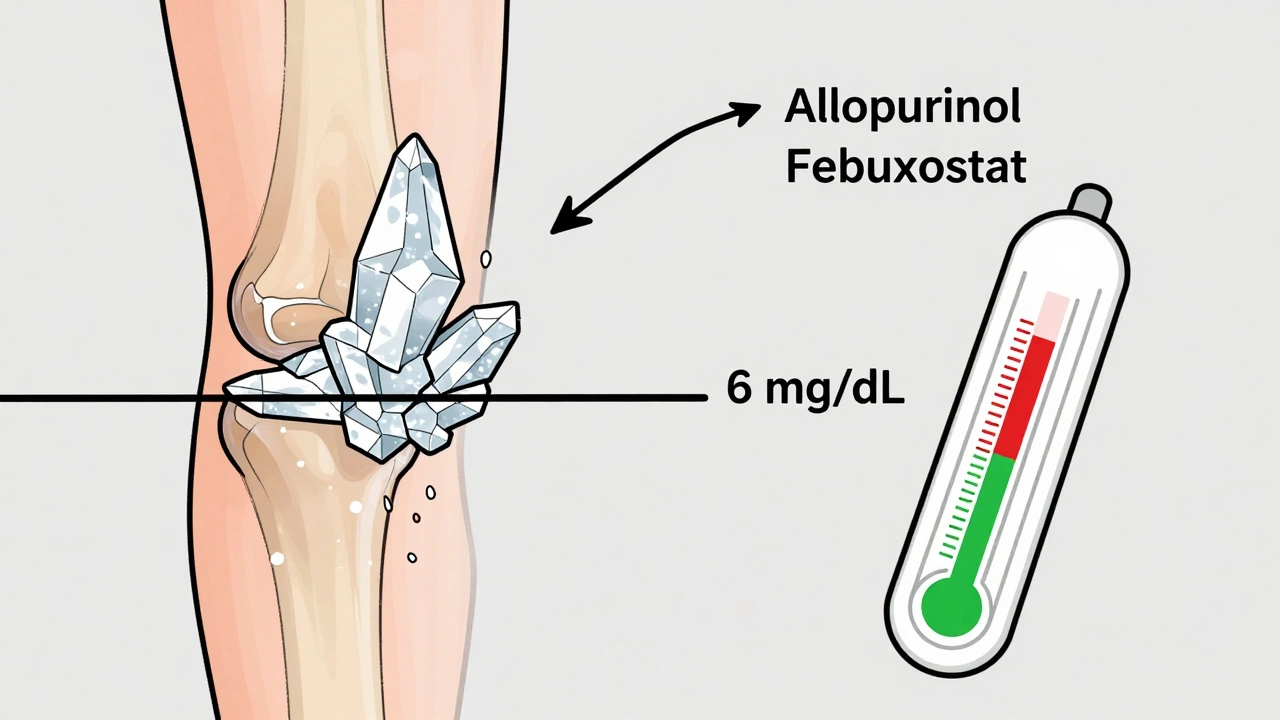
When you have gout, it’s not enough to just treat the pain. If your blood uric acid stays too high, crystals keep forming in your joints - even when you’re not having a flare. That’s why doctors now focus on a single number: your serum urate. Getting this level below 6 mg/dL (360 micromol/L) is the first step to stopping gout for good. And for people with tophi, joint damage, or frequent flares, the goal drops even lower - to under 5 mg/dL (300 micromol/L). This isn’t guesswork. It’s science backed by decades of research and updated guidelines from the American College of Rheumatology, NICE, and EULAR.
Why 6 mg/dL? The Science Behind the Number
The number 6 mg/dL isn’t arbitrary. It’s the point where uric acid stops crystallizing in your joints. Above this level, monosodium urate crystals form and stick around. Below it, they begin to dissolve. Think of it like salt in water: if you add too much, it settles at the bottom. But if you dilute it enough, it disappears back into solution. That’s what lowering serum urate does for gout.
Studies show that keeping urate below 6 mg/dL cuts flare frequency by 74%. In one trial, patients who hit this target had 89% fewer tophi after two years. And if you go even lower - under 5 mg/dL - you speed up crystal dissolution. For someone with visible lumps under the skin (tophi), this isn’t just comfort - it’s preventing permanent joint damage.
But there’s a limit. Going below 3 mg/dL doesn’t help more - and might cause other issues. No guideline recommends going that low. The goal isn’t to wipe out all uric acid. It’s to get it just low enough to stop the crystals.
