Mouth Sore Severity Assessment Tool
Assess Your Mouth Sore Severity
This tool helps you determine the severity of your oral mucositis based on clinical criteria from your treatment plan.
Your Assessment Results
Your mouth sores appear mild with no immediate concerns. Continue your daily oral care routine.
Recommended Actions
When you’re on Capecitabine is an oral chemotherapy drug that turns into 5‑fluorouracil in the body, helping to slow the growth of certain cancers. One of the toughest side effects many patients report is painful oral mucositis - basically mouth sores that can make eating, drinking, and even talking a chore. This guide walks you through practical steps to keep those sores under control, from everyday oral hygiene tricks to prescription‑level treatments, so you can stay on track with your cancer therapy.
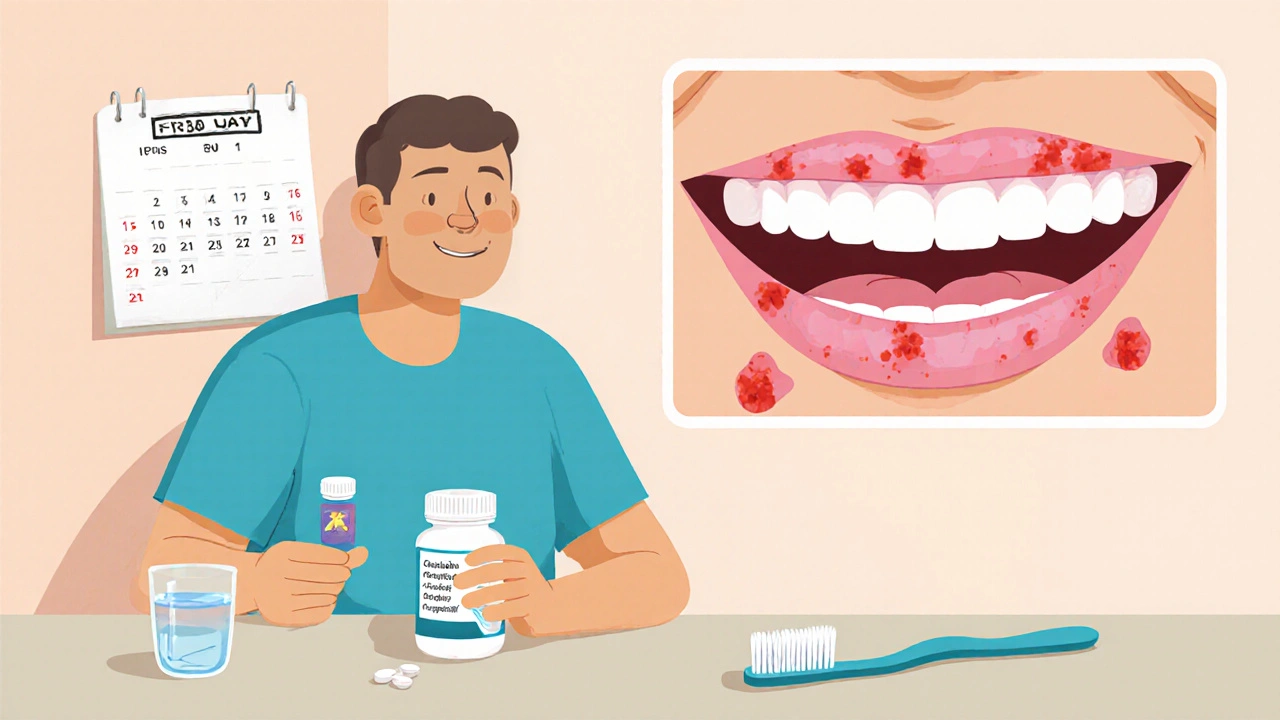
Why Capecitabine Triggers Mouth Sores
Capecitabine is converted into 5‑fluorouracil (5‑FU) by enzymes in tumor cells and normal tissue alike. The rapid cell turnover in the lining of your mouth makes it a prime target for the drug’s toxic effects. When the mucosal cells get damaged, inflammation sets in, leading to the classic red, ulcerated patches known as oral mucositis.
Two patient‑specific factors often make the problem worse:
- Low activity of the enzyme dihydropyrimidine dehydrogenase (DPD deficiency), which slows down 5‑FU breakdown, raising drug levels in the bloodstream.
