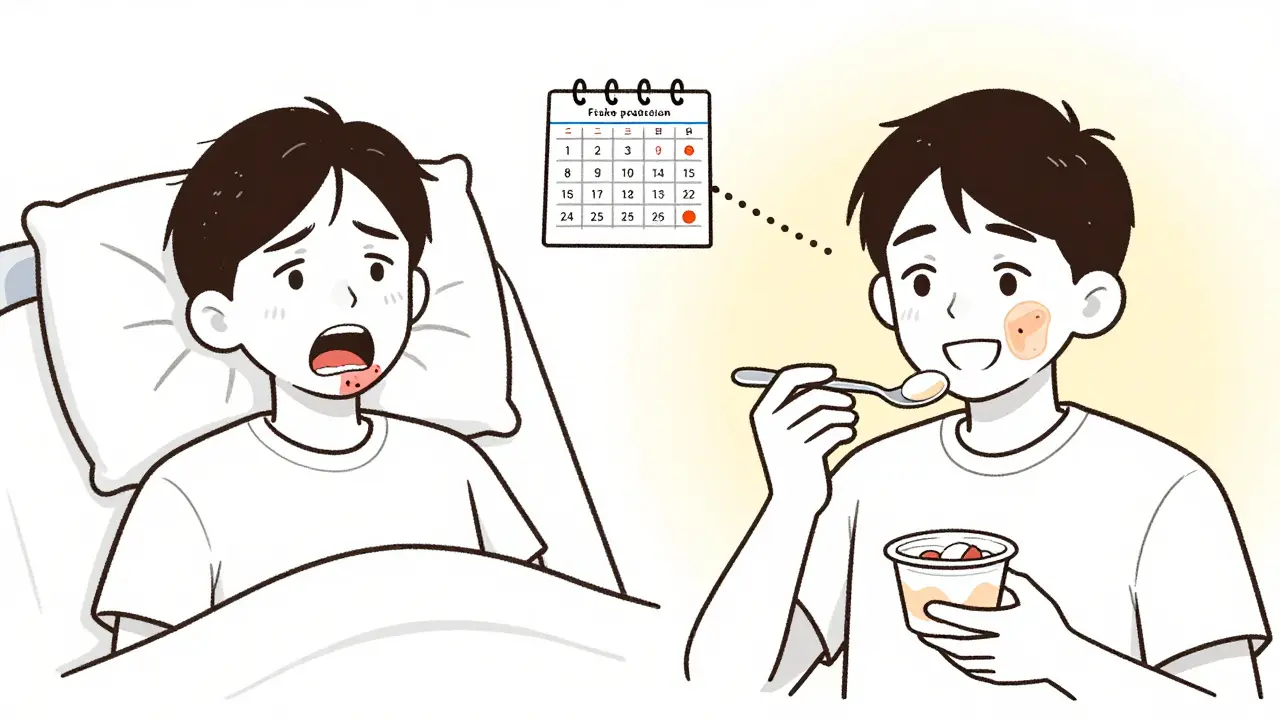
When you’re taking medication for cancer, autoimmune disease, or even high blood pressure, the last thing you expect is to start getting painful sores inside your mouth. But it happens more often than you think. These aren’t just minor irritations-they can make eating, speaking, and even swallowing unbearable. This isn’t rare. Up to 100% of people undergoing certain cancer treatments develop them. The medical term is oral mucositis, and it’s caused by the drugs themselves damaging the thin lining of your mouth. The good news? You don’t have to just suffer through it. Prevention works better than treatment, and there are proven, practical steps you can take right now.
Why Medications Cause Mouth Sores
Not all mouth sores are the same. Canker sores from stress or vitamin deficiency are different from the ones caused by drugs. Medication-induced sores happen because the drugs don’t just target cancer cells or inflammation-they also hit fast-growing cells everywhere, including the ones lining your mouth. Chemotherapy and radiation are the biggest culprits, but even some antibiotics, blood pressure meds, and immunotherapy drugs can trigger them.
The damage starts fast. Within hours of receiving certain chemo drugs like 5-fluorouracil or melphalan, your mouth’s protective layer begins to break down. Inflammation follows, then open sores. These aren’t just painful-they can become infected, delay your treatment, and even land you in the hospital. A 2019 study found severe cases added $1,500 to $17,000 in extra costs per patient because of longer stays and extra care.
