Every time you take an antibiotic when you don’t need it, you’re not just helping yourself-you’re helping bacteria become stronger. That’s the quiet, dangerous truth behind the rise of antibiotic overuse. It’s not just about one person getting sick. It’s about entire communities losing the ability to treat simple infections. And one of the biggest, most overlooked consequences is the rise of Clostridioides difficile, or C. difficile, a gut infection that can turn a routine hospital stay into a life-threatening event.
What Happens When Antibiotics Don’t Work Anymore?
Antibiotics are powerful tools-but they’re not magic pills. They only work on bacteria, not viruses. Yet, in 2023, nearly one in six bacterial infections worldwide were resistant to the first-line antibiotics doctors normally reach for. That’s according to the World Health Organization’s latest global surveillance report. In some regions, like Southeast Asia and the Eastern Mediterranean, that number jumps to one in three. This isn’t science fiction. It’s happening now. Bacteria like Escherichia coli and Staphylococcus aureus are evolving faster than new drugs can be made. Forty-two percent of E. coli cases in 76 countries are now resistant to third-generation cephalosporins-drugs meant for serious urinary and bloodstream infections. In the U.S., methicillin-resistant Staphylococcus aureus (MRSA) still affects tens of thousands every year. And resistance to carbapenems, the last-resort antibiotics, is doubling every decade. The reason? Overuse. Not just in hospitals, but in homes, farms, and clinics. A sore throat caused by a virus? Antibiotics won’t help. But they’re still prescribed-sometimes because patients ask, sometimes because doctors feel pressured. In low-resource settings, where labs can’t confirm if an infection is bacterial, antibiotics are given as a guess. That guess is costing lives.How C. difficile Turns Antibiotics Into a Trap
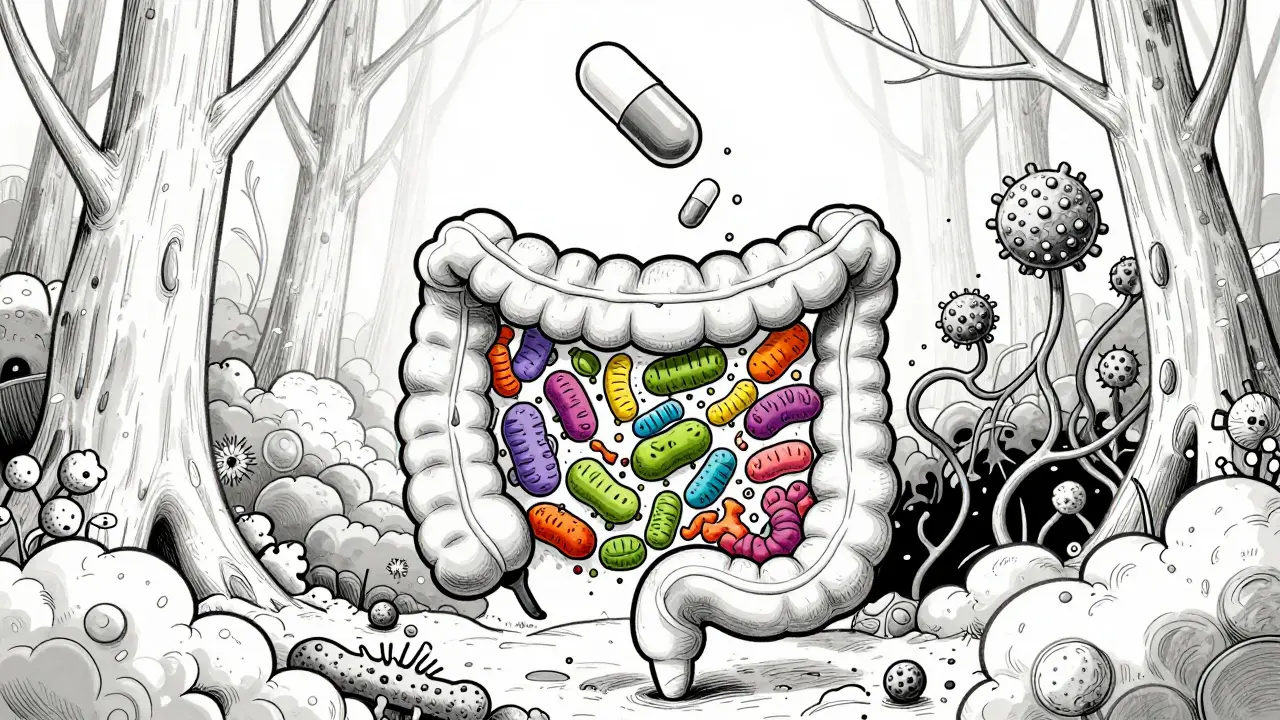
C. difficile isn’t a new germ. But it’s becoming a bigger problem because of how we use antibiotics. Your gut has trillions of good bacteria that keep harmful ones in check. When you take an antibiotic-even for a simple ear infection-you’re not just killing the bad bacteria. You’re wiping out the good ones too. That creates a vacuum. And C. difficile is waiting. Once it takes hold, it doesn’t just cause diarrhea. It can lead to severe inflammation of the colon, sepsis, organ failure, and death. In the U.S. alone, C. difficile caused nearly half a million infections in 2017. Around 