Anticholinergic Burden Calculator
This tool helps you assess your risk from medications with anticholinergic effects. High ACB scores increase risk of confusion, falls, and dementia.
Your Total ACB Score
Risk Assessment
Low Risk (0-1)
Your medications are generally safe for most people. Continue regular monitoring.
Dangerous Combinations Detected
Antihistamine interactions with other sedating medications aren’t just a footnote in a drug leaflet-they can land you in the hospital. Every year, over 300,000 emergency visits in the U.S. are tied to dangerous combinations of these drugs. Many people don’t realize that their nighttime allergy pill, taken for a stuffy nose, can turn into a silent killer when mixed with their sleep aid, anxiety medication, or even a glass of wine. This isn’t theoretical. It’s happening right now, in homes, nursing facilities, and doctor’s offices across the country.
Why Some Antihistamines Are Riskier Than Others
Not all antihistamines are created equal. There are two main types: first-generation and second-generation. The difference isn’t just marketing-it’s life or death. First-generation antihistamines like diphenhydramine (Benadryl), hydroxyzine, and promethazine were designed decades ago to block histamine, the chemical that triggers allergy symptoms. But they also slip easily into the brain, where they mess with other brain chemicals. This causes drowsiness, confusion, and slowed breathing. They’re also strong anticholinergics, meaning they block acetylcholine, a key neurotransmitter for memory, focus, and muscle control. On the Anticholinergic Cognitive Burden (ACB) scale, diphenhydramine scores a 3-the highest level of risk. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were made to avoid this. They’re engineered to stay out of the brain. Their ACB scores are 0 or 1. That’s why they’re called “non-drowsy.” In user surveys, 97% of people taking loratadine reported no drowsiness, compared to 68% of those on diphenhydramine.The Dangerous Cocktail: Antihistamines + Other CNS Depressants
The real danger kicks in when you mix first-generation antihistamines with other drugs that slow down your central nervous system (CNS). These include:- Benzodiazepines (like lorazepam, alprazolam/Xanax)
- Opioids (like oxycodone, hydrocodone, codeine)
- Sleep aids (like zolpidem/Ambien)
- Alcohol
- Some antidepressants (like trazodone, amitriptyline)
Why Older Adults Are at Highest Risk
People over 65 are especially vulnerable. Their bodies clear drugs slower. Liver and kidney function decline. Muscle mass drops. Fat increases. All of this means drugs like diphenhydramine stick around longer and build up in the system. The American Geriatrics Society lists first-generation antihistamines on its Beers Criteria-the official list of medications that should be avoided in older adults. Why? Because they increase the risk of delirium, falls, confusion, and even dementia. A 2021 study in JAMA Internal Medicine found that combining diphenhydramine with other anticholinergic drugs (like oxybutynin for overactive bladder) raised delirium risk by 54%. Even short-term use can be dangerous. Dr. Darryl Toscani, a co-author of the Beers Criteria, says: “Even one night of diphenhydramine with another sedating medication can trigger delirium in someone with early cognitive decline.”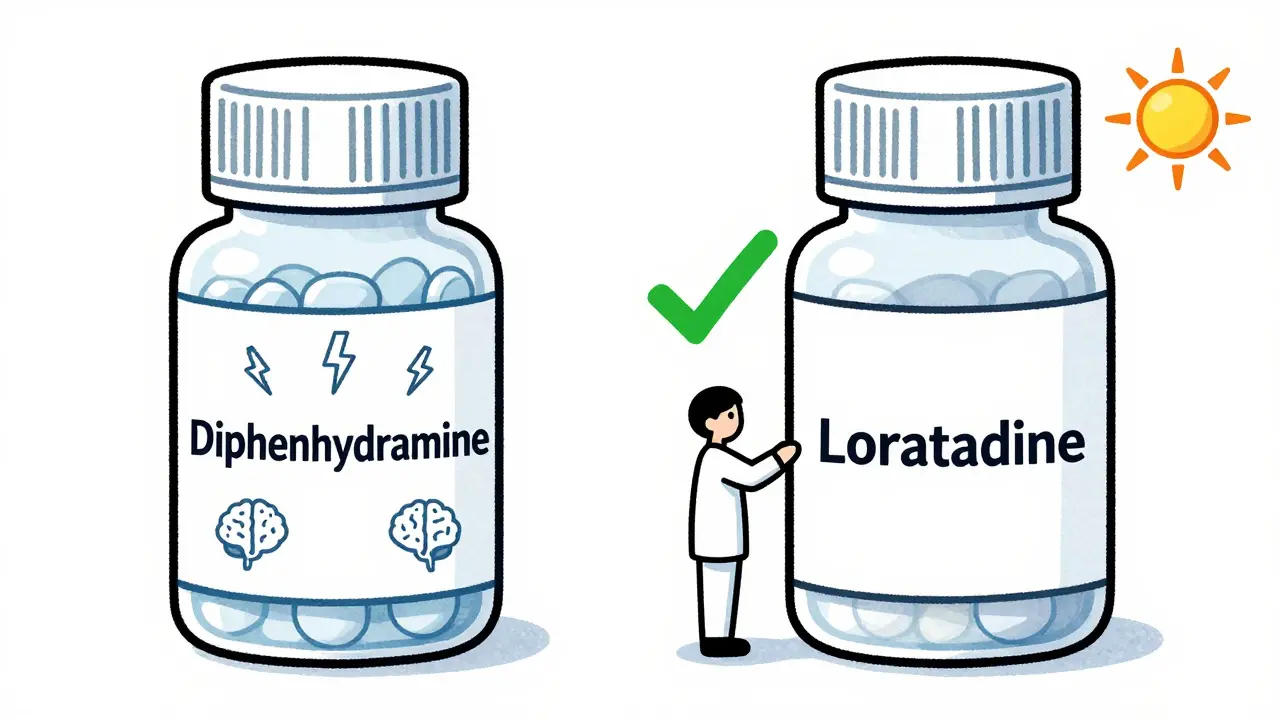
What About H2 Blockers Like Cimetidine?
