Getting the right dose of medicine for a child isn’t about age. It’s not about how tall they are. It’s not even about what the label says for "children." It’s about their weight. One wrong number - a misplaced decimal, a confused pound-to-kilo conversion - can turn a safe dose into a dangerous one. In pediatric care, weight-based dosing isn’t just standard practice. It’s the only safe way to give medications to children.
Why Weight Matters More Than Age
A 2-year-old can weigh anywhere from 9 to 15 kilograms. That’s a 67% difference in body mass. If you gave both kids the same dose based on age, the lighter child might get too little - the medicine won’t work. The heavier one might get too much - and risk serious side effects like liver damage, seizures, or even death. That’s why age-based dosing charts are outdated and dangerous. The gold standard today is milligrams per kilogram (mg/kg). Every major hospital system - from Children’s Hospital Colorado to St. Louis Children’s Hospital - uses this method. The Institute for Safe Medication Practices confirms that 35% of all pediatric medication errors come from incorrect dosing, and nearly 80% of those are due to simple weight conversion mistakes.The Three-Step Formula for Safe Dosing
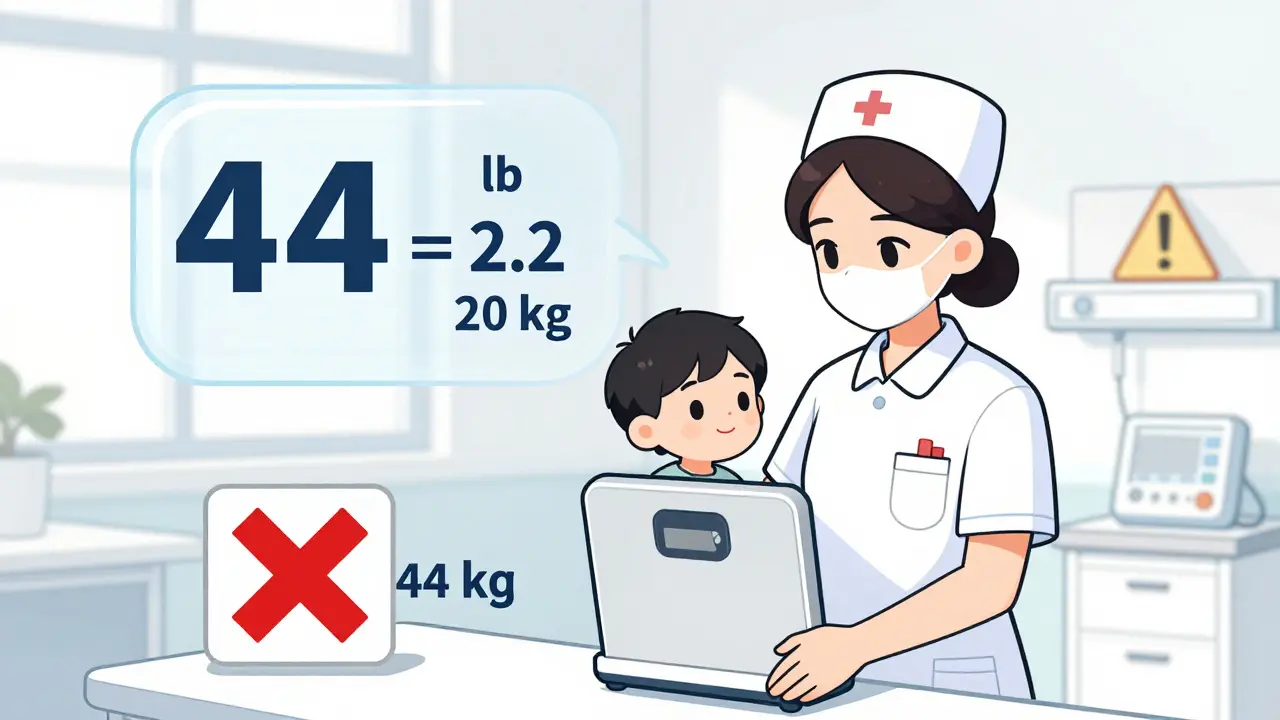
There are three steps to get it right every time. Skip one, and you risk harm.- Get the weight in kilograms. In the U.S., scales often show pounds. You must convert. Use 1 kg = 2.2 lb. No exceptions. If a child weighs 44 pounds, divide by 2.2: 44 ÷ 2.2 = 20 kg. Never estimate. Always use the most accurate scale available.
