Pseudotumor Cerebri Medication Risk Checker
Is This Medication Risk Right for You?
Pseudotumor cerebri can develop from certain medications. This tool helps you understand your risk based on medications you're taking and symptoms you're experiencing.
It's important to note that this tool doesn't replace medical advice. If you experience headaches or vision changes while on these medications, see a doctor immediately.
Select Your Medications
-
MinocyclineMost common trigger in young adults (1 in 7,500 prescriptions)
-
Isotretinoin (Accutane)Causes IIH in 15-20% of medication-related cases
-
Corticosteroid withdrawalMost dangerous trigger (up to 18% permanent vision loss)
-
Growth hormone therapy22% of pediatric cases show vision changes before headaches
-
Excess vitamin AHigh-dose supplements can trigger the condition
Check for Symptoms
- Worsening headaches when lying down
- Vision changes (blurring, dimming, or seeing spots)
- Double vision or difficulty focusing
- Pulsatile tinnitus (ringing in ears)
- No nausea or light sensitivity (unlike migraines)
When a headache feels like it’s crushing your skull, and your vision starts to blur or go dark for a few seconds, it’s easy to blame stress, lack of sleep, or a sinus infection. But what if it’s something far more serious - and directly tied to a medication you’re taking? Pseudotumor cerebri, now more accurately called idiopathic intracranial hypertension (IIH), is a condition where pressure builds up inside your skull, mimicking a brain tumor - even though no tumor exists. And in 10-15% of cases, it’s not random. It’s caused by common medications.
What Exactly Is Medication-Induced Pseudotumor Cerebri?
Pseudotumor cerebri happens when cerebrospinal fluid (CSF), the liquid that cushions your brain and spinal cord, builds up to dangerous levels. Normal CSF pressure is between 70 and 180 mm H₂O. In this condition, it spikes above 250 mm H₂O. That pressure pushes on your optic nerves and brain, causing severe headaches and vision problems. The term “false brain tumor” was coined because the symptoms - intense head pain, blurred vision, even temporary blindness - look exactly like a tumor on imaging. But scans show nothing.
It’s not rare. In the U.S., about 8,000 to 10,000 new cases happen every year from medications alone. The real danger? Permanent vision loss. Up to 10% of untreated cases lose vision permanently. And unlike migraines or tension headaches, this isn’t something you can just pop an Advil and wait out.
Which Medications Trigger It?
Not all drugs cause this. But some are well-documented triggers, and they’re more common than you think.
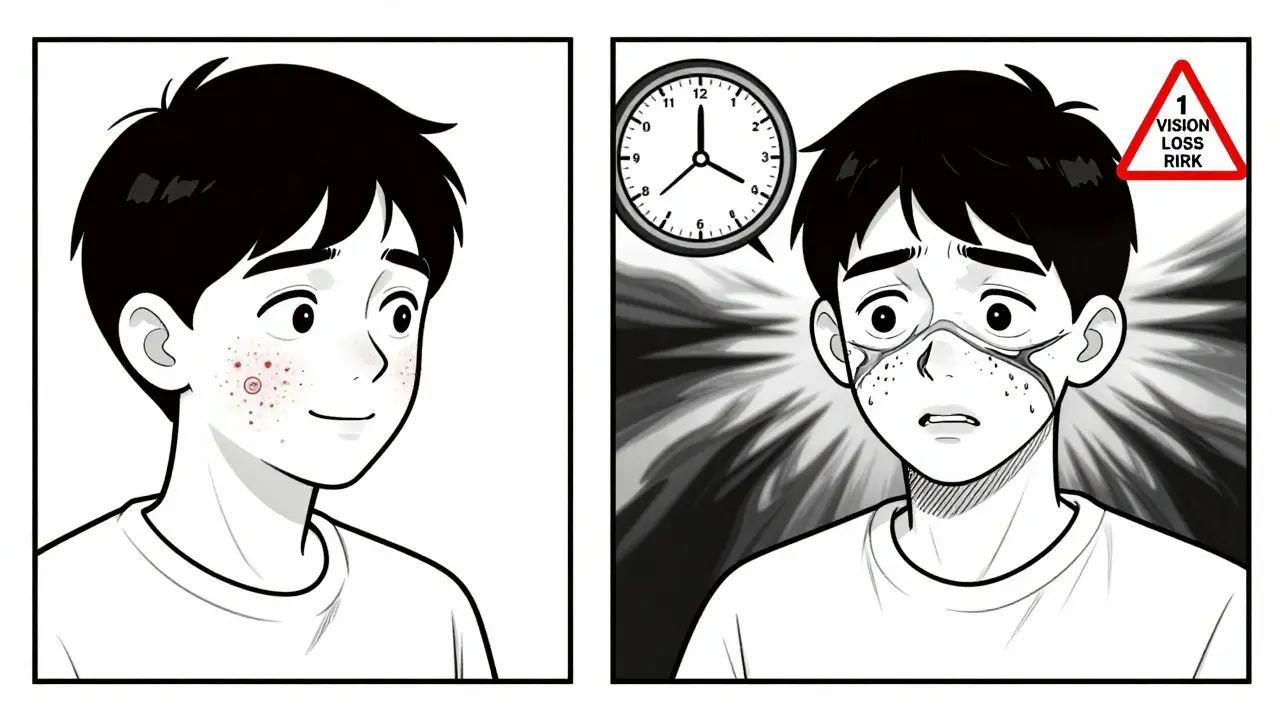
- Minocycline (a type of tetracycline antibiotic): This is the most common culprit in young adults. It’s often prescribed for acne or rosacea. Studies show 1 in every 7,500 prescriptions leads to IIH. Symptoms usually appear 1 to 6 months after starting it.
