Antihistamine Blood Pressure Calculator
How This Tool Works
Enter your current blood pressure and select your antihistamine type to see potential effects. Results are based on clinical data from the article.
When you're dealing with allergies, antihistamines can be a lifesaver. But if you have high blood pressure, you might be wondering: are they safe? The short answer is yes - but only if you choose the right kind and know what to watch for. Many people assume all antihistamines raise blood pressure, but that’s not true. In fact, most modern options have little to no effect. The real risk comes from hidden ingredients, older drugs, or how your body processes them.
How Antihistamines Work - and Why They Might Affect Blood Pressure
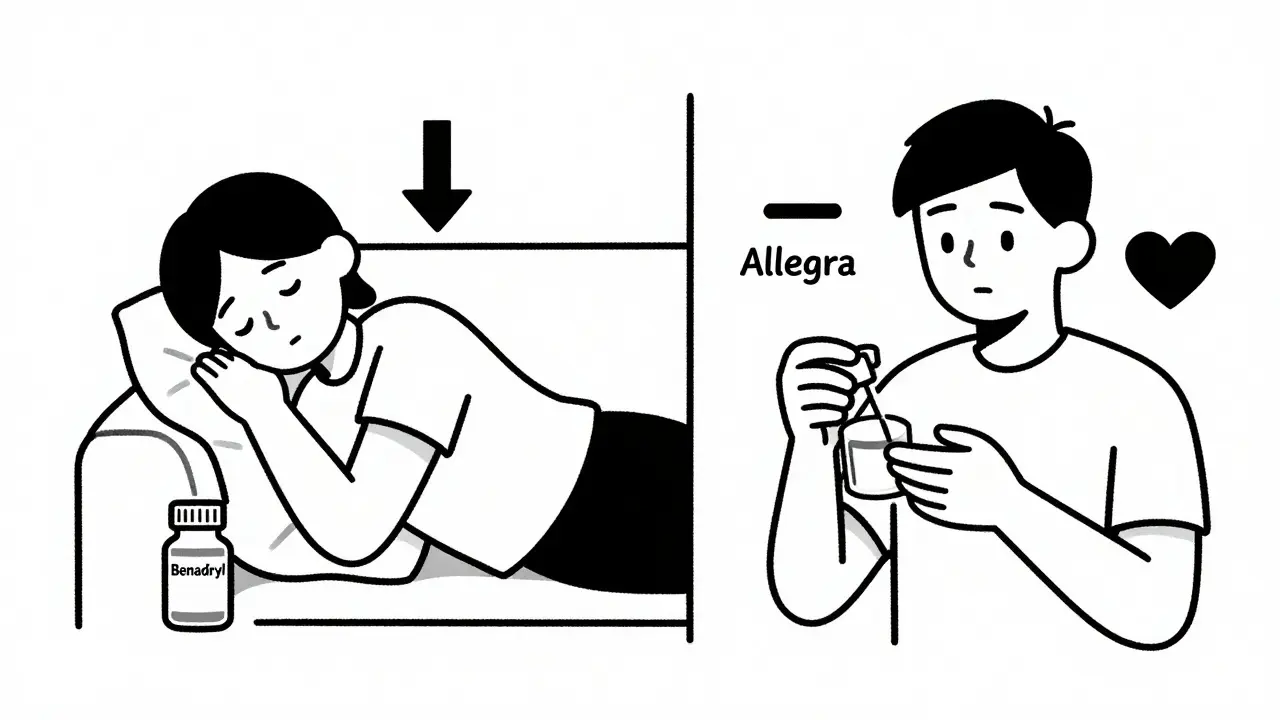
Antihistamines block histamine, a chemical your body releases during allergic reactions. Histamine causes swelling, itching, and runny nose - but it also affects your blood vessels. When histamine binds to H1 receptors, it makes blood vessels widen (vasodilation), which can lower blood pressure. So when you take an antihistamine, you’re stopping that effect. That might sound like it would raise blood pressure, but in practice, it rarely does - unless you’re using certain types. First-generation antihistamines like diphenhydramine (Benadryl) are strong blockers of H1 receptors and cross into the brain, which is why they make you drowsy. They also interfere with acetylcholine, leading to dry mouth, blurred vision, and sometimes a drop in blood pressure. IV diphenhydramine, used in emergency settings, can cause systolic blood pressure to fall by 8-12 mmHg within minutes. That’s why hospitals monitor patients after giving it. Second-generation antihistamines - like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - were designed to avoid the brain and minimize side effects. They don’t cross the blood-brain barrier well, so they don’t cause drowsiness. More importantly, they don’t significantly affect blood pressure in most people. Studies show 97% of patients on loratadine had no change in blood pressure. Cetirizine even showed potential benefits in early research, reducing inflammation markers linked to heart stress.The Real Danger: Combination Products with Decongestants