29,000 people died that year. While exact numbers for 2025 aren’t finalized, trends show it’s still climbing. The CDC reports that hospital-acquired resistant infections jumped 20% during the pandemic, partly because antibiotic use spiked as doctors tried to prevent secondary infections in vulnerable patients. What’s worse? C. difficile doesn’t always go away after treatment. Up to 20% of people get it again. And each recurrence makes the next one harder to treat. Some patients need fecal transplants just to restore their gut flora. That’s not science fiction-it’s a real treatment for people who’ve lost their natural defenses because of antibiotics.
Why the System Keeps Failing
You’d think we’d learn from this. But the system is built to fail. Hospitals still prescribe broad-spectrum antibiotics before they even know what’s causing the infection. Primary care clinics still hand out prescriptions for colds and flu. Parents give leftover antibiotics to kids with earaches. And in agriculture, antibiotics are still used to make livestock grow faster-not just to treat sick animals. Even when doctors want to be careful, they’re stuck. Many clinics don’t have rapid diagnostic tests. Waiting 48 hours for a culture result means patients leave with a prescription, just in case. That’s not negligence-it’s a system failure. The economic side is just as broken. Drug companies aren’t investing in new antibiotics because they don’t make money. A new cancer drug can earn billions. A new antibiotic? It’s held in reserve, used only as a last resort. So why spend $1 billion to develop it? The result? The pipeline is dry. Of the 25 antibiotics the WHO calls critically important, many are already in short supply in 64% of countries.What You Can Do-And What You Shouldn’t
You don’t need to be a doctor to help stop this crisis. Here’s what actually works:- Don’t ask for antibiotics if your doctor says you have a virus. Colds, flu, most sore throats, and bronchitis are viral. Antibiotics won’t touch them.
- Never use leftover antibiotics. The dose is wrong, the type is wrong, and it’s likely expired. This is one of the top ways resistance spreads in households.
- Finish your full course-but only if it’s truly needed. If your doctor says you’re done early, trust them. You don’t need to take antibiotics longer than necessary.
- Ask about alternatives. For sinus infections or ear infections, sometimes watchful waiting works better than immediate antibiotics.
- Practice good hygiene. Wash your hands. Get vaccinated. Prevent infections before they start.