- Isotretinoin (Accutane): Used for severe acne, this drug can cause IIH in 15-20% of medication-related cases. Vision changes can start as early as 4 weeks after beginning treatment. In some cases, visual field damage happens within 2 weeks of the first headache.
- Corticosteroid withdrawal: Stopping prednisone or similar drugs after long-term use can trigger a spike in CSF pressure. This happens in 10-15% of cases, often 1 to 3 weeks after stopping. It’s the most dangerous trigger - up to 18% of patients with this form suffer permanent vision loss.
- Growth hormone therapy: In children, this can lead to IIH. Alarmingly, in 22% of pediatric cases, vision changes appear before headaches at all.
- Excess vitamin A: High-dose supplements or multivitamins with megadoses of vitamin A can also trigger this condition.
Here’s the scary part: using two of these together - like minocycline and isotretinoin - increases your risk by more than 7 times. This isn’t theoretical. A 2022 study of 142 patients found that nearly every case of severe vision loss involved patients on multiple triggering drugs.
How Do You Know It’s Not Just a Migraine?
Most people with medication-induced IIH first see their primary care doctor for “bad headaches.” In fact, 65-70% of these cases are misdiagnosed as migraines or sinus infections. But there are red flags that set it apart:
- Headaches get worse when lying down - unlike migraines, which often improve with rest.
- Visual obscurations: Brief episodes (5-15 seconds) where your vision goes gray or black, especially when standing up or bending over.
- Double vision or difficulty focusing - caused by pressure on the nerves controlling eye movement.
- Ringing in the ears (pulsatile tinnitus) that matches your heartbeat.
- No nausea or light sensitivity - common in migraines but rare in IIH.
One patient, sharing on a rare disease forum, described it perfectly: “I thought it was stress headaches. Then I started seeing gray spots every time I stood up. By the time I got to a neurologist, I’d already lost 20% of my peripheral vision.”
Why Vision Loss Happens So Fast
The optic nerve sits inside the skull. When pressure builds, it squeezes the nerve like a kinked hose. The nerve can’t send signals properly. First, you get transient blurring. Then, blind spots form in your peripheral vision. Left unchecked, the nerve dies. That damage is permanent.
Medication-induced IIH is especially aggressive. While idiopathic cases (no clear cause) take months to damage vision, medication-triggered cases can do it in weeks. Data from UVA Health shows 40% of patients with drug-induced IIH have major visual field defects within 4 weeks - compared to 25% in idiopathic cases.
And here’s the kicker: many patients don’t notice the warning signs until it’s too late. A 2022 survey of 318 patients found that 63% waited 4 to 12 weeks before getting a correct diagnosis. Doctors missed it because they weren’t looking for it.
How It’s Diagnosed
There’s no single test. Diagnosis requires a combination:
- Lumbar puncture (spinal tap): This is the gold standard. A needle measures CSF pressure. If it’s above 250 mm H₂O, and your brain scan is normal, you have IIH.
- Optical coherence tomography (OCT): This scan measures the thickness of the retinal nerve fiber layer. A spike of 15-20 microns within the first week is a strong early indicator.