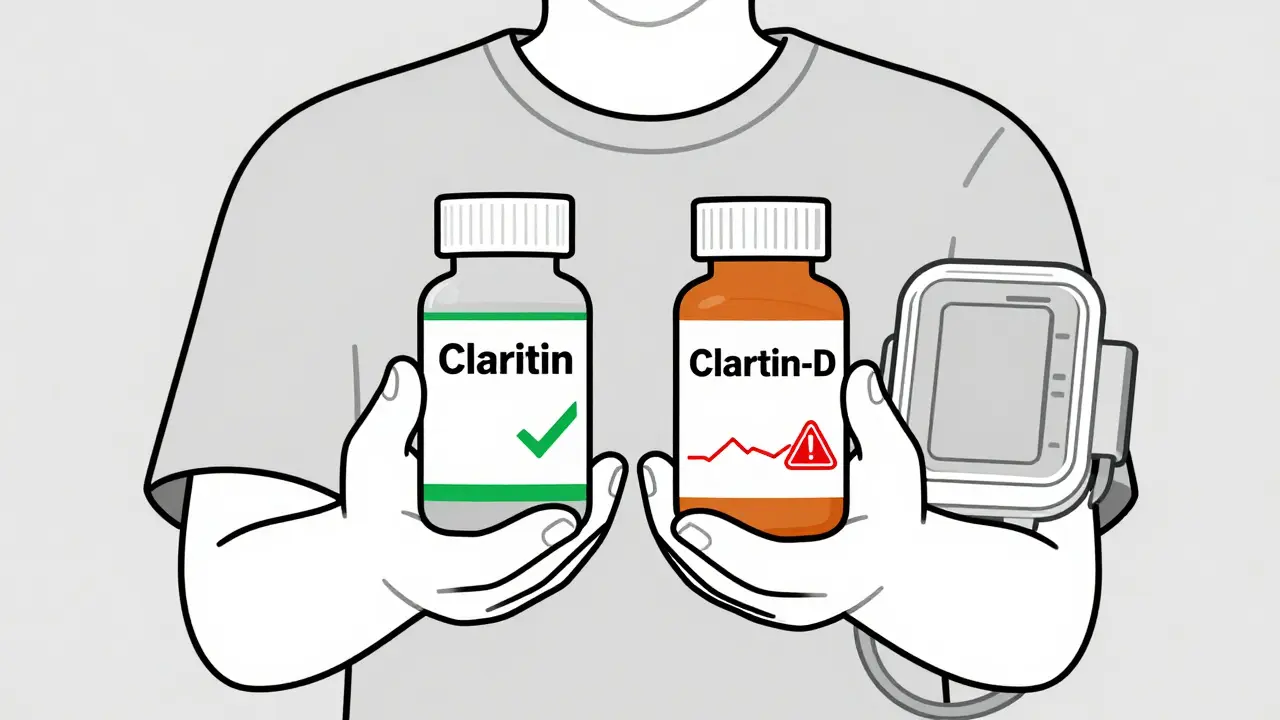
The biggest mistake people make is reaching for allergy meds that include decongestants. Products like Claritin-D, Zyrtec-D, or Sudafed PE contain pseudoephedrine or phenylephrine - ingredients that tighten blood vessels to relieve nasal congestion. That’s great for your nose, but not for your blood pressure. Pseudoephedrine can raise systolic blood pressure by about 1 mmHg on average. Sounds small, right? But in someone with uncontrolled hypertension, that’s enough to push readings into dangerous territory. A 2023 analysis of 12 clinical trials found that people taking pseudoephedrine combinations saw their systolic pressure rise by 5-10 mmHg. That’s not a minor fluctuation - it’s enough to increase stroke risk over time. Even over-the-counter pain relievers mixed with antihistamines can be risky. Ibuprofen combinations can lift blood pressure by 3-4 mmHg. Acetaminophen, often seen as safe, can add another 5 mmHg when taken at the maximum daily dose of 4,000 mg. If you’re already on blood pressure meds, these small spikes can add up.First-Gen vs. Second-Gen: A Clear Safety Divide
Here’s how the two generations stack up:| Antihistamine | Generation | Typical Blood Pressure Effect | Key Risks |
|---|---|---|---|
| Diphenhydramine (Benadryl) | First | Mild drop (especially IV) | Orthostatic hypotension, dizziness, interactions with CYP enzymes |
| Loratadine (Claritin) | Second | Neutral | Very low risk; safe for most with hypertension |
| Cetirizine (Zyrtec) | Second | Neutral to slightly beneficial | Minimal risk; may reduce inflammation |
| Fexofenadine (Allegra) | Second | Neutral | Least drug interactions; safest for liver-impaired patients |
| Pseudoephedrine (in Claritin-D, etc.) | Decongestant | Rises by 5-10 mmHg | High risk for uncontrolled hypertension |
What’s clear? Stick with second-generation antihistamines. They’re not just safer - they’re more effective long-term. First-gen drugs like diphenhydramine are outdated for daily use. They’re fine for occasional sleep aid or severe reactions, but not for managing seasonal allergies if you have high blood pressure.