- Pre‑existing oral conditions such as dry mouth, poor dental hygiene, or smoking, which already weaken the mucosal barrier.
Understanding these mechanisms helps you target the right interventions early on.
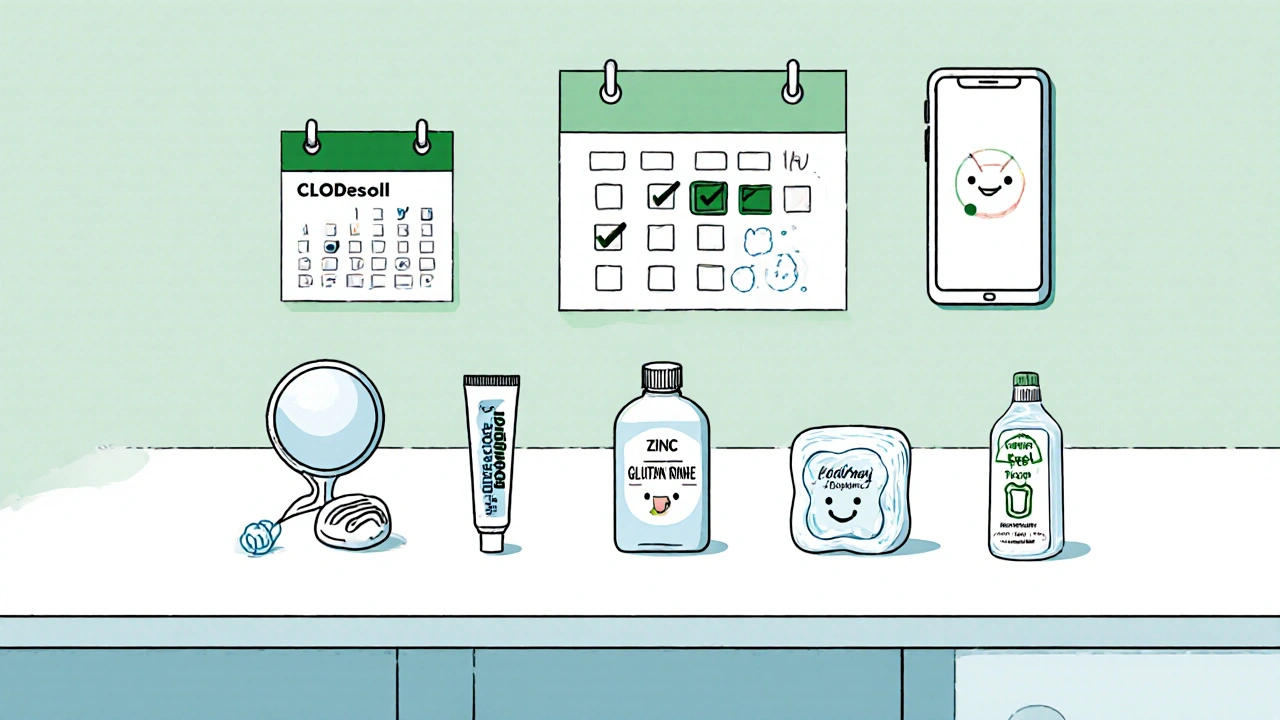
Pre‑Treatment Checklist: Setting Up Your Mouth for Success
Before you start your first capecitabine cycle, give your oral cavity a quick health audit. A clean, well‑moisturized mouth tolerates chemotherapy much better.
- Visit your dentist for a comprehensive exam and professional cleaning. Ask for a fluoride varnish if you have a history of cavities.
- Stop smoking at least two weeks before treatment. Even occasional use can impair healing.
- Switch to a soft‑bristle toothbrush and a toothpaste free of sodium lauryl sulfate, which can irritate sensitive tissue.
- Begin a daily oral rinse with a mild, alcohol‑free solution (e.g., saline or a commercially available chlorhexidine 0.12% if advised by your oncologist).