Allopurinol: The First-Line Choice for Most
Allopurinol is the most common drug used to lower urate. It works by blocking the enzyme that makes uric acid. It’s cheap - generic versions cost $4 to $12 a month in the U.S. - and has been around since the 1960s. But here’s the catch: most people don’t take enough of it.
Doctors often start patients at 100 mg a day. That’s not enough for most. Real-world data from New Zealand shows 30-50% of patients need doses above 300 mg, and many need 600-800 mg to reach their target. The trick? Start low, go slow. Increase by 50-100 mg every 2-4 weeks, checking your serum urate each time. Don’t just give a fixed dose and hope for the best.
There’s one big safety warning: allopurinol can cause a rare but serious skin reaction called allopurinol hypersensitivity syndrome. The risk is 25 times higher if you carry the HLA-B*5801 gene - common in people of Asian, African, or Native American descent. Testing for this gene before starting isn’t routine everywhere, but it should be considered, especially if you have kidney issues or belong to a higher-risk group.
Febuxostat: When Allopurinol Isn’t Enough
Febuxostat is the other main drug. It works the same way - blocks uric acid production - but it’s stronger and doesn’t rely on kidney function to clear it from your body. That makes it a better choice if you have moderate to severe kidney disease.
A 2023 meta-analysis found febuxostat helped 15% more patients reach their urate target than allopurinol in those with CKD. It’s also faster: you can start at 40 mg and bump to 80 mg in a month if needed. But it’s pricier - $30 to $50 a month - and has a black box warning for possible heart risks. That’s why guidelines like NICE say it’s fine as a first choice, but only if you can’t use allopurinol or it doesn’t work.
For people with normal kidneys, most guidelines still prefer allopurinol. But if you’ve tried it at high doses and still have flares or tophi, febuxostat is a solid next step.
The Real Problem: Most People Never Reach Their Target
Here’s the uncomfortable truth: only about 42% of gout patients hit their urate target within a year. Why?
- Dosing mistakes: Doctors often start too low and never increase. Patients think “I’m on medicine, so I’m fine,” and skip follow-ups.
- Flare paradox: When you start lowering urate, crystals start to dissolve - and that can trigger flares. Patients panic and stop the drug. But this is normal. Taking low-dose colchicine or NSAIDs for the first 6 months helps.
- Testing gaps: Monthly urate checks during titration boost success by 31%. Yet in the U.S., only 54% of patients get them.
- Education: 62% of patients say their provider never explained how to titrate the dose. They’re left guessing.
One solution? Protocol-driven care. Kaiser Permanente’s program - where pharmacists monitor urate levels and adjust doses automatically - got 67% of patients to target. That’s nearly double the usual rate.
Who Needs the Lower Target? (Under 5 mg/dL)
Not everyone needs to go below 6 mg/dL. But if you have any of these, aim for 5 mg/dL or lower:
- Visible tophi (lumps under skin)
- Joint damage seen on X-rays
- Two or more flares a year despite being on treatment
- Chronic kidney disease with gout
For these patients, the goal isn’t just fewer flares - it’s dissolving the crystals that are already there. Dual-energy CT scans can show crystal reduction over time. Some experts now call this “treat-to-dissolve.” Once crystals are gone, you might be able to lower your dose - but don’t stop the medicine.
What About Asymptomatic High Urate?
If your urate is 7 mg/dL but you’ve never had a gout flare? Don’t start medication. The 2020 ACR guideline says no - and most experts agree. Treating high urate without gout doesn’t prevent future flares and exposes you to drug risks for no benefit. Focus on lifestyle: cut back on alcohol, sugary drinks, and red meat. Lose weight if needed. But don’t take pills just because a lab number is high.
What’s Next? Precision Dosing and New Drugs
Research is moving fast. A 2024 study called GOUT-PRO found that testing for two genes - ABCG2 and SLC22A12 - helped predict who responds to allopurinol. Patients who got dosing based on their genes hit their target 83% of the time, compared to 61% with standard dosing.
New drugs are coming too. Verinurad, a uricosuric that helps your kidneys dump more uric acid, is in late-stage trials. It might let people reach targets without massive allopurinol doses. And the ULTRA-GOUT trial, due in late 2025, will compare fixed doses versus treat-to-target. That could change how we think about dosing forever.