- Multiply by the prescribed dose. If the order says 15 mg/kg for amoxicillin, and the child weighs 20 kg: 15 × 20 = 300 mg total per day.
- Divide by frequency. If the dose is given twice a day: 300 mg ÷ 2 = 150 mg per dose.
When Weight Isn’t Enough: Body Surface Area
For some drugs - especially chemotherapy agents like vincristine or immunosuppressants - weight alone isn’t precise enough. These drugs have a narrow safety window. Too little, and the treatment fails. Too much, and it kills healthy cells. In these cases, doctors use body surface area (BSA), measured in square meters (m²). The Mosteller formula is the standard: √(height in cm × weight in kg ÷ 3600). For a child who is 97 cm tall and weighs 16.8 kg: √(97 × 16.8 ÷ 3600) = √0.453 = 0.67 m². The dose is then calculated as mg per m². This method is complex and rarely used outside of oncology or critical care. But if you’re caring for a child on chemo, this isn’t optional. It’s life-saving.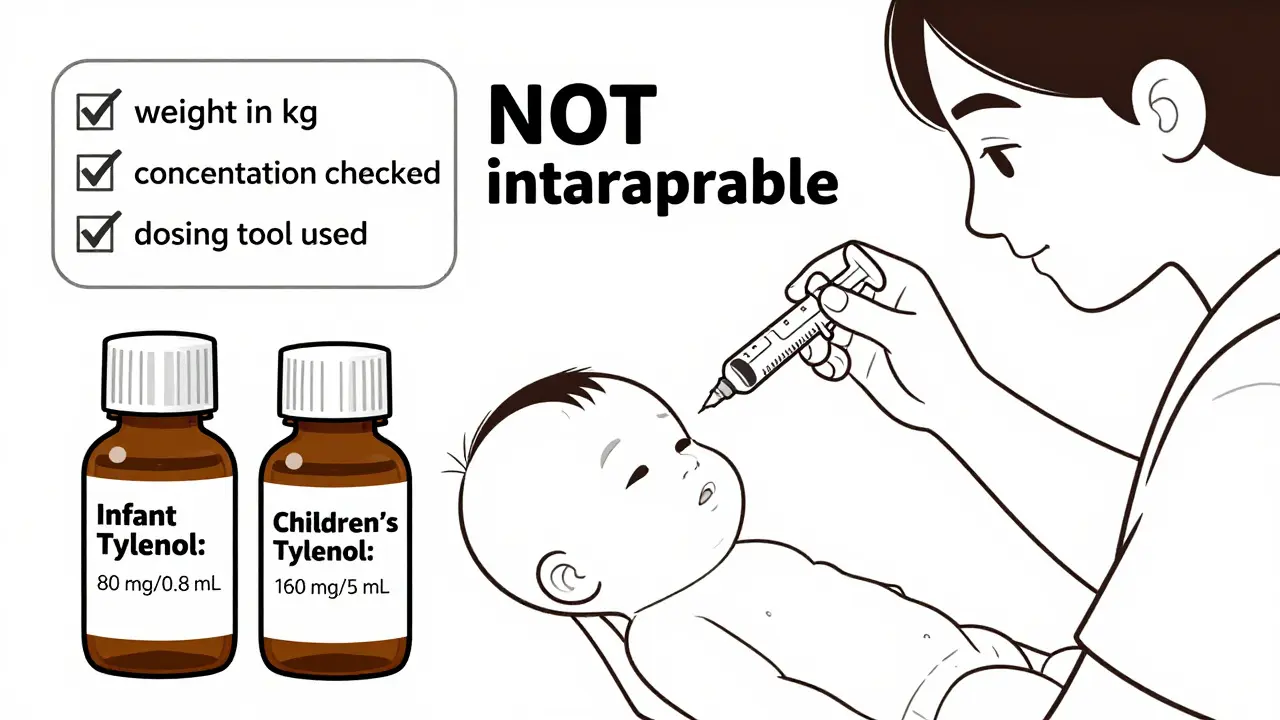
Common Mistakes That Put Kids at Risk
Even experienced nurses and parents make these errors - and they’re deadly.- Confusing mg/kg/day with mg/kg/dose. An order saying “10 mg/kg/d” means the total daily dose. If given twice daily, each dose is 5 mg/kg. Many assume it’s per dose - and give double the intended amount.