Cimetidine (Tagamet), an older heartburn medication, isn’t an antihistamine in the traditional sense-it blocks H2 receptors in the stomach. But it’s still dangerous because it interferes with liver enzymes (CYP1A2, CYP2D6, CYP3A4) that break down dozens of other drugs. When cimetidine is taken with diphenhydramine, it can cause diphenhydramine levels to spike by 40-70%. That’s like taking double the dose without knowing it. This isn’t just about antihistamines. Cimetidine can also dangerously increase levels of blood thinners, seizure meds, and antidepressants. Many doctors don’t think to ask about heartburn meds when reviewing a patient’s list of drugs. That’s a gap that can kill.What You Can Do: A Simple Safety Plan
You don’t need to be a pharmacist to protect yourself or a loved one. Here’s what works:- Switch to second-generation antihistamines. If you’re taking Benadryl for allergies, switch to Claritin, Zyrtec, or Allegra. They work just as well for sneezing and runny nose-with none of the brain fog.
- Check your ACB score. The University of Washington has a free online calculator. Add up the ACB scores of all your medications. If the total is 3 or higher, you’re at increased risk for cognitive problems. Ask your doctor if you can drop one.
- Never mix with alcohol or sleep meds. Even one drink with diphenhydramine can cause complete blackouts. One study found people needed hospital care after just one standard drink and 25mg of Benadryl.
- Review all meds with your pharmacist. Pharmacists see your full prescription history. They’re trained to catch dangerous combos. Bring your pill bottles in person or use a free online checker like the Institute for Safe Medication Practices’ tool.
- Ask about deprescribing. If you’re on three or more medications with anticholinergic effects, talk to your doctor about cutting one. Often, you can replace a first-gen antihistamine with a nasal spray or allergy shots.
What’s Changing in the Market
The tide is turning. Sales of first-generation antihistamines have dropped 12.7% every year since 2018. In 2023, second-generation antihistamines made up 83% of the U.S. OTC market. The FDA now requires bold warning labels on diphenhydramine packaging: “May cause severe drowsiness when combined with alcohol, opioids, or sleep medications.” Newer antihistamines like bilastine and levocetirizine are being developed with even more precision-targeting only the H1 receptor and avoiding all other brain activity. A 2023 study showed bilastine had no interaction with lorazepam, even at high doses. Hospitals and health systems are catching up too. Kaiser Permanente added automated alerts in their electronic records that cut antihistamine-related ER visits by 34% between 2020 and 2022.When Is It Still Okay to Use First-Gen Antihistamines?
There are rare exceptions. Dimenhydrinate (Dramamine), which contains diphenhydramine, is still the go-to for motion sickness. Some palliative care teams use low-dose diphenhydramine with benzodiazepines to calm terminal agitation-only under strict supervision. But for allergies, colds, or sleep? There’s no good reason anymore. Second-generation options are just as effective, safer, and widely available.Final Thought: Your Meds Are a Team
No drug works alone. Every pill you take affects how others behave in your body. A “harmless” nighttime allergy pill can turn into a hidden danger when stacked with your anxiety med, your painkiller, or your nightly glass of wine. The solution isn’t to stop taking your meds. It’s to know what you’re taking-and who’s watching your back. Talk to your pharmacist. Use the ACB calculator. Switch to the safer option. It’s not just about avoiding drowsiness. It’s about avoiding the ER, the ICU, or worse.Can I take Benadryl with Xanax?