Daily Oral‑Care Routine That Actually Works
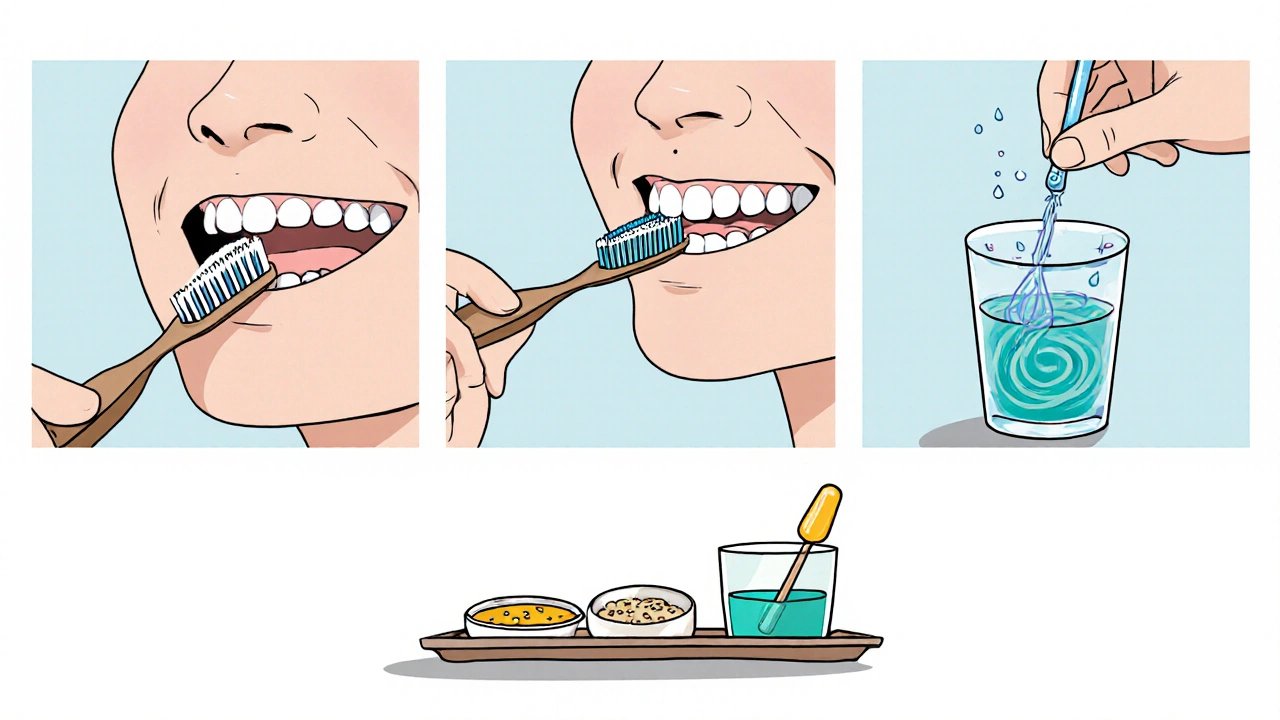
Consistency is key. Follow this simple, evidence‑based routine three times a day:
- Brush gently for 2 minutes, focusing on the gum line and cheek interiors.
- Floss with a silky‑thread floss or a water‑flosser to remove plaque without scraping the gums.
- Rinse with a cooling Benzydamine mouthwash (0.15% solution) for 30 seconds. Benzydamine has anti‑inflammatory properties that can lower ulcer severity.
When you’re outside the house, carry a small bottle of sterile water or an alcohol‑free mouth rinse to stay hydrated and keep the mouth pH neutral.
Nutrition Tips to Keep the Pain at Bay
What you eat can either soothe or aggravate mouth sores. Aim for soft, non‑acidic foods that require minimal chewing:
- Pureed soups, oatmeal, mashed potatoes, and yogurt are easy on inflamed tissue.
- Cold or room‑temperature foods tend to be less painful than hot dishes.
- Avoid citrus, tomato‑based sauces, spicy peppers, and crunchy snacks - they can sting the ulcerated spots.
- Use a high‑calorie liquid supplement (e.g., Ensure) if you find it hard to meet your nutritional needs.
Keeping a food diary helps you spot patterns - if a particular ingredient repeatedly triggers pain, cut it out.