What’s Being Done-and Why It’s Not Enough
There are programs trying to fix this. Antibiotic stewardship teams in hospitals are reducing unnecessary prescriptions. The WHO’s Global Action Plan has been signed by 194 countries. CARB-X, a public-private partnership, has invested over $480 million into new antibiotic research since 2016. But progress is slow. Only 40% of countries have national action plans fully implemented. Surveillance is still patchy. In many places, doctors don’t even know what bacteria are circulating. And without better diagnostics, we’re still flying blind. The WHO’s 2025 report shows resistance is rising in over 40% of the pathogen-antibiotic combinations they track. That’s not a glitch. That’s a trend. And if it continues, we’ll reach a point where even minor surgeries become dangerous. A simple hip replacement could lead to an untreatable infection. Chemotherapy could become too risky because your immune system can’t fight off a simple fever.The Future Is Either Better or Bleaker
We’re at a fork in the road. One path leads to a world where antibiotics are useless for most infections. Where common illnesses kill. Where hospitals become places of last resort-not healing. The other path? We change how we use these drugs. We invest in faster diagnostics. We stop overprescribing. We support new treatments. We make sure antibiotics are used only when they’re truly needed. The science is clear. The data is alarming. And the cost of inaction? Experts predict 10 million deaths a year by 2050-more than cancer. That’s not a guess. That’s a projection based on current trends. We don’t need a miracle. We need discipline. We need to stop treating antibiotics like candy. And we need to remember: every pill you take, or refuse to take, has a ripple effect.Can antibiotics cause C. difficile even if I take them correctly?
Yes. Even when taken exactly as prescribed, antibiotics can disrupt your gut bacteria enough to allow C. difficile to grow. That’s why they’re the top risk factor for this infection. The more antibiotics you take-and the broader their spectrum-the higher the risk. That’s why doctors are now choosing narrower-spectrum antibiotics when possible, to reduce collateral damage to your gut.
Is antibiotic resistance only a problem in hospitals?
No. While hospitals are hotspots because of high antibiotic use and vulnerable patients, resistance is growing everywhere. Community-acquired resistant infections are rising fast. A urinary tract infection you get at home might be caused by bacteria already resistant to common drugs. That’s why some simple infections now require IV antibiotics even in outpatient clinics.
Are natural remedies a good alternative to antibiotics?
For viral infections like colds or flu, yes-rest, fluids, and time are the best treatments. But for confirmed bacterial infections like strep throat, pneumonia, or sepsis, natural remedies won’t work. Delaying real treatment can turn a treatable infection into a life-threatening one. Don’t trade science for superstition when lives are on the line.
Why aren’t new antibiotics being developed faster?
Because the business model doesn’t work. Antibiotics are used for short courses, and new ones are kept in reserve to slow resistance. That means companies can’t make enough profit to justify the $1 billion cost of development. Most big pharma has walked away from antibiotic research. Only small biotechs and public funding are keeping the pipeline alive-and even that’s not enough.
Can I avoid C. difficile if I never take antibiotics?
Not entirely. C. difficile spores are everywhere-in hospitals, nursing homes, and even on surfaces in public places. But your risk drops dramatically if you avoid unnecessary antibiotics. Your gut bacteria stay strong, and they naturally fight off the bad ones. Antibiotic use is the biggest controllable risk factor. Avoiding them when you don’t need them is your best shield.
15 Comments
steve rumsford
January 7 2026
antibiotics are literally candy now and we wonder why everyone gets sick all the time
LALITA KUDIYA
January 8 2026
i grew up in rural india where antibiotics were rare and we used turmeric and neem for everything
we didn’t get sick often and when we did we rested
now kids get amoxicillin for a sniffle and wonder why they can’t fight anything
Poppy Newman
January 9 2026
the c. diff thing hits different after you’ve had it
imagine your gut being a garden and someone comes in with a flamethrower labeled "medicine"
now you need a stranger’s poop to replant it 😔
Anthony Capunong
January 10 2026
this is why america needs to stop letting foreigners prescribe pills
in my family we never took antibiotics unless we were literally dying
your weak immune system is your fault for eating kale and yoga
Vince Nairn
January 11 2026
so you’re telling me the same system that gives you a 30-minute doctor visit and a script for azithromycin
also expects you to magically know the difference between viral and bacterial
and then blames you when you get c. diff
ohhhhh sure
the real villain here is the guy who wrote the insurance forms
not the guy who wrote the antibiotic guidelines
Ayodeji Williams
January 12 2026
in nigeria we just use garlic and prayer
if you still sick after that you dead anyway
why waste money on pills that dont work?
