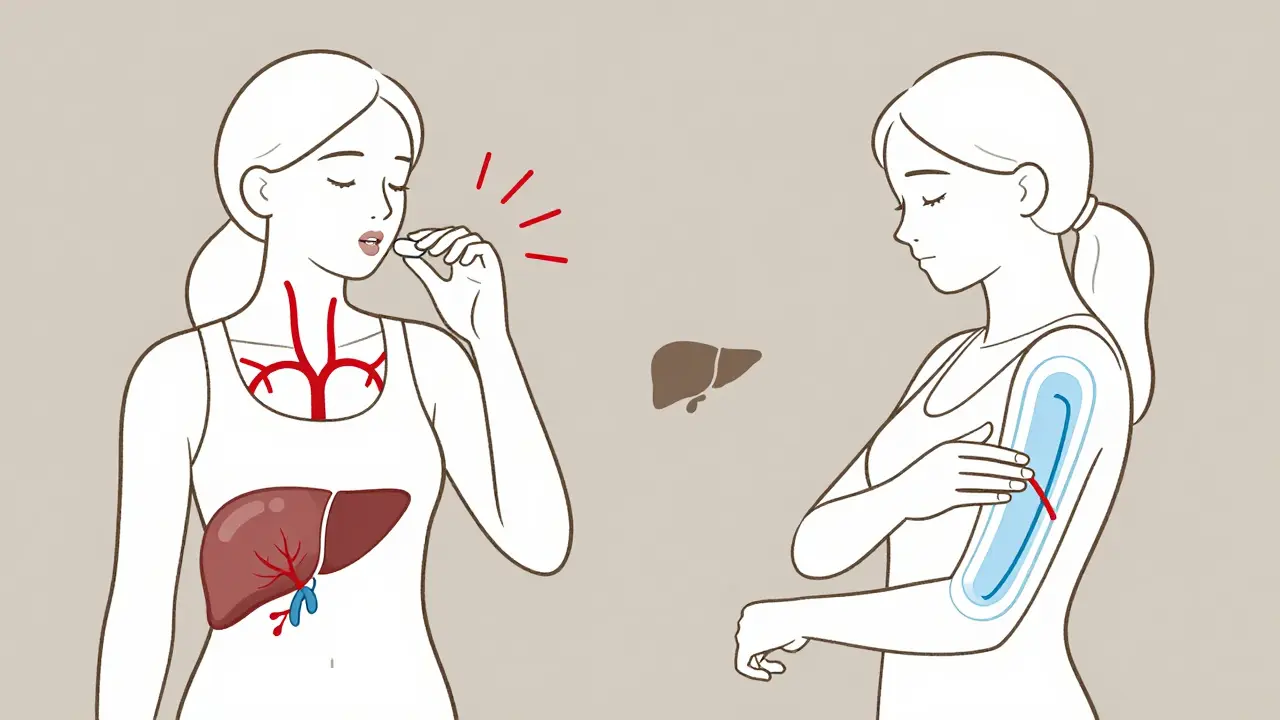
Delivery Methods: Patches, Gels, and More
How you take your hormones matters as much as what you take. Oral pills are the most common. But they go through your liver first. That’s a problem. The liver reacts by increasing clotting factors. That’s why oral estrogen raises your risk of blood clots by 2 to 3 times compared to skin-based methods. Transdermal options - patches, gels, and sprays - skip the liver. They go straight into your bloodstream. That means:- Lower risk of blood clots
- Lower risk of stroke, especially after age 60
- More stable hormone levels
Who Should Avoid Hormone Therapy?