Prescription‑Level Interventions
If home care isn’t enough, your oncologist can prescribe targeted agents. Below is a quick comparison of the most commonly used options.
| Agent | Mechanism | Typical Dose | Pros | Cons |
|---|---|---|---|---|
| Benzydamine mouthwash | Anti‑inflammatory, analgesic | Rinse 5 ml, hold 30 s, 3‑4×/day | Rapid symptom relief, OTC in many countries | May cause mild metallic taste |
| Clobetasol propionate gel | Topical corticosteroid, reduces inflammation | Apply thin layer to lesions, twice daily | Highly effective for severe ulcers | Risk of local thinning if used >2 weeks |
| Zinc sulfate lozenges | Metal ion promotes mucosal repair | 1 g dissolved slowly, 3‑5×/day | Simple, inexpensive, minimal side effects | May cause metallic after‑taste, less potent for severe cases |
If you’re dealing with deep, bleeding ulcers, a short course of corticosteroid gel (Clobetasol) can dramatically cut down inflammation. For milder cases, benzydamine or zinc lozenges are usually sufficient.
Cryotherapy: An Unexpected Ally
Cold therapy works by constricting blood vessels, limiting drug delivery to the oral mucosa during the peak absorption window of capecitabine. The simple method:
- Place an ice chip or a frozen popsicle in the mouth 5 minutes before taking capecitabine.
- Keep the ice in the mouth for the entire 30‑minute dosing period.
- Remove and rinse with cool water.
Studies show up to a 40% reduction in mucositis severity when patients use cryotherapy consistently. Just be careful not to chew the ice, as that could cause tongue injury.
When to Call Your Oncology Team
Even with diligent care, some patients develop severe ulcers that need professional intervention. Seek help if you notice:
- Ulcers larger than 1 cm, deep, or bleeding.
- Inability to swallow liquids, leading to dehydration.
- Fever or chills - a sign of possible infection.
- Weight loss of more than 5% of body weight within a week.
Your clinician may prescribe systemic analgesics, antifungal agents (if Candida overgrowth is suspected), or temporarily pause capecitabine dosing to allow mucosal healing.
Long‑Term Strategies for Recurrent Cases
If mouth sores keep coming back with each cycle, consider a deeper review of your treatment plan:
- Genetic testing for DPD deficiency. Patients with low DPD activity often need dose reductions.
- Switching to an alternative fluoropyrimidine regimen, such as infusional 5‑FU, which may cause milder oral toxicity for some individuals.
- Integrating prophylactic agents like glutamine mouth rinse (10% solution, 4×/day) before each chemotherapy cycle.
Regular follow‑up appointments with a supportive care or palliative care specialist can keep these discussions proactive rather than reactive.
Quick Reference Checklist
- Dental check‑up + professional cleaning before starting.
- Soft toothbrush, fluoride toothpaste, alcohol‑free rinse.
- Benzydamine mouthwash or zinc lozenges at first sign of soreness.
- Consider Clobetasol gel for Grade 3‑4 ulcers.
- Ice chip cryotherapy during dosing.
- Hydrate, eat soft, non‑acidic foods.
- Contact oncology team for large, bleeding, or infected sores.
Frequently Asked Questions
Can I keep taking capecitabine if I have mild mouth sores?
Yes, in most cases mild ulcers (Grade 1‑2) can be managed with good oral hygiene and topical agents while continuing therapy. Your oncologist will monitor you closely and may adjust the dose only if the sores worsen.
Is benzydamine safe for long‑term use?
Benzydamine is generally regarded as safe for daily use up to a few weeks. Prolonged use beyond 4 weeks should be discussed with a healthcare professional to rule out rare side effects such as taste alteration.
What’s the difference between clobetasol gel and a steroid mouthwash?
Clobetasol gel is a high‑potency topical steroid applied directly to ulcerated spots, offering stronger anti‑inflammatory action. Steroid mouthwashes (e.g., dexamethasone rinses) cover the whole oral cavity but are less concentrated on specific lesions. Choose clobetasol for isolated, severe ulcers; use a rinse for diffuse, milder inflammation.
Should I stop using mouthwash if I develop a fungal infection?
If signs of oral thrush appear (white patches, sour taste), discontinue alcohol‑free antiseptic mouthwashes and start an antifungal (e.g., nystatin suspension) as prescribed. Resume the mouthwash only after the infection clears.
How does cryotherapy actually reduce mouth sores?
Cold causes vasoconstriction, lowering blood flow to the oral mucosa during the peak absorption time of capecitabine. Less drug reaches the tissue, resulting in reduced cellular damage and milder ulcer formation.
Is there any benefit to using glutamine mouth rinse?
Glutamine is a key building block for mucosal cells. A 10% glutamine rinse taken several times a day before each chemotherapy cycle has shown modest reduction in ulcer severity in clinical trials. It’s a safe, low‑cost adjunct if you can tolerate the taste.