What Works: Proven Prevention Methods
Doctors used to wait until sores appeared before doing anything. Now, they know better. Prevention isn’t optional-it’s the standard. Here’s what actually works, based on real studies and clinical guidelines.
- Cryotherapy (ice chips): If you’re getting melphalan or 5-fluorouracil, sucking on ice chips for 30 minutes-starting 5 minutes before your infusion and continuing through it-can cut severe mouth sores by half. It works by freezing the cells in your mouth, slowing down how much drug they absorb. But you have to do it right: no breaks, no sipping, just constant ice. About 42% of people quit because it’s too cold, but those who stick with it report big pain relief.
- Benzydamine mouthwash: This isn’t a regular mouthwash. It’s a topical anti-inflammatory. Use it 3-4 times a day, starting before treatment begins. For people getting radiation to the head or neck, it reduces severe sores by 34%. It costs $15-$25 per course. The downside? It stings at first. But 82% of users keep using it because the pain relief outweighs the burn.
- Palifermin: This is a powerful, injectable drug that tells your mouth’s cells to grow faster. It’s used for stem cell transplant patients and cuts severe sores from 63% down to 20%. But it’s expensive-over $10,000 per treatment-and only given to those with the highest risk. Most insurance won’t cover it unless you’re in a transplant program.
- Glutamine: This amino acid supplement, dissolved in water and swished in your mouth for 2 minutes before swallowing, helped reduce sore duration by 43% in one major trial. But results are mixed. It only seems to help people getting radiation for head and neck cancer-not those on chemo alone. Still, many patients swear by it. One tip: swish it longer than you think you need to.
- Low-level laser therapy (LLLT): Newer but promising. This uses a specific red light (650nm) on the inside of the mouth for a few minutes a day. A 2023 study showed it cut severe sores from 41% to 18%. It’s not widely available yet, but more cancer centers are starting to offer it.
What Doesn’t Work (or Might Hurt)
Some things you’ve heard about? They’re not backed by science-or they’re worse than useless.
- Chlorhexidine mouthwash: This is the most common one doctors hand out. It’s cheap and easy to find. But it only reduces risk by 15%. Worse, long-term use can stain your teeth brown or black. Many patients also say it ruins their taste. The European Medicines Agency now warns against concentrations above 0.2%.
- Systemic antibiotics: Taking pills to prevent infection in your mouth? Don’t. A 2021 study found it raised the risk of dangerous gut infections like C. diff by 27%. Your mouth isn’t infected yet-don’t poison your gut trying to stop it.
- Benzocaine gels: Over-the-counter numbing gels might feel good for a minute, but they’re risky. The FDA warns against using them in kids under 2, and even adults can develop a rare but serious blood condition called methemoglobinemia.
- Alcohol-based mouthwashes: They dry out your mouth, which makes sores worse. Skip them. Even if they say “freshens breath,” they’re not helping your healing.

Daily Care Routine That Makes a Difference
Prevention isn’t just about special treatments. It’s about what you do every single day.
- Brush gently: Use a soft-bristle toothbrush with bristles no thicker than 0.008 inches. Brush twice a day with fluoride toothpaste. No whitening or SLS (sodium lauryl sulfate)-those ingredients irritate sores. Many patients switch to children’s toothpaste because it’s milder.
- Rinse after meals: Mix 1 teaspoon of baking soda in 8 ounces of water. Swish and spit. It neutralizes acid from food and drinks, which can burn open sores.
- Stay hydrated: Dry mouth makes everything worse. If your mouth feels like sandpaper, try Biotene saliva spray or take pilocarpine 5mg tablets three times a day. One study showed it boosts natural saliva by 47%.
- Use Gelclair: This isn’t a cure, but it’s a relief. It’s a gel that sticks to sores like a protective bandage. It lasts up to 4 hours and reduces pain fast. People love it-71% say it works immediately. The downside? It feels slimy. But if you can get past the texture, it’s one of the best tools for daily comfort.
- Dental checkup before treatment: Go to the dentist 2-4 weeks before starting chemo or radiation. Fix cavities, clean your teeth, remove anything that could become a source of infection. Roswell Park Cancer Institute found 78% of severe mouth sores could be avoided with this step alone.