HRT isn’t for everyone. You should not start it if you have:- A history of breast cancer
- Unexplained vaginal bleeding
- Active liver disease
- History of blood clots, stroke, or heart attack
Long-Term Risks and What the Data Really Says
The biggest fear around HRT is breast cancer. Let’s be clear: the risk is small, but real. Using combined HRT for more than five years increases breast cancer risk by less than 1 in 1,000 women per year. That’s tiny - but it adds up. The risk is higher with synthetic progestins like medroxyprogesterone acetate. With micronized progesterone, the risk is lower - about 1.9% per year versus 2.7% for synthetic versions. Estrogen-only therapy doesn’t raise breast cancer risk much - but again, only if you’ve had a hysterectomy. For women with a uterus, skipping progestogen is dangerous. Heart risks are also tied to delivery method. Oral estrogen increases stroke risk by about 39% in women over 60. Transdermal estrogen doesn’t. That’s why many doctors now recommend patches or gels for older women.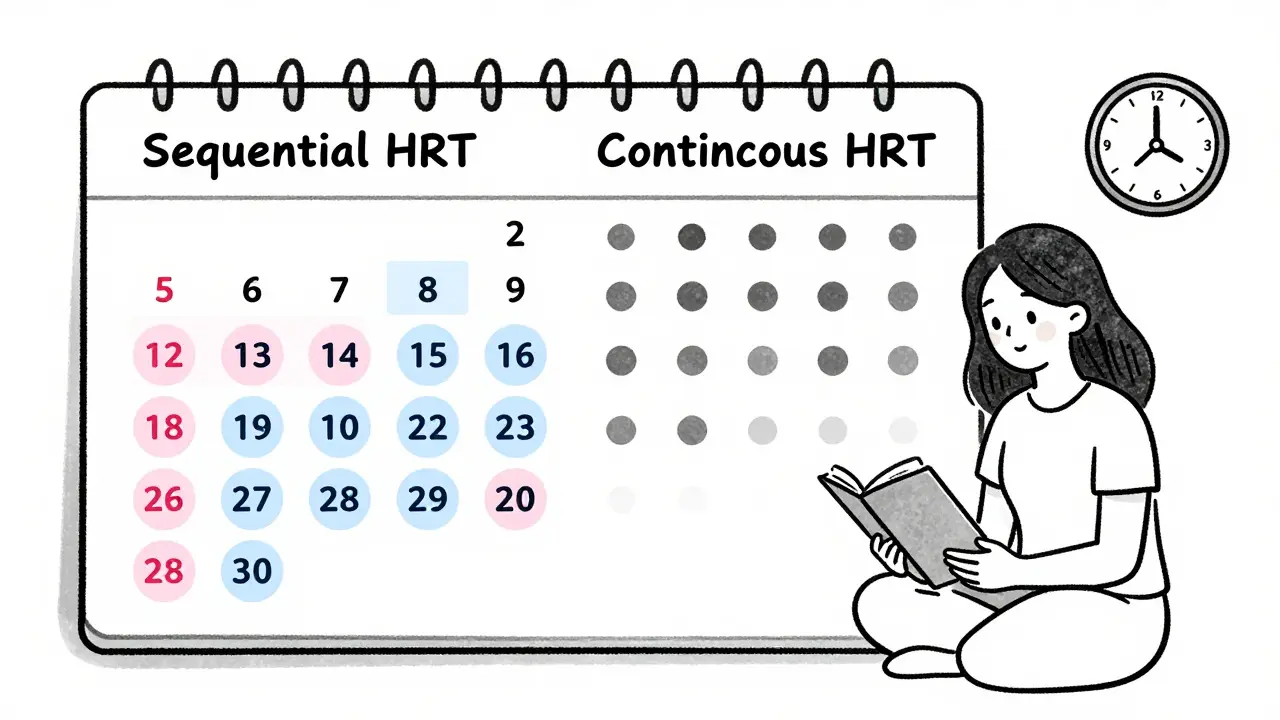
What to Expect When You Start
Most women don’t feel better overnight. It takes 3 to 6 months to find the right dose and delivery method. Side effects like bloating, breast tenderness, or mood swings are common at first. They usually fade. Breakthrough bleeding happens in 15 to 20% of women during the first 6 months - especially with sequential therapy. That’s normal. But if it keeps happening after six months, you need to see your doctor. It could mean the dose is too low, the type of progestogen isn’t right, or something else is going on. Don’t stop because of bleeding. Don’t switch brands because you’re frustrated. Work with your provider. Adjust slowly. Keep a symptom journal. It helps.The Future of Hormone Therapy
New options are coming. In 2023, the FDA approved a new transdermal patch that combines estrogen and progesterone in one patch. Early data suggests it may lower breast cancer risk even more than older combinations. Researchers are also testing tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs). These are designed to give symptom relief without affecting breast or uterine tissue the same way traditional hormones do. But for now, the best tools we have are the ones already here: low-dose, transdermal, generic, and personalized.How to Decide What’s Right for You
Ask yourself these questions:- Have I had a hysterectomy?
- Am I under 60 or within 10 years of my last period?
- Do I have a history of blood clots, stroke, or breast cancer?
- Am I willing to apply a gel daily or change a patch twice a week?
- Can I afford or access transdermal options?
Can I take generic hormone therapy instead of brand-name?
Yes, and most women should. Generic hormone therapies like estradiol tablets, conjugated estrogens, and medroxyprogesterone acetate are just as effective as brand names like Premarin or Provera. They’re tested to meet the same FDA standards. The main difference is cost - generics can be 80% cheaper. Insurance often covers them first. Always ask your pharmacist if a generic is available.
Is transdermal HRT safer than pills?
For most women, yes. Transdermal estrogen - patches, gels, sprays - doesn’t pass through the liver, so it doesn’t trigger the same increase in clotting factors. That means lower risk of blood clots and stroke, especially after age 50. The NHS and European guidelines now recommend transdermal as the first choice for women with risk factors. Oral pills are still fine for younger, healthy women without clotting issues.
