Immunosuppressants keep transplanted organs alive but come with serious risks like infection, cancer, and organ damage. Learn how to take them safely, avoid rejection, and live longer with your transplant.
Organ Transplant Side Effects: What You Need to Know
When someone gets an organ transplant, a surgical procedure to replace a failing organ with a healthy one from a donor. Also known as solid organ transplantation, it’s often the only option left for people with end-stage organ failure. But surviving the surgery is just the beginning—long-term survival depends on managing immunosuppressants, medications that stop your immune system from attacking the new organ—and dealing with the side effects that come with them.
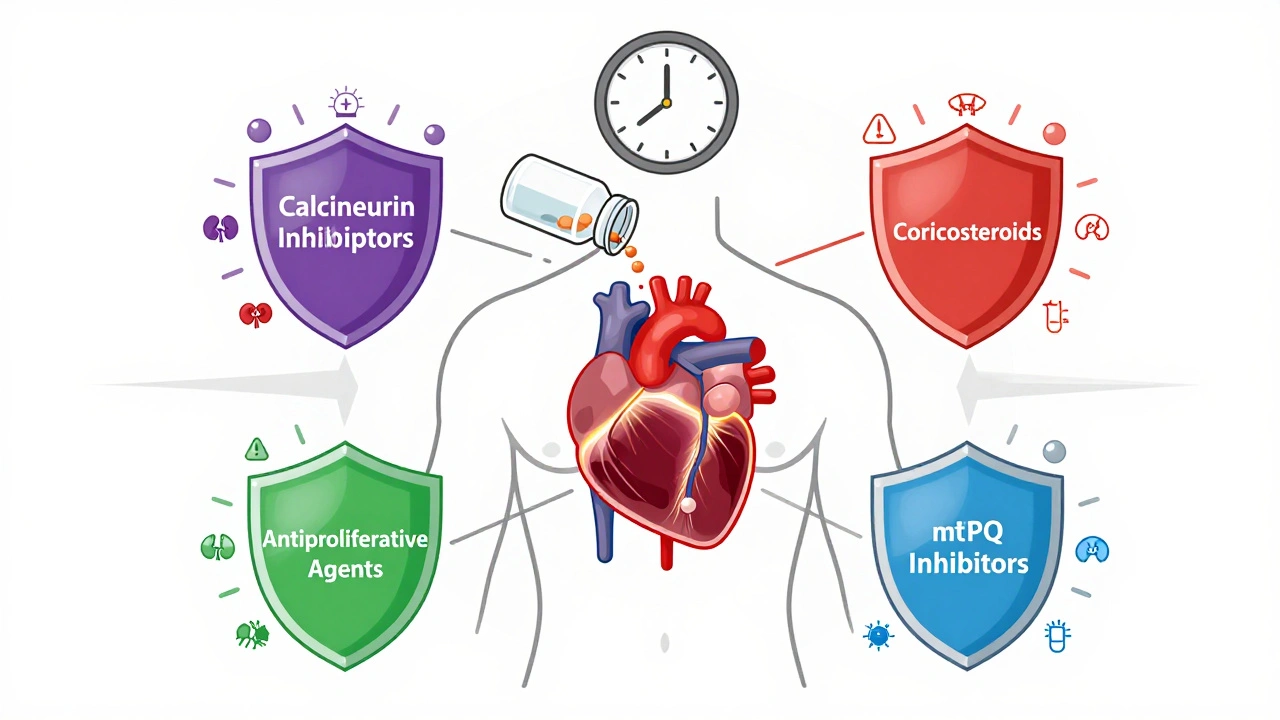
These drugs are essential. Without them, your body sees the new kidney, liver, or heart as an invader and tries to destroy it. That’s transplant rejection, the immune system’s attack on the transplanted organ. But suppressing your immune system opens the door to other problems: infections, kidney damage, high blood pressure, diabetes, and even certain cancers. And then there’s steroid myopathy, muscle weakness caused by long-term use of corticosteroids like prednisone, a common part of transplant regimens. It’s not painful, so many patients don’t notice it until they can’t climb stairs or stand up from a chair. These aren’t rare side effects—they’re expected, and they’re managed daily by millions of transplant recipients.
What you won’t find in brochures are the quiet struggles: the fear of missing a pill, the weight gain from steroids, the constant checkups, the anxiety over every fever. Some people get lucky—few side effects, stable function. Others fight a slow battle with high cholesterol, nerve damage, or bone thinning. The key isn’t avoiding side effects—it’s spotting them early and adjusting before they spiral. That’s why knowing the signs matters more than memorizing drug names. If your muscles feel weak, your blood sugar spikes, or you get sick more often than before, it’s not just bad luck. It’s your body telling you something about your meds.
The posts below cover exactly this: how transplant medications work, what side effects actually look like in real life, and how to protect yourself without stopping treatment. You’ll find guides on spotting steroid myopathy, managing drug interactions, understanding rejection symptoms before they become emergencies, and how to stay healthy long after the hospital stay ends. This isn’t theoretical. These are the tools people who’ve been through it use every day.