- Visual field testing: A machine tests your peripheral vision. The earliest sign? A loss in the upper outer quadrant - a pattern so consistent, it’s now used to confirm diagnosis.
- Eye exam: Doctors look for papilledema - swelling of the optic nerve head. It’s visible with an ophthalmoscope.
And timing matters. If you’ve been on minocycline for 3 months and suddenly get daily headaches, your doctor should suspect this - even if you’re young and healthy. The delay between starting a drug and symptoms (1-6 weeks) makes it easy to miss.
What Happens After Diagnosis?
The good news? If caught early, it’s often reversible.
- Stop the drug: This is step one. For isotretinoin or minocycline, stopping the medication alone leads to improvement in 80% of cases.
- Medication to reduce pressure: Acetazolamide (Diamox) is the standard. It reduces CSF production. A new drug, venglustat, was approved in 2023 and shows 37% better pressure reduction than acetazolamide in trials.
- Weight management: Though less critical in medication-induced cases than in idiopathic ones, losing weight can still help.
- Surgery: In severe cases, a shunt may be placed to drain fluid. Or a nerve sheath fenestration may be done to relieve pressure on the optic nerve.
Recovery isn’t instant. Headaches can linger for months. Vision may improve slowly. But if you stop the drug early, most people regain full vision. One patient reported complete recovery after stopping minocycline and taking acetazolamide for 6 weeks - though headaches took 4 months to vanish.
Why This Is Still Underdiagnosed
Doctors aren’t trained to connect the dots. A 2022 study in Neurology Today found that primary care physicians misdiagnose this condition in 65-70% of cases. They see a headache. They see acne treatment. They don’t think: “Could this be pressure building inside the skull?”
Also, many patients don’t know to mention their vision changes. They think blurring is just eye strain. Or they assume their doctor already knows about the risks of isotretinoin - but even if they do, monitoring isn’t always done.
Regulatory agencies like the FDA and EMA now require monthly eye exams for isotretinoin users. In the EU, this cut permanent vision loss from 12% to 4.7%. But compliance varies. And for antibiotics like minocycline? No such requirement exists.
What You Should Do If You’re on These Drugs
If you’re taking any of these medications - especially minocycline, isotretinoin, or corticosteroids - here’s what to do:
- Know the warning signs: Headaches that get worse lying down, vision that dims for seconds, double vision, or ringing in your ears.
- Don’t wait: If you have these symptoms, see a neurologist or neuro-ophthalmologist - not just your GP.
- Ask for a lumbar puncture: If your doctor dismisses you, insist on CSF pressure testing. It’s the only way to confirm.
- Track your symptoms: Keep a log: when headaches start, how long they last, if vision changes happen.
- Never stop corticosteroids abruptly: Always taper under medical supervision.
And if you’re on more than one of these drugs? Talk to your doctor about alternatives. There are other acne treatments. Other antibiotics. Other ways to manage inflammation. The risk isn’t worth it.
The Bigger Picture
Medication-induced pseudotumor cerebri isn’t just a rare side effect. It’s a systemic blind spot in medicine. We’ve got powerful drugs that help millions - but we’re not monitoring the hidden dangers well enough.
Between 2015 and 2023, minocycline-induced cases rose by 217% - mostly because it’s now used for rosacea, not just acne. And with more teens getting both isotretinoin and minocycline together, we’re heading for a wave of preventable vision loss.
Research is moving forward. A 2023 study from Johns Hopkins found three specific inflammatory markers that appear only in medication-triggered IIH - a potential blood test to distinguish it from other causes. The IIH Registry Project, launched in January 2023, is tracking 500 patients to finally map out exact timelines for each drug.
But until then, awareness is your best defense. If you’re on a medication that could cause this, and you have new headaches or vision changes - don’t assume it’s nothing. Push for answers. Your eyesight might depend on it.
Can pseudotumor cerebri be caused by over-the-counter supplements?
Yes. High-dose vitamin A supplements - especially those exceeding 10,000 IU daily - can trigger pseudotumor cerebri. This includes some multivitamins, acne treatments, and liver health formulas. The risk is low, but it’s real. If you’re taking high-dose vitamin A and develop headaches or vision changes, stop the supplement and get checked.
Is pseudotumor cerebri permanent if I don’t stop the medication?
Vision loss from pseudotumor cerebri can become permanent if pressure isn’t lowered quickly. Studies show 5-10% of untreated cases result in irreversible damage. The longer you wait, the higher the risk. In corticosteroid withdrawal cases, up to 18% of patients lose vision permanently if not treated within 3 weeks of symptom onset. Early action saves sight.
