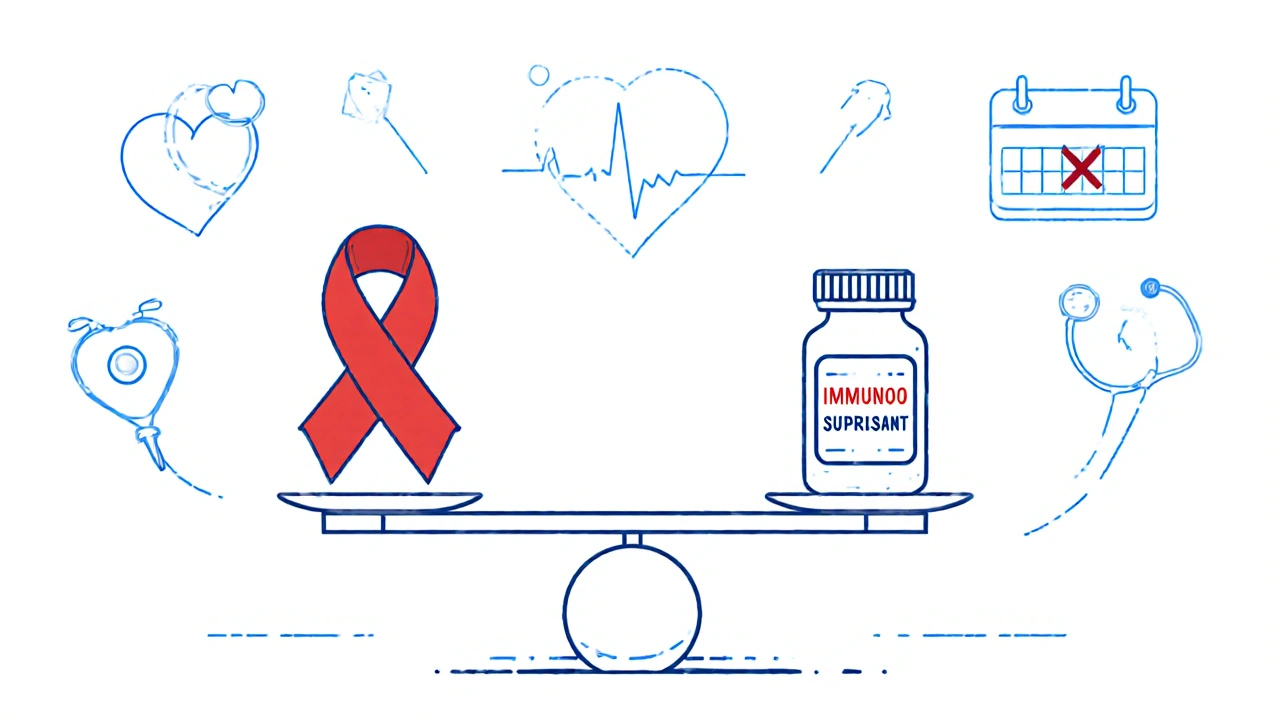
New research shows immunosuppressants don’t increase cancer recurrence risk. Learn how anti-TNF drugs, methotrexate, and biologics are safe for cancer survivors-and why the old 5-year waiting rule is outdated.
Cancer Recurrence: What It Means, What to Watch For, and How to Fight Back
When cancer recurrence, the return of cancer after a period of remission following treatment. Also known as cancer relapse, it happens when some cancer cells survive treatment and grow again, sometimes months or even years later. It’s not a failure—it’s a reality many cancer survivors face, and knowing what to look for makes all the difference.
Cancer recurrence isn’t one thing. It can show up in the same place as the original tumor (local recurrence), nearby lymph nodes (regional), or far away in organs like the lungs, liver, or bones (distant). The type of cancer, how advanced it was at diagnosis, and the treatment you got all play a role. But even with the best care, tiny clusters of cells can hide and wake up later. That’s why ongoing monitoring isn’t optional—it’s part of survival. Blood tests, scans, and physical exams aren’t just routine checks. They’re your early warning system.
Some signs are obvious: a new lump, unexplained weight loss, constant fatigue, or pain that won’t go away. Others are quiet—like a cough that won’t clear, changes in bowel habits, or skin changes that don’t heal. For people who’ve had breast, colon, or skin cancer, regular self-checks are lifesavers. For others, tracking symptoms with a simple journal helps spot patterns doctors might miss. And while you can’t control everything, lifestyle choices matter. Studies show that staying active, eating real food, avoiding smoking, and limiting alcohol can lower the chance of recurrence for many types of cancer. It’s not about perfection. It’s about consistency.
You’re not alone in this. Many of the guides below come from people who’ve walked this path—managing side effects from chemo, dealing with skin reactions from targeted therapies, or learning how to track medications that help prevent recurrence. Some share how they used visual dosing tools to stay on top of daily pills. Others explain how drug interactions or storage conditions can quietly affect your recovery. One post breaks down how capecitabine can cause mouth sores, a common issue for people on certain regimens. Another talks about how warfarin and vitamin K levels need to stay balanced, especially if you’re on long-term treatment. These aren’t abstract topics. They’re daily realities for people fighting cancer recurrence.
What you’ll find here isn’t theory. It’s what works in real life. From knowing when to ask for a second scan to understanding which supplements might help—or hurt—this collection gives you the tools to stay alert, informed, and in control. No fluff. No fearmongering. Just clear, practical steps you can use today to protect your health long after treatment ends.