CYP2C9 and VKORC1 gene variants significantly affect warfarin dosing and bleeding risk. Genetic testing can reduce dangerous side effects by up to 32% in the first 90 days of therapy.
Warfarin Genetics: How Your DNA Affects Blood Thinner Dosing
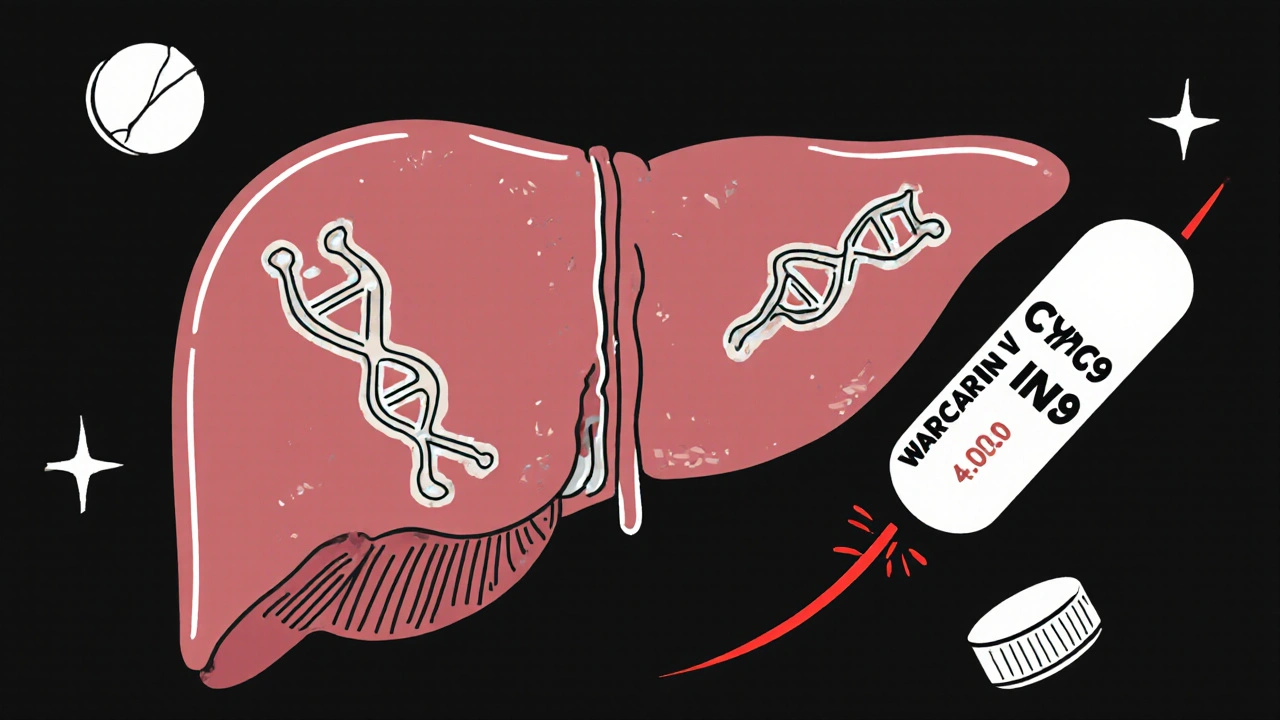
When you take warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it’s one of the most commonly prescribed anticoagulants—but it’s also one of the trickiest to get right. Why? Because your genes play a huge role in how your body handles it. Two key genes, CYP2C9, an enzyme that breaks down warfarin in the liver, and VKORC1, a gene that controls how sensitive your blood is to warfarin, can make your ideal dose 20% higher or 50% lower than someone else’s. This isn’t guesswork—it’s science backed by decades of research.
Most people think warfarin dosing is all about diet, alcohol, or other meds. And yes, vitamin K intake matters—so does the advice to keep your greens consistent. But if your CYP2C9 variant is slow to metabolize warfarin, even a perfect diet won’t stop your INR from spiking. Same goes for VKORC1: if your version makes you ultra-sensitive, a standard 5mg dose could put you at risk of bleeding. That’s why hospitals and clinics now routinely test for these variants before starting therapy. It’s not just for high-risk patients anymore. If you’ve ever had your warfarin dose changed after a blood test, or if your doctor said, ‘We’re lowering your dose because your INR was too high,’ there’s a good chance your genes were the real reason.
And it’s not just about avoiding bleeding. Getting your dose right faster means fewer hospital visits, less time spent in the clinic for INR checks, and more confidence that your treatment is working. Studies show that patients who get genetically guided dosing reach their target INR 20% faster than those who don’t. That’s not a small win—it’s life-changing for someone recovering from a stroke or dealing with a mechanical heart valve. The good news? You don’t need a fancy genetic test to start understanding this. If you’ve been on warfarin for more than a few months and still struggle with unstable INR, ask your doctor: ‘Could my genes be affecting my dose?’ It’s a simple question with huge consequences.
Below, you’ll find real-world guides that connect warfarin genetics to everyday life—from how vitamin K interacts with your genes, to what happens when you mix warfarin with other meds, to how to track your INR without panic. These aren’t theoretical articles. They’re written by people who’ve been there, tested the science, and found what actually works.