- Unit conversion errors. 44 pounds isn’t 44 kilograms. That’s a 10-fold overdose. This is the #1 error in pediatric hospitals.
- Ignoring concentration. A bottle labeled “100 mg/mL” is 10 times stronger than “10 mg/mL.” Using the wrong one can be fatal.
- Not double-checking. Leading hospitals require two clinicians to verify every weight-based dose. No exceptions.
What About Over-the-Counter Medicines?
Parents often think OTC meds are safe. They’re not. Acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) are the most common causes of pediatric poisonings - and most are due to dosing errors. The American Academy of Pediatrics says: never use a kitchen spoon. Always use the syringe or cup that comes with the medicine. And never mix formulations. Infant drops are concentrated. Children’s liquid is diluted. One teaspoon of infant drops equals four teaspoons of children’s liquid. Get them confused, and you overdose. Also, don’t give Benadryl to children under 2 years unless a doctor says so. It can cause seizures, breathing problems, or coma in very young kids - even at “correct” weight-based doses.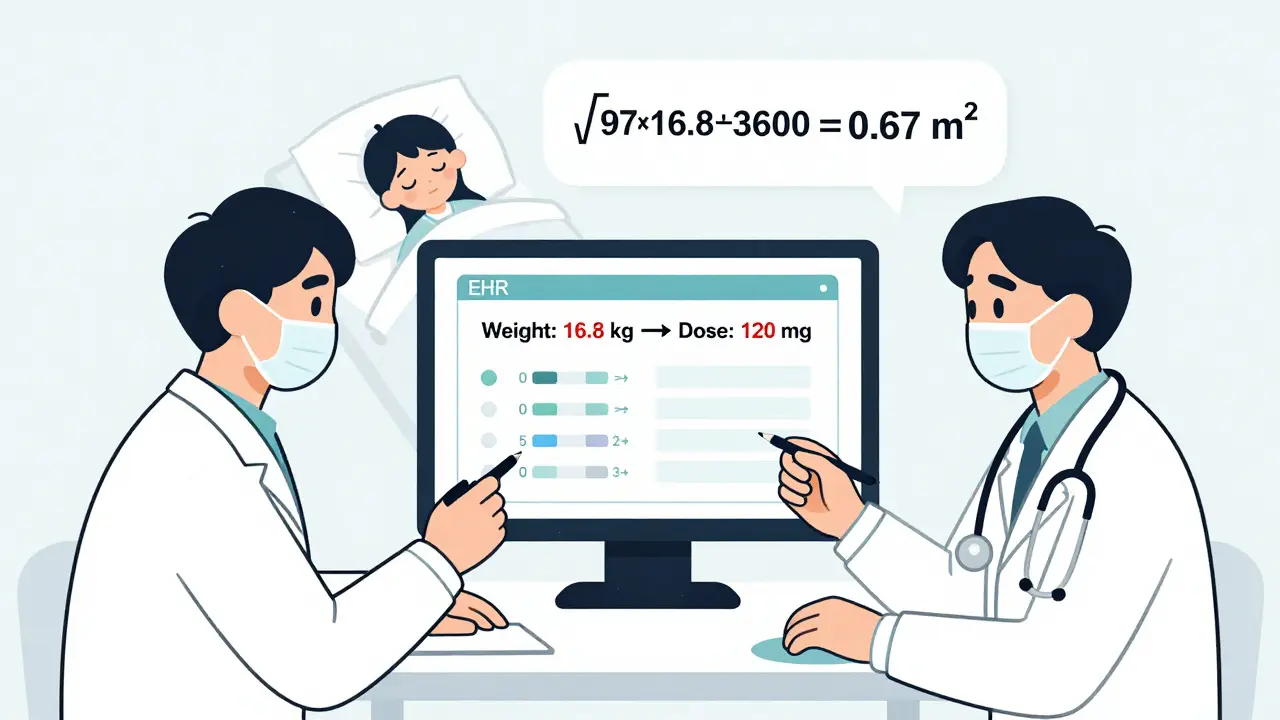
How Hospitals Are Fixing the Problem
Hospitals didn’t just hope people would get better at math. They built systems to prevent errors.- Electronic health records (EHRs) like Epic and Cerner now auto-convert pounds to kilograms and calculate doses in real time. A 2023 JAMA Pediatrics study found this cut dosing errors by 57%.
- Dual verification is mandatory for high-alert drugs like insulin, morphine, and chemotherapy. Two licensed providers must sign off.
- Standardized order sets prevent vague orders like “mg/kg/d.” Now, orders must specify “mg/kg/day” or “mg/kg/dose.”
- AI tools are being tested. Children’s Hospital of Philadelphia uses machine learning to flag doses that deviate from historical patterns. In trials, it caught 92% of potential errors before they reached the patient.
What Parents Should Do
You’re not expected to be a pharmacist. But you are responsible for your child’s safety.- Always ask: “Is this dose based on my child’s weight?”
- Write down the weight in kilograms. Keep it on your phone or in your wallet.