What to Do When Sores Already Happen
If you already have open sores, don’t panic. The goal shifts from prevention to comfort and healing.
- Dexamethasone mouthwash: A prescription rinse (0.5mg/5mL) used four times a day cuts pain scores by 37%. It’s a steroid, so it reduces swelling fast. Use it after meals and don’t eat or drink for 30 minutes after.
- Hydrate and eat soft foods: Avoid spicy, acidic, or crunchy foods. Stick to yogurt, mashed potatoes, smoothies, and soups. Cold foods are easier to tolerate.
- Don’t ignore signs of infection: If your sores turn white, ooze pus, or you develop a fever, call your oncologist. You might need a topical antifungal or a short course of antibiotics-but only if there’s clear infection, not just soreness.
Cost, Access, and Real-Life Challenges
Some of these treatments are expensive. Palifermin costs over $10,000. Benzydamine is $20. Gelclair is $30 a tube. Insurance doesn’t always cover them. A 2022 study found 92% of uninsured patients couldn’t afford palifermin. That’s why prevention tools like ice chips and baking soda rinses are so important-they’re free or nearly free.
Patients on Reddit and CancerCare forums share real tips: “Use a baby toothbrush,” “Swish glutamine for two minutes,” “Avoid mint-flavored anything.” These aren’t just anecdotes-they’re patterns. One patient said, “I stopped crying when I started the ice chips.” Another: “Gelclair let me eat my daughter’s birthday cake again.”
The bigger picture? The global market for mouth sore treatments is growing fast-projected to hit $2 billion by 2030. More hospitals now have formal oral care teams. But access still depends on where you live and what insurance you have. Don’t wait for your doctor to bring it up. Ask: “What’s my risk for mouth sores? What can I start doing today?”
What’s Coming Next
Research is moving fast. Scientists at Memorial Sloan Kettering built a tool that predicts your risk of mouth sores using 12 factors-your age, type of cancer, drug dose, even your saliva flow. It’s 84% accurate. Soon, prevention won’t be one-size-fits-all. It’ll be personalized.
Another drug, GC4419, is in late-stage trials. It’s designed to neutralize free radicals caused by radiation. Early results show it cuts the length of severe sores by 38%. If approved, it could become standard for head and neck cancer patients.
The message is clear: Mouth sores from medication aren’t inevitable. They’re predictable. And predictable means preventable. The tools exist. The evidence is strong. You just need to start before the pain begins.
Can over-the-counter mouthwashes treat medication-induced mouth sores?
Most OTC mouthwashes won’t help and can make things worse. Products with alcohol, mint, or sodium lauryl sulfate irritate the tissue. Chlorhexidine is sometimes prescribed, but it only reduces risk by 15% and can stain teeth. For real relief, use prescription rinses like dexamethasone or topical gels like Gelclair. Ice chips and baking soda rinses are safer, cheaper alternatives.
Is glutamine worth trying for mouth ulcers?
It depends. Glutamine helped reduce sore duration in patients getting radiation for head and neck cancer, but not in those on chemo alone. A 2022 review found mixed results overall. If you’re in the right group, try 15g dissolved in water, swished for 2 minutes, then swallowed, four times a day. Many users report benefit, but it’s not a guaranteed fix. Don’t rely on it alone.
Why do some people get mouth sores and others don’t?
It’s not random. Risk depends on the drug, dose, and your genetics. Radiation to the head/neck has the highest risk. Certain chemo drugs like 5-FU and melphalan are more likely to cause sores. People with poor dental health, dry mouth, or who smoke are at higher risk. New tools can now predict your personal risk with 84% accuracy by combining 12 clinical factors.
Can I use numbing gels like Orajel for relief?
Avoid benzocaine-based gels like Orajel. The FDA warns they can cause methemoglobinemia, a rare but dangerous blood condition that reduces oxygen delivery. Even in adults, the risk isn’t worth it. Use Gelclair or dexamethasone rinse instead-they’re safer and just as effective for pain.
How soon should I start prevention before treatment?