Who Needs to Be Extra Careful?
Not everyone reacts the same way. Certain people need to take extra steps:- People with uncontrolled hypertension - If your systolic pressure is above 140 mmHg, check your blood pressure 2-4 hours after taking any new antihistamine.
- Those on multiple blood pressure meds - Antihistamines can interact with beta-blockers or diuretics, especially if you’re also taking grapefruit juice or certain antibiotics like erythromycin.
- People with heart rhythm issues - Avoid older drugs like terfenadine or astemizole (both pulled from the market in 1999). Even now, some generic versions linger in other countries. These can dangerously prolong the QT interval on an ECG, leading to arrhythmias.
- Patients with liver disease - Many antihistamines are processed by the liver. If your liver isn’t working well, drugs can build up. Fexofenadine is the best option here because it’s mostly eliminated unchanged through the kidneys.
Genetics also play a role. About 7% of people have a slow CYP2D6 enzyme, which affects how they break down diphenhydramine. That means the drug sticks around longer, increasing side effects. Some hospitals now test for this before prescribing - especially in older adults or those with heart conditions.
How to Monitor Your Blood Pressure Safely
You don’t need to check your blood pressure every day. But here’s what to do when starting a new antihistamine:- Take your baseline reading at home for 3 days before starting.
- Take your first dose in the morning, and check your blood pressure again after 30 minutes (for first-gen) or 2-4 hours (for second-gen).
- Repeat for the next 2-3 days, especially if you feel dizzy, lightheaded, or your heart races.
- If your systolic pressure rises more than 10 mmHg above baseline, stop the medication and talk to your doctor.
- Use a validated home monitor - wrist and finger devices are unreliable. Arm cuffs are best.
Keep a simple log: date, time, medication, reading. Bring it to your next appointment. Many doctors don’t ask about OTC meds - but they should.

Real Stories: What Patients Are Saying
Online forums show how real people manage this. On Reddit’s r/Allergy, a user named u/HypertensionWarrior wrote: “I had an allergic reaction during a skin test. They gave me IV Benadryl. My systolic dropped from 138 to 126 in 30 minutes. They made me sit for 20 minutes before letting me leave.” That’s normal - and why clinics monitor patients after IV doses. Another user reported: “I took Claritin-D for a week. My BP jumped from 128/80 to 142/88. Switched back to plain Claritin - back to normal in two days.” A 2022 survey of over 4,300 patients found that 89% of those using pure second-gen antihistamines saw no change. But 47% of those using decongestant combos saw spikes. The message is clear: avoid the “D” unless your doctor says it’s okay.What the Experts Say Now
The American Heart Association updated its guidelines in 2022: pure antihistamines are safe for most people with high blood pressure. No routine monitoring needed - unless you’re high-risk. The American College of Allergy, Asthma & Immunology recommends second-generation antihistamines as first-line treatment for anyone with heart disease. They explicitly warn against terfenadine, astemizole, and any product with pseudoephedrine unless you’re under close supervision. Even newer research is promising. A 2023 study showed cetirizine reduced endothelial inflammation by 22% in hypertensive patients - meaning it might help protect blood vessels, not just stop sneezing.What to Do Today
If you have high blood pressure and take antihistamines:- Check the label. Is there a “-D” or “decongestant”? If yes, switch to the plain version.
- Look for loratadine, cetirizine, or fexofenadine. These are your safest bets.
- Don’t take diphenhydramine daily. It’s not meant for long-term use.
- If you’re unsure, ask your pharmacist. They can scan your meds and flag interactions.
- Keep a blood pressure log for 3 days before and after starting any new allergy med.