Do I need to stop all medications if I’m diagnosed?
You should stop the specific medication suspected of causing the condition - not all of them. For example, if minocycline is the trigger, you stop that. You don’t necessarily stop your birth control or blood pressure pills. But if you’re on multiple triggers (like minocycline and isotretinoin), both must be discontinued. Always work with your doctor to find safe alternatives.
Can children get pseudotumor cerebri from medication?
Yes. Growth hormone therapy, corticosteroids, and tetracycline antibiotics (like minocycline) can trigger IIH in children. In fact, in 22% of pediatric cases, vision changes appear before headaches. That’s why regular eye exams are required for kids on growth hormone. Parents should watch for complaints of blurred vision, eye pain, or difficulty seeing at night.
How long does it take to recover after stopping the drug?
Vision often improves within 4-8 weeks after stopping the triggering drug. Headaches may take longer - up to 4 months. Most patients regain full vision if they stop the medication early and take pressure-lowering drugs like acetazolamide. Recovery is slower if the condition was ignored for months. The key is speed: the sooner you act, the better the outcome.

15 Comments
Mike Hammer
February 15 2026
Been on minocycline for my rosacea for 6 months. Started getting these weird headaches last week. Thought it was just stress. Then yesterday I stood up and my vision went black for like 5 seconds. Didn't think twice. Went to the doc today and they did a lumbar puncture. CSF pressure was 280. Holy shit. I'm stopping the med tomorrow. If you're on this stuff and have headaches + vision weirdness? Don't wait. Go now.
Daniel Dover
February 16 2026
Stop isotretinoin immediately if vision changes. No exceptions.
Chiruvella Pardha Krishna
February 16 2026
The human body is not a machine to be dosed like a circuit board. We have forgotten that medicine is not chemistry alone, but a dance between biology and awareness. The pharmaceutical industry, in its infinite wisdom, markets drugs as solutions without acknowledging the silent, creeping cost - the erosion of perception. Pseudotumor cerebri is not a side effect. It is a message. A whisper from the nervous system saying: you are not listening.
Joe Grushkin
February 18 2026
So let me get this straight - you’re telling me that a teenager on acne meds could go blind because no one thought to check intracranial pressure? This isn’t medicine. This is negligence dressed up in white coats. And now we’re supposed to be grateful they’re finally ‘studying’ it? Pathetic. The FDA should have mandated eye exams for minocycline a decade ago. But no - profit over patients. Again.
Virginia Kimball
February 19 2026
I had this. Took me 10 weeks to get diagnosed because my GP thought it was migraines. By the time I saw a neuro-ophthalmologist, I’d lost 15% of my peripheral vision. Took 6 months to get it back. Acetazolamide was a nightmare - I felt like a zombie. But I’m alive and I can still drive. If you’re on any of these meds and have weird headaches? Don’t be polite. Demand the spinal tap. Seriously. Your eyes are worth more than your doctor’s schedule.
Kapil Verma
February 20 2026
India has the highest number of acne cases in the world. We are a nation of youth, of glowing skin, of Instagram filters. But who warns the 17-year-old girl on isotretinoin? Who tells her that her vision might vanish while she’s trying to look perfect? We are not taught to question doctors. We are taught to obey. And now, because of this silence, we are losing our children’s sight. This is not a medical issue - it is a cultural failure. Someone must speak up. Someone must change the system. Not tomorrow. Today.
Michael Page
February 22 2026
I read this article and just sat there. No reaction. No emotion. Just… stillness. Because I know. I’ve seen it before. A friend. A cousin. A neighbor. All of them dismissed. All of them delayed. All of them damaged. And yet, the cycle continues. No outrage. No headlines. Just another quiet tragedy in a world that prefers distraction over diagnosis.
Mandeep Singh
February 22 2026
Let me tell you something. I work in a dermatology clinic in Mumbai. I’ve seen 14 cases of drug-induced IIH in the last 18 months. 12 of them were on minocycline + isotretinoin. Both prescribed together. No warning. No consent. No follow-up. One girl, 16 years old, went completely blind in one eye before we even got her to a neurologist. Her parents didn’t even know what isotretinoin was. They thought it was just a pill for acne. We need mandatory education. We need mandatory imaging. We need to stop treating patients like numbers. And we need to stop letting lazy doctors write scripts without thinking. This isn’t an accident