Bottom Line: Your Urate Is Your Best Guide
Gout isn’t a one-time flare. It’s a chronic condition that needs ongoing management. Allopurinol and febuxostat aren’t magic pills - they’re tools. Used right, they can make gout disappear. But only if you track your urate, adjust your dose, and stick with it.
Ask your doctor: “What’s my current urate level?” “What’s my target?” “Am I on the right dose?” If they can’t answer, it’s time to find someone who can. The goal isn’t just to feel better next week. It’s to never feel this pain again.
What is the ideal serum urate level for gout patients?
For most people with gout, the target is below 6 mg/dL (360 micromol/L). This stops new crystals from forming and helps dissolve existing ones. If you have tophi, joint damage, or frequent flares, aim even lower - under 5 mg/dL (300 micromol/L). Going below 3 mg/dL isn’t recommended, as it offers no extra benefit and may carry risks.
Is allopurinol better than febuxostat for gout?
Allopurinol is usually the first choice because it’s cheaper and works well for most people. Febuxostat is stronger and safer for those with kidney disease, but it costs more and carries a heart risk warning. If allopurinol doesn’t get your urate low enough - even at high doses - febuxostat is the next step.
Why do I get more flares when I start taking urate-lowering drugs?
When urate levels drop quickly, crystals start to break apart. This can trigger inflammation and flares - even though you’re doing the right thing. This is called the “flare paradox.” It’s temporary. Taking low-dose colchicine or an NSAID for the first 6 months while starting treatment can prevent these flares.
How often should my urate level be checked?
During the first 6-12 months of treatment, check your serum urate every 2-4 weeks as your dose is adjusted. Once you hit your target, check it every 6 months. Monthly testing during titration improves success by 31% compared to less frequent checks.
Can I stop taking allopurinol or febuxostat once my gout feels better?
No. Stopping the medicine lets urate levels rise again, and crystals return. Gout is a chronic condition that needs lifelong management. Even if you haven’t had a flare in years, staying on your dose keeps you protected. Only under close supervision - and with proof crystals are gone - might a doctor consider reducing the dose.
Do I need genetic testing before starting allopurinol?
Not always, but it’s recommended if you’re of African, Asian, or Native American descent, or if you have kidney disease. The HLA-B*5801 gene increases your risk of a dangerous skin reaction to allopurinol. Testing can prevent this rare but serious side effect. Ask your doctor if it’s right for you.
Is it safe to take allopurinol if I have kidney disease?
Yes - but you need a lower starting dose. If you have stage 3 or higher chronic kidney disease, start at 50 mg/day instead of 100 mg. Increase slowly and monitor urate levels closely. Febuxostat may be preferred in severe kidney disease because it’s cleared by the liver, not the kidneys.
What lifestyle changes help lower urate levels?
Cut back on alcohol (especially beer), sugary drinks like soda, red meat, and shellfish. Lose weight if you’re overweight - even 5-10% can lower urate by 1-2 mg/dL. Drink plenty of water, and consider low-fat dairy, cherries, and coffee - these are linked to lower gout risk. But lifestyle alone rarely gets you to target. Medication is still needed for most people.
15 Comments
jagdish kumar
December 4 2025
Urate is just another number the pharmas wants you to obsess over. Real healing? It's in the soil, in the water, in the silence between breaths. You think a pill dissolves crystals? Nah. It dissolves your soul first.
Benjamin Sedler
December 5 2025
Wait - so you're telling me I can't just chug beer and eat steak and then pop a pill to make the pain go away? That's not medicine, that's a scam. I've been doing this for 12 years and I'm still standing. Who even made this 6 mg/dL rule? Some guy in a lab coat who's never felt a gout flare?
zac grant
December 5 2025
For those of you new to urate management - this is the gold standard. The 6 mg/dL threshold is empirically validated across RCTs, meta-analyses, and real-world cohorts. The real bottleneck isn't pharmacology - it's adherence and titration inertia. Most providers default to 100 mg allopurinol and call it a day. That's like prescribing 5 mg of lisinopril for hypertension. You're not treating the disease - you're performing a placebo ritual.
And yes - the flare paradox is real. It's not a failure of the drug. It's a biomarker of efficacy. Dissolving crystals = inflammation. Use colchicine prophylaxis. 0.6 mg BID for 6 months. Done.
Also - HLA-B*5801 screening? If you're South Asian, African, or Indigenous - get tested. It's not optional. It's harm reduction 101.
michael booth
December 6 2025
If you have gout you need to take this seriously. Allopurinol is not optional. Febuxostat is not a last resort. Urate is your number. Check it. Adjust it. Stick with it. You can live without pain. But you have to do the work. No shortcuts. No magic. Just science and consistency. Your future self will thank you.