Start before treatment begins. Dental exams should happen 2-4 weeks ahead. Benzydamine mouthwash should be used 3-4 times daily starting at least 2 days before chemo or radiation. Ice chips need to be ready the day your infusion starts. Delaying prevention means missing the window where it’s most effective.
Are there any natural remedies that help?
There’s no strong evidence for honey, aloe vera, or coconut oil as reliable treatments. Some patients find them soothing, but they don’t prevent sores or speed healing like the proven methods do. Stick to science-backed approaches: ice chips, baking soda rinses, prescribed rinses, and soft oral care. Natural doesn’t mean effective-especially when your treatment depends on it.
Next Steps: What to Do Today
If you’re about to start a new medication that can cause mouth sores:
- Ask your oncologist or pharmacist: “What’s my risk for oral mucositis?”
- Schedule a dental checkup-don’t wait until your mouth hurts.
- Buy a soft-bristle toothbrush and fluoride toothpaste without SLS.
- If you’re getting 5-FU or melphalan, buy ice chips and practice the 30-minute routine.
- Ask if benzydamine or Gelclair is right for you. Don’t assume chlorhexidine is the best choice.
You don’t have to wait for pain to start acting. The best time to prevent mouth sores is before they appear. And you have more control over this than you think.
8 Comments
Josh Kenna
January 20 2026
Man, I wish I’d known about the ice chip thing before I went through chemo-my mouth felt like sandpaper for weeks. Just sucking on ice for 30 minutes straight sounds brutal, but if it cuts severe sores in half? Sign me up next time. Also, who knew benzydamine stings at first but then becomes your best friend? I used it after my third round and actually slept through the night for the first time in months.
Christi Steinbeck
January 20 2026
THIS. I’m a nurse and I’ve seen patients suffer needlessly because no one told them to ask about oral care BEFORE treatment. The dental checkup step? Non-negotiable. One lady came in with a tooth abscess that turned into sepsis-could’ve been avoided. Stop waiting for pain. Start prepping like your life depends on it-because it does.
Lydia H.
January 22 2026
I love how this post doesn’t just dump facts-it gives you a roadmap. The part about Gelclair feeling slimy but letting someone eat their daughter’s birthday cake? That’s the kind of detail that sticks with you. It’s not just about medicine, it’s about dignity. When you can taste food again, you feel human. That’s worth every awkward sip of glutamine sludge.
Jake Rudin
January 23 2026
It’s fascinating-our bodies are these intricate, self-repairing systems… and yet, we treat them like disposable machines. Chemotherapy doesn’t discriminate between cancerous cells and mucosal cells-it’s a blunt instrument. But here’s the paradox: the very drugs that save us also break us down. And yet, we’ve engineered solutions-ice, lasers, peptides-that gently nudge biology back into balance. We’re not just surviving… we’re learning to coexist with the violence of cure.
sujit paul
January 24 2026
Interesting how the pharmaceutical industry profits from every stage of this suffering. Ice chips? Free. Gelclair? $30. Palifermin? $10,000. And yet, the same companies who sell the chemo drugs also sell the 'fixes.' Who funds the research? Who controls the guidelines? I’m not saying prevention is bad-but I am saying, question everything. Even the 'evidence.'
Jackson Doughart
January 24 2026
As someone who’s spent years managing chronic illness, I appreciate the nuance here. Too many posts oversimplify: 'Just use baking soda!' But this acknowledges cost, access, and individual variation. The 84% predictive tool? That’s the future. Personalized care isn’t a buzzword-it’s a lifeline. And yes, I switched to children’s toothpaste. No regrets.
Tracy Howard
January 26 2026
Canada has had oral mucositis protocols in place since 2018. We don’t wait for patients to suffer. We don’t make them beg for benzydamine or fight insurance for Gelclair. This is why American healthcare is a joke. You’re lucky if your oncologist even mentions your mouth. Meanwhile, in Toronto, you get a dedicated oral care nurse on day one. Shameful.
Erwin Kodiat
January 26 2026
Just wanted to say: I tried the ice chips. It was the coldest 30 minutes of my life. My teeth hurt. My jaw locked. But I did it. And when I bit into a banana two days later without crying? Worth it. Also-baking soda rinse? Life-changing. No fancy products needed. Just patience, cold, and a little stubbornness. You got this.