Why do I keep bleeding on HRT?
Breakthrough bleeding is common in the first 3 to 6 months, especially with sequential therapy. It’s usually because your body is adjusting to the hormones. If bleeding continues beyond six months, your dose might be too low, or you may need a different type of progestogen. It could also signal an issue like polyps or thyroid problems. Don’t ignore it - get checked.
How long should I stay on hormone therapy?
There’s no fixed rule. Most women take it for 2 to 5 years to manage symptoms. If symptoms return after stopping, you can restart at the lowest dose. Annual reviews are key. If you’re over 60 or have been on it for more than 5 years, your doctor should reassess whether the benefits still outweigh the risks. You don’t need to stay on it for life.
Does HRT cause weight gain?
Not directly. Weight gain during menopause is mostly due to aging, slower metabolism, and changes in fat distribution - not the hormones themselves. Some women feel bloated at first, which can feel like weight gain. Others find that better sleep and fewer hot flashes help them stick to healthy habits. HRT doesn’t cause obesity, but it won’t reverse it either.
Can I use HRT if I have a family history of breast cancer?
It’s complicated. A family history alone doesn’t rule out HRT, but it does mean you need extra caution. If you’re a BRCA carrier or have had breast cancer, estrogen therapy is usually avoided. If you have a distant relative with breast cancer and no personal history, transdermal estrogen with micronized progesterone may be an option - but only after detailed risk assessment. Always talk to a specialist.

11 Comments
Jackie Be
December 19 2025
OMG I started HRT last year and my life changed like literally overnight no more night sweats no more crying over spilled milk i was a mess before now i feel like myself again and yeah i use the gel cause i dont wanna risk clots and my doc said its better anyway
Meina Taiwo
December 21 2025
Generic estradiol and micronized progesterone are equally effective as brand names. Transdermal routes reduce liver metabolism risks. Always confirm dosage with your provider.
Swapneel Mehta
December 23 2025
Interesting breakdown. I’ve been on patches for two years now and the stability is way better than pills. No more mood swings at work. Took a while to find the right combo but totally worth it.
Stacey Smith
December 23 2025
Why are we even talking about this like it’s a choice? If you’re postmenopausal and symptomatic you take HRT. The fearmongering is what’s killing women not the hormones. Wake up.
Jason Silva
December 24 2025
Bro the FDA is just letting Big Pharma push pills because they make more money 😤 Patches are cheaper long term and safer but they don’t want you to know that 🤫💊
Adrian Thompson
December 24 2025
They say 'generic works just as well' but you know what they dont tell you? The fillers are different. I had a bad reaction to one brand of generic estradiol. Turned out it had corn starch. I’m corn allergic. They dont test for that. This is how you get sick. They dont care. Just profit.
Ben Warren
December 25 2025
It is imperative to underscore that the indiscriminate administration of hormone replacement therapy constitutes a profound public health risk, particularly when predicated upon anecdotal efficacy rather than longitudinal, randomized controlled trial data. The Women’s Health Initiative findings remain unequivocal: early initiation is associated with reduced cardiovascular morbidity, yet prolonged exposure-particularly in conjunction with synthetic progestins-elevates neoplastic risk in a dose- and duration-dependent manner. Furthermore, the assumption that transdermal delivery confers universal safety is empirically unfounded; while hepatic first-pass avoidance mitigates thrombotic propensity, it does not eliminate systemic estrogenic activity. Physicians must exercise rigorous patient selection, and patients must be educated regarding the non-negotiable necessity of annual endometrial surveillance, mammographic screening, and lipid profile monitoring. To suggest otherwise is not merely irresponsible-it is negligent.
Hannah Taylor
December 26 2025
you think theyre telling you the truth about clots? wait till you find out what they put in the gel… its not even real progesterone its some lab thing that tricks your body into thinking its safe… i read a guy on a forum who got a tumor after 6 months… they cover it up
Jerry Peterson
December 27 2025
Thanks for laying this out so clearly. I’m from the Midwest and most docs here still push pills. I switched to patches after reading this and my sister in Canada said they’ve been doing this for years. It’s good to see the science catching up.
Teya Derksen Friesen
December 28 2025
As a physician practicing in Vancouver, I can confirm that transdermal HRT is now the first-line recommendation for all patients over 50 with cardiovascular risk factors. The evidence is robust, and patient adherence is higher with gels than pills due to fewer GI side effects. We no longer prescribe oral estrogen to women with a history of migraines or thrombophilia. The paradigm shift is real-and overdue.
mukesh matav
December 30 2025
My mom took HRT for 8 years and she’s 72 and fine. No cancer, no clots. She used the patch and micronized progesterone. Don’t scare people away from help. Everyone’s body is different.