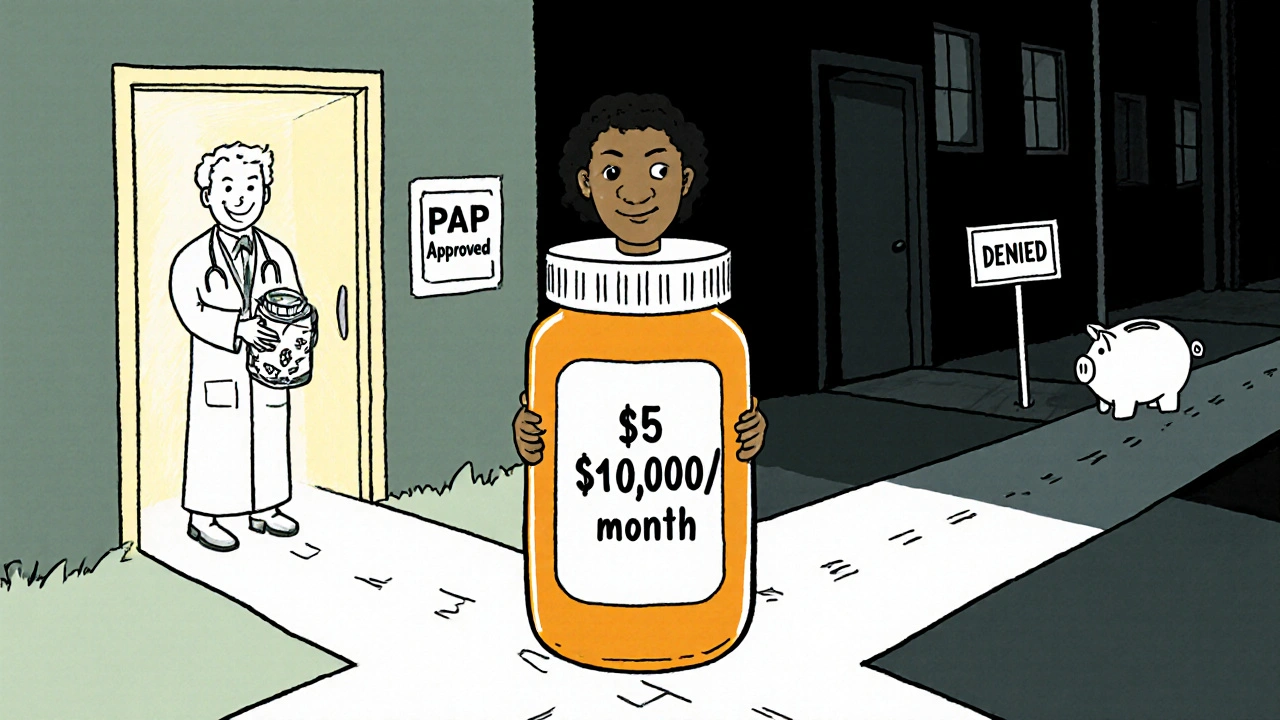
When no generic version of your medication exists, patient assistance programs can cover 90%+ of the cost. Learn how to apply, avoid hidden traps like accumulator policies, and get brand-name drugs for free or low cost.
Brand-Name Medication: What It Is, Why It Matters, and What You Need to Know
When you pick up a prescription, you might see a brand-name medication, a drug sold under a proprietary name by the original manufacturer after patent protection. Also known as proprietary medication, it’s the version you see advertised on TV or recommended by your doctor before the generic version hits the market. These drugs go through years of testing, clinical trials, and regulatory review before they’re approved. That’s why they cost more — not because they work better, but because the company paid to develop them.
But here’s the thing: once the patent expires, other companies can make the exact same drug and sell it as a generic medication, a copy of the brand-name drug with the same active ingredient, strength, and dosage form. Also known as nonproprietary drug, it’s just as safe and effective, but often costs 80% less. That’s why brand-name medication isn’t always the smartest choice — especially if you’re managing a chronic condition like diabetes or high blood pressure. Over time, switching to generics can save you tens of thousands of dollars, as shown in real patient data from long-term studies.
Still, brand-name drugs matter in other ways. Some patients report better results or fewer side effects with the original version — not because the chemistry is different, but because of how the inactive ingredients (fillers, coatings, binders) affect absorption. That’s why your pharmacist might ask if you prefer the brand or generic. And sometimes, the brand is the only option if the generic hasn’t been approved yet, or if your insurance requires prior authorization. That’s where tools like pharmaceutical tracking, systems that use lot numbers and serial codes to trace drugs from factory to pharmacy come in. They help make sure the brand-name pill you’re taking isn’t counterfeit, especially when bought online. With fake drugs flooding the market, knowing your medication’s origin isn’t just smart — it’s life-saving.
And then there’s safety. Brand-name medications often come with clearer labeling, updated instructions, and better patient support programs. But that doesn’t mean generics are unsafe. In fact, the FDA requires them to meet the same strict standards. What’s more important is how you store them. Heat and humidity can ruin both brand-name and generic pills — especially insulin, nitroglycerin, or thyroid meds. That’s why knowing how to read your prescription labels, the printed information on your medicine bottle that includes refill dates, expiration dates, and usage warnings matters more than the brand. A refill-by date isn’t the same as an expiration date. And a QR code on your label? That’s not just tech flair — it’s a direct link to the latest safety info from the manufacturer.
So when you’re deciding between brand-name and generic, ask yourself: Is this drug critical to my health? Do I have a reaction to the filler in the generic? Is my insurance covering it? Are there recalls or counterfeit alerts for this batch? The answers aren’t always obvious. That’s why you’ll find real patient stories here — like how someone with epilepsy avoided seizures after switching from brand to generic, or how a truck driver got caught using a banned brand-name painkiller that wasn’t listed on his DOT form. These aren’t hypotheticals. They’re the kind of details that keep you safe, legal, and in control of your health.