lol
Kyle King
January 12 2026
antibiotics are a government mind control tool to make you dependent on pharma
the real c. diff is the FDA and WHO pushing this narrative to sell more tests
they don’t want you to heal naturally
they want you hooked on pills forever
ask yourself: who profits from your gut being destroyed?
it’s not the farmer
it’s the lab coat guy with the billion dollar salary
Kamlesh Chauhan
January 13 2026
why do people care so much about antibiotics
we all gonna die eventually
just take the pill and shut up
my cousin took 12 courses last year and still got cancer
so what
Emma Addison Thomas
January 14 2026
my grandmother in rural wales never saw an antibiotic until she was 60
she lived to 94 with a strong gut and no hospital stays
we’ve confused convenience with health
and now we’re paying the price
it’s not just about medicine-it’s about how we’ve lost our relationship with our own bodies
Mina Murray
January 16 2026
you think this is bad wait till the 5g towers start emitting antibiotic-resistant spores
they’ve been testing this since 2018 in 5g cities
that’s why your diarrhea won’t go away
it’s not the meds it’s the microwaves
and the CDC knows
they just won’t tell you
they’re paid by big pharma
and the vaccines are the real cause of c. diff
you think that’s a coincidence
Rachel Steward
January 16 2026
the entire medical-industrial complex is a Ponzi scheme built on the illusion of control
we don’t cure illness-we monetize symptoms
antibiotics are the perfect product: expensive, addictive, and guaranteed to create more demand
the real epidemic isn’t resistance-it’s the belief that we can engineer our way out of biology
you can’t outsmart evolution
you can only delay the inevitable with a prescription pad
and then wonder why your gut is a wasteland
Christine Joy Chicano
January 17 2026
the poetic tragedy here is that we’ve weaponized healing
antibiotics were once miracles-now they’re the blunt instrument of a broken system
we treat the body like a battlefield to be bombed into submission
but the gut isn’t a warzone-it’s a symphony
and every antibiotic is a conductor smashing the cello
the silence that follows isn’t peace
it’s the sound of a thousand microbial voices screaming into the void
and then-c. diff walks in like it owns the place
Adam Gainski
January 17 2026
i work in a rural clinic and we’ve cut antibiotic prescriptions by 60% in two years
we started using rapid strep tests and waiting 48 hours for ear infections
parents were skeptical at first
but now they bring their kids back saying "they’re better without the pills"
it’s not magic-it’s patience and education
and yeah, we still get pushback
but when you see a kid who didn’t get c. diff because you held off on the amoxicillin
you know it matters
Anastasia Novak
January 19 2026
oh look another do-gooder with a blog post telling me to "be responsible"
you think i care about your c. diff statistics
my kid had a fever and i wanted the damn pill
not a lecture on microbial ecology
you’re not a doctor
you’re just someone who read a WHO report and thinks that makes you wise
go touch grass and stop judging people who just want their kid to feel better
Jonathan Larson
January 21 2026
as someone who has spent two decades studying antimicrobial resistance in both clinical and agricultural settings, I must emphasize that the framing of this issue as a matter of individual choice is dangerously incomplete.
While patient demand and physician prescribing habits are significant, they are symptoms of a deeper structural failure: the absence of affordable, rapid diagnostics in 87% of primary care clinics globally.
When a child presents with fever and cough in a clinic with no access to PCR or antigen testing, the default is antibiotics-not because the provider is negligent, but because the system has not equipped them with alternatives.
Moreover, the economic disincentives for antibiotic development are not merely market failures-they are policy failures. Governments have allowed patent systems to prioritize chronic disease drugs over acute antimicrobials, despite the latter being classified as essential medicines by the WHO.
It is not enough to ask patients to "not ask for antibiotics." We must redesign the entire ecosystem: subsidize diagnostics, incentivize stewardship programs with funding-not just guidelines-and create public-private partnerships that reward antibiotic innovation based on public health impact, not profit margins.
Every pill refused is a small victory. But the real victory lies in making refusal the default-not the exception.
This is not about blame. It is about redesign.