No. Combining diphenhydramine (Benadryl) with alprazolam (Xanax) or other benzodiazepines can cause extreme drowsiness, confusion, slowed breathing, and even respiratory arrest. Studies show this combination increases sedation by over 35%. There is no safe dose of this mix. Switch to a non-drowsy antihistamine like loratadine or cetirizine instead.
Are all antihistamines equally dangerous?
No. First-generation antihistamines like diphenhydramine, hydroxyzine, and promethazine cross into the brain and cause strong sedation and anticholinergic effects. Second-generation antihistamines like loratadine, cetirizine, and fexofenadine are designed to stay out of the brain and have minimal sedation. They’re much safer to use with other medications.
Is Zyrtec safe with other medications?
Cetirizine (Zyrtec) is a second-generation antihistamine with a low ACB score of 1. It’s generally safer than Benadryl, but it can still cause drowsiness in some people, especially when combined with opioids, alcohol, or sleep aids. It’s not risk-free, but it’s far less likely to cause dangerous interactions than first-generation options.
Can antihistamines cause dementia?
Long-term use of high-anticholinergic drugs-including first-generation antihistamines like diphenhydramine-has been linked to a higher risk of dementia. A 2015 study found that people with the highest cumulative anticholinergic exposure had a 54% increased risk of developing dementia over 10 years. This risk builds up over time, even with occasional use.
What should I do if I’m already taking Benadryl with other sedating meds?
Don’t stop suddenly if you’re using it for sleep or anxiety-talk to your doctor first. But start by switching to a non-drowsy antihistamine like Claritin or Allegra for allergies. Review every medication you take with your pharmacist. Use the Anticholinergic Burden Calculator to see your total risk. If your combined score is 3 or higher, ask about deprescribing.
Are there any natural alternatives to antihistamines?
There’s no proven natural substitute that works like prescription or OTC antihistamines. Some people report relief from local honey or quercetin supplements, but no large studies confirm they block histamine effectively. For reliable allergy control, second-generation antihistamines remain the safest and most effective option. Avoid unregulated herbal products-they may interact unpredictably with your other meds.

11 Comments
Nicole Beasley
December 28 2025
OMG I had no idea Benadryl was this dangerous 😱 I’ve been taking it with my wine every night for years… time to switch to Zyrtec ASAP. Thanks for the wake-up call!
sonam gupta
December 29 2025
Western medicine is full of lies your body is not weak stop taking pills
Julius Hader
December 29 2025
Look I get it people are scared of meds but this is just fearmongering. I’ve taken Benadryl with Xanax for years and I’m fine. If you’re gonna panic over a little drowsiness maybe you should just stop living.
Vu L
December 31 2025
Second-gen antihistamines are just Big Pharma’s way of making you pay more for the same thing. Benadryl works better and costs 50 cents. Also Zyrtec gives me brain fog so don’t act like it’s magic.
James Hilton
December 31 2025
So let me get this straight… we’re telling older folks to ditch their $0.25 Benadryl so they can spend $12 on a bottle of Claritin? That’s not safety that’s capitalism with a side of condescension. 🤡
Mimi Bos
December 31 2025
i just relized i took benadryl with my ambien last week… hope im ok lol
oluwarotimi w alaka
December 31 2025
They want you to stop using benadryl because the chinese own the patents on zyrtec now and they want you dependent on their meds. also the fda is controlled by the cia and they dont want you sleeping too well
Debra Cagwin
January 1 2026
If you’re reading this and you’re over 65 or caring for someone who is - please, take a moment to review your meds. You don’t need to be a doctor to make a life-saving change. Talk to your pharmacist. Use the ACB calculator. It’s one of the easiest ways to protect your brain. You’ve earned that clarity.
Celia McTighe
January 3 2026
I used to take Benadryl for sleep until I woke up confused and fell down the stairs. Now I use melatonin and a weighted blanket. I still get sleepy sometimes but at least I don’t feel like I’m in a fog. Thanks for sharing this - it saved me from a worse accident 😊
Ryan Touhill
January 4 2026
While the data presented is statistically significant, one must question the epistemological framework underpinning the ACB scale. Is cognitive burden truly quantifiable via a three-point ordinal scale? And further - is the reduction in ER visits attributable to labeling, or merely to the natural market shift toward second-generation agents? The causal chain remains, at best, correlational.
Teresa Marzo Lostalé
January 4 2026
There’s something deeply human about how we treat our bodies like machines we can just plug and play with. We stack meds like Legos, never asking why they’re there - or who decided we needed them. Maybe the real danger isn’t the drugs… it’s that we stopped listening to ourselves.
I used to take Benadryl to sleep because I thought I was broken. Turns out I just needed better sleep hygiene. No pills. No panic. Just quiet. And yes - I still drink wine. But now I don’t mix it with anything that makes my brain feel like it’s underwater.
It’s not about being perfect. It’s about being aware. And maybe that’s the most dangerous thing of all - realizing you’ve been asleep while the world kept spinning.