There’s no need to suffer through allergies because you’re afraid of your blood pressure. With the right choice, you can breathe easy - literally and figuratively.
Can antihistamines raise blood pressure?
Most second-generation antihistamines like loratadine, cetirizine, and fexofenadine do not raise blood pressure. The real risk comes from combination products that include decongestants like pseudoephedrine, which can increase systolic pressure by 5-10 mmHg. First-generation antihistamines like diphenhydramine may cause a slight drop in blood pressure, especially when given intravenously.
Is Benadryl safe if I have high blood pressure?
Diphenhydramine (Benadryl) is not recommended for daily use if you have high blood pressure. It can cause dizziness, low blood pressure, and interactions with other medications. While it doesn’t typically raise blood pressure, it can lead to orthostatic hypotension - a sudden drop when standing up - which increases fall risk. Use it only for short-term, occasional relief.
What’s the safest antihistamine for someone with hypertension?
Fexofenadine (Allegra) is considered the safest for people with high blood pressure because it has minimal drug interactions and is not metabolized by the liver. Loratadine (Claritin) and cetirizine (Zyrtec) are also excellent choices. All three are second-generation antihistamines with no significant effect on blood pressure in clinical studies.
Can I take allergy medicine with my blood pressure pills?
You can, but only if you choose the right allergy medicine. Avoid anything with pseudoephedrine, phenylephrine, or ibuprofen. Stick to plain loratadine, cetirizine, or fexofenadine. Be cautious with grapefruit juice - it can interfere with how your body processes some antihistamines. Always check with your pharmacist before combining medications.
Do I need to check my blood pressure every day when taking antihistamines?
No, not every day. But if you’re starting a new antihistamine, check your blood pressure before you take it, then again 2-4 hours later. Do this for the first 3 days. If your systolic pressure rises more than 10 mmHg above your normal baseline, stop the medication and contact your doctor. Otherwise, routine daily monitoring isn’t needed unless you have uncontrolled hypertension.
9 Comments
Bobby Collins
January 2 2026
they're hiding the truth again. antihistamines are just the tip of the iceberg. did you know the FDA approved these drugs because big pharma funded the studies? they want you dependent on pills while your blood pressure creeps up. they don't care if you live or die as long as you keep buying. check the ingredients in your 'safe' claritin - it's all connected to the same corporate machine.
Layla Anna
January 3 2026
i just switched to zyrtec after reading this and my bp dropped like magic 😊 i used to get dizzy all the time with benadryl but now i can actually sleep without feeling like my head’s gonna explode. thank you for writing this! 💙
Heather Josey
January 4 2026
This is an exceptionally well-researched and clinically grounded article. As a healthcare professional, I appreciate the clear distinction between first- and second-generation antihistamines, and the emphasis on decongestants as the primary risk factor. The inclusion of specific BP thresholds, pharmacokinetic considerations, and monitoring protocols elevates this beyond typical patient advice. I will be sharing this with my hypertensive patients immediately. Thank you for the thoroughness and precision.
Alex Warden
January 5 2026
usa got it right. europe is still pushing dangerous junk. if you’re american and you take benadryl for allergies you’re dumb. just take claritin like everyone else. no drama. no risk. simple. america wins again.
LIZETH DE PACHECO
January 6 2026
this was exactly what i needed to hear. i’ve been scared to take anything for my allergies for years because i didn’t want to mess with my meds. now i feel confident switching to allegra. thank you for making it so clear and not scary. you just made my life easier 💪
Lee M
January 6 2026
the body doesn’t need antihistamines. allergies are a symptom of systemic toxicity. pharmaceuticals are band-aids on a bullet wound. the real solution is detoxing the liver, alkalizing the blood, and reconnecting with nature. but they won’t tell you that because nature doesn’t have a patent.
Matthew Hekmatniaz
January 7 2026
i’ve been on blood pressure meds for 12 years and took zyrtec-d for two winters thinking it was fine. my bp jumped 15 points. switched to plain zyrtec and everything normalized. this post saved me from a stroke. thanks to everyone who contributed to the research. we need more of these clear, evidence-based guides in a world full of noise.
Liam George
January 9 2026
the cyp2d6 polymorphism data is selectively presented. why isn't there mention of the 2018 NIH study linking cetirizine to mitochondrial dysfunction in elderly patients with subclinical cardiac impairment? the data is suppressed because it contradicts the narrative. they want you believing it's safe while the epigenetic damage accumulates silently. ask yourself: who benefits from you thinking this is just about 'decongestants'?
gerard najera
January 9 2026
Second-gen safe. Decongestants dangerous. That’s it.