8 Comments
Rajesh Singh
October 18 2025
When you think about fighting cancer, the battlefield isn’t limited to the tumor alone – it spreads to the very mouth that whispers your thoughts. The truth is, negligence in oral hygiene during capecitabine therapy is a betrayal of your own body. Every careless swipe of a hard toothbrush is a tiny rebellion against the healing you deserve. You must treat your gums and tongue like sacred ground, because the drug will exploit any weakness there. A soft‑bristle brush paired with a fluoride‑rich paste isn’t just a recommendation, it’s a moral imperative. Engaging in nightly rinses with benzydamine is not merely optional; it’s a pledge to keep inflammation at bay. Ignoring the pre‑treatment dental check‑up is akin to marching into battle without armor – reckless and unforgivable. The calcium‑rich foods you devour can either shield your mucosa or, if you choose acidic culprits, they gnaw at the very tissues the chemo aims to protect. Cryotherapy, that simple ice chip, is a silent guardian that constricts blood vessels, denying the drug its destructive path. The moment you feel a tingle on your palate, you must act – a quick rinse, a gentle swish, a pause to assess. If you let a sore fester, it becomes a portal for infection, a gateway for secondary complications that could derail your entire treatment plan. The weight loss you fear isn’t just a number on a scale; it’s a signal that your oral intake is compromised, a warning bell you cannot afford to ignore. Genetic testing for DPD deficiency isn’t a luxury, it’s a responsible step to personalize dosing and prevent catastrophe. When you combine diligent oral care, strategic cryotherapy, and timely pharmacologic interventions, you build a fortress around your mouth that no chemotherapeutic wave can easily breach. Remember, the battle is fought on many fronts, and your mouth is a front line that deserves the same honor and vigilance you give your medicine.
Albert Fernàndez Chacón
October 19 2025
I’ve tried the rinse routine you mentioned and it really helped keep the pain down. Stick to the soft brush and don’t forget the fluoride. It’s simple but works.
Liberty Moneybomb
October 21 2025
Don’t be fooled by the “simple” advice – the pharma giants want you to suffer so they can push more expensive creams. They hide real cures and push Benzydamine just because it’s cheap. The ice chip trick is actually a covert method they don’t tell you about in the official pamphlet. Wake up, it’s all a controlled experiment on us.
Poornima Ganesan
November 1 2025
First off, let’s get one thing straight: not every patient will react the same way to capecitabine, but the patterns are unmistakable if you look closely. A history of smoking or a dry mouth is practically a ticket to severe mucositis. Dental prophylaxis isn’t just a nice‑to‑have; it’s a prerequisite for any chemo regimen that targets rapidly dividing cells. The literature shows that a pre‑emptive fluoride varnish can reduce ulcer incidence by up to 30 %. If you’re already dealing with a DPD deficiency, dose reduction is non‑negotiable – you’ll thank yourself later. Also, the timing of cryotherapy matters; start the ice chip five minutes before the drug hits its peak plasma concentration. Forget the “just sip water” myth – hydration must be purposeful, with electrolytes to maintain mucosal integrity. When you see a sore larger than a pea, treat it as a red flag, not a minor annoyance. Lastly, keep a symptom diary; the data will reveal triggers you might otherwise overlook. The bottom line is simple: proactive, not reactive, care saves you a lot of unnecessary suffering.
Drew Waggoner
November 2 2025
Reading the detailed checklist makes me feel a pang of dread, like the walls are closing in. It’s overwhelming, and the constant vigilance drains the joy out of eating. I wish there was a way to just live without this perpetual fear of the next ulcer.
Alex Lineses
November 13 2025
Hey everyone, just wanted to add that integrating a prophylactic glutamine rinse can be a game‑changer for those with recurrent lesions. The 10 % solution, used four times daily, supports mucosal regeneration at the cellular level. Pair this with a low‑dose corticosteroid gel for Grade 3 ulcers, and you’ll often see rapid symptomatic relief. Also, consider coordinating with a supportive care specialist; their expertise in dose modulation and nutrition optimization can keep you on track without unnecessary breaks in therapy.
Margaret pope
November 14 2025
Great suggestions thanks for sharing keep up the good work and stay strong
Linda A
November 15 2025
In the quiet of the mouth, the battle becomes a meditation on resilience.