Carolyn Ford
December 6 2025
Oh, so now we're all supposed to be lab rats? 'Target urate!' 'Dissolve crystals!' Who even decided this? The pharmaceutical industry? The ACR? The same people who told us statins were for everyone? Wake up. You're being sold a chronic disease model to keep you on pills forever. I've been off allopurinol for 4 years. I eat meat. I drink wine. I haven't had a flare. Your 'target' is a trap.
Heidi Thomas
December 7 2025
If you're still on 100mg allopurinol you're not treating gout you're pretending it doesn't exist. The fact that doctors do this is criminal. You don't get to say 'I'm sorry your joints are destroyed' and then give them a baby dose. And yes - febuxostat has cardiac risks. But so does untreated gout. You want to live? Take the right dose. Or don't. But don't act surprised when your foot looks like a rotten plum.
Alex Piddington
December 7 2025
Hey everyone - just wanted to say this is one of the clearest, most practical breakdowns of gout management I've seen. Seriously. The titration advice? Spot on. The flare paradox explanation? Perfect. And the Kaiser Permanente model? That's the future. Pharmacists managing doses? Yes please. We need more of this. Keep sharing this kind of stuff. 👍
Libby Rees
December 8 2025
The science here is sound. The goal of serum urate below 6 mg/dL is not arbitrary. It is the saturation point for monosodium urate crystals. Below this, dissolution begins. Above it, formation continues. This is basic physical chemistry applied to human physiology. The real issue is implementation - not theory. Most patients are not monitored. Most doses are not optimized. That is the failure - not the guideline.
Dematteo Lasonya
December 9 2025
I’ve been on allopurinol for 5 years. I used to have flares every month. Now? Zero. But I didn’t get here by accident. I tracked my urate every 4 weeks. I talked to my pharmacist. I took colchicine when I started. It wasn’t easy - but it was worth it. If you’re reading this and you’re scared of the meds or the numbers - I get it. I was too. But this isn’t about fear. It’s about showing up for yourself. You deserve to walk without pain.
Rudy Van den Boogaert
December 10 2025
My doc started me at 300mg. I asked why not 600. He said 'we'll see how you do.' Three months later I was still at 8.2. He upped it to 400. Still no. Finally at 800 I hit 5.4. Took a year. But now I haven't had a flare in 22 months. If you're not getting to target - you're not trying hard enough. Don't let your doctor be lazy. Push for the dose. Your joints will thank you.
Gillian Watson
December 11 2025
Interesting how this mirrors the UK's NICE guidelines. We've been pushing treat-to-target here for years. The real win? When patients understand that gout isn't a 'flare condition' - it's a metabolic disorder. That shift changes everything. I've seen people go from wheelchair to walking again. Just by lowering urate. No magic. Just math.
Jordan Wall
December 13 2025
So we're all just... urate zombies now? 😅 The 6 mg/dL cult is real. Allopurinol is the new Prozac. Everyone's on it. But nobody talks about how it makes you feel like a ghost. Also, febuxostat? Bro, I got the heart warning like it was a free tattoo. Still took it. Worth it. My tophi? Gone. My bank account? Ruined. My life? Better. 🤷♂️💎
Gareth Storer
December 14 2025
Wow. A whole article about lowering urate and not one mention of the fact that 80% of uric acid is produced endogenously? So your 'diet changes' are basically irrelevant unless you're a monk. Nice distraction tactic, doc. Keep selling pills while people think it's the beer's fault.
Pavan Kankala
December 14 2025
Who funds this 'science'? Big Pharma. They need you addicted to pills. Uric acid isn't evil. It's an antioxidant. They're trying to make you afraid of your own body. The real cause of gout? Toxic food supply. GMO corn syrup. Chemtrails. The government wants you weak. Don't take the pill. Eat raw garlic. Walk barefoot. Wake up.
Martyn Stuart
December 14 2025
This is excellent. I've been a rheumatology nurse for 18 years. I've watched patients lose toes because they stopped their meds after one 'good month'. I've seen tophi disappear in 14 months with consistent dosing and monthly labs. The data is overwhelming. But the emotional resistance? Even stronger. Please - if you're reading this and you're on a low dose and still flaring - talk to your doctor. Don't wait. You're not failing. The system is. But you can still win.