- Take a photo of the medicine bottle’s concentration label.
- Use only the dosing tool that came with the medicine.
- If the dose seems too high or too low - ask again. Don’t assume it’s right.
Final Rule: Never Guess. Always Verify.
Weight-based dosing works - but only if done right. The math isn’t hard. The consequences of getting it wrong are. Every child is different. Their metabolism, their liver, their kidneys - all develop at different rates. A 6-month-old and a 6-year-old may weigh the same, but their bodies handle drugs differently. That’s why dosing guidelines say: “These are general recommendations only.” The final decision always belongs to the provider - and the parent. Use the numbers as a tool, not a substitute for judgment.How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, if your child weighs 33 pounds, 33 ÷ 2.2 = 15 kg. Never round unless instructed by a provider - and even then, only after double-checking. Use a calculator or phone app. Never do it in your head.
What if the prescription says ‘mg/kg/d’?
That notation is confusing and outdated. It means milligrams per kilogram per day - the total daily dose. You must ask the prescriber how many times a day to give it. For example, if the dose is 10 mg/kg/d and it’s given twice daily, each dose is 5 mg/kg. Never assume.
Can I use the same dose for different brands of the same medicine?
No. Different brands or formulations can have different concentrations. Children’s Tylenol is 160 mg per 5 mL. Infant Tylenol drops are 80 mg per 0.8 mL. Using the wrong one can lead to a 10-fold overdose. Always check the concentration on the bottle before giving any dose.
Is it safe to give my child adult medicine if I cut the dose in half?
Never. Adult medications are not formulated for children. They may contain inactive ingredients that are unsafe for kids, or the concentration may be too high to safely divide. Always use a pediatric-specific product approved for your child’s age and weight.
What should I do if I think I gave the wrong dose?
Call Poison Control immediately at 1-800-222-1222. Do not wait for symptoms. Even small overdoses can be dangerous in children. Keep the medicine bottle handy - you’ll need the concentration and ingredients for the operator.
13 Comments
Kiruthiga Udayakumar
January 8 2026
Wow. Just... wow. I’m a nurse in Mumbai and I’ve seen kids given adult doses because the mom thought ‘half a pill’ was fine. This post should be mandatory reading for every parent, grandparent, and babysitter with a medicine cabinet. No more guessing. No more ‘I think it’s okay.’ Weight. Is. Everything. 🙏
tali murah
January 8 2026
Let me guess - the 44-pound kid got 44mg of something because someone forgot to divide by 2.2. Again. This isn’t negligence. It’s a systemic failure wrapped in a laziness bow. Hospitals still use paper charts in 2024? Are we in a time loop? 😒
Patty Walters
January 9 2026
Thank you for this. I’m a mom of two and I keep a note in my phone: ‘1 kg = 2.2 lb’ and the concentration of every med we’ve ever used. I take a pic of the bottle every time. I don’t care if I look obsessive. My kid’s liver doesn’t get a second chance. 💙
Catherine Scutt
January 10 2026
People still use kitchen spoons?? I swear half the pediatric ER is just parents with measuring cups from their baking drawer. 🤦♀️
Johanna Baxter
January 10 2026
My cousin’s kid almost died because they gave infant Tylenol thinking it was the same as kids’ liquid. Now the kid has liver damage. And the pharmacy? They didn’t even warn them. This isn’t an accident. It’s a crime.
Jerian Lewis
January 12 2026
It’s not just about math. It’s about culture. We treat kids like tiny adults because we don’t want to admit how little we understand their bodies. We outsource responsibility to labels. And then we blame the parents when things go wrong.
Diana Stoyanova
January 13 2026
Okay but let’s talk about the AI tools - I work in a hospital that uses the one from CHOP. It flagged a dose for a 3-year-old with asthma that was 3x too high because the nurse typed 20kg instead of 18kg. The AI didn’t just catch it - it sent a pop-up with a link to the weight conversion chart. I cried. Like, actual tears. This is what progress looks like. 🤖❤️
Jenci Spradlin
January 13 2026
ps. i always use the app on my phone to convert lbs to kg. no more head math. also - never trust a bottle that says ‘for ages 2-11’ without checking the mg/kg. those labels are lies wrapped in glitter.
Elisha Muwanga
January 13 2026
Why are we letting non-medical professionals handle this at all? In America, we let anyone parent. No license. No test. No training. But if you want to open a coffee shop? 17 forms. 3 inspections. This is why our kids die. We value capitalism over childhood.
Maggie Noe
January 15 2026
BSA dosing for chemo? I had a friend’s kid on vincristine. The formula looked like rocket science. But the nurse? She printed it out, double-checked with the pharmacist, then had the mom sign off on it. That’s the standard. Not ‘trust the computer.’ Not ‘I’m pretty sure.’ Actual human accountability. 🤝
Gregory Clayton
January 15 2026
Ugh. Another ‘pediatric dosing’ lecture. Can we just make all meds taste like gummy bears and call it a day? Kids don’t care about mg/kg - they care if it’s sweet. Let the adults do the math. I’m tired.
Pooja Kumari
January 16 2026
I’m from India and we don’t have scales in every home. We use old charts - ‘2 years = 10kg’ - and hope. I’ve seen kids get half-doses because the doctor said ‘she looks small.’ But what if she’s just short? What if she’s chubby? Weight isn’t a guess. It’s a number. And we’re failing them because we’re too lazy to weigh them. Every. Single. Time.
Phil Kemling
January 17 2026
What if the real problem isn’t math, but the belief that medicine is a science of certainty? Children aren’t small adults. Their bodies aren’t just scaled-down versions. They’re different organisms - developing, changing, unpredictable. We calculate mg/kg like it’s a fixed equation. But biology isn’t algebra. Maybe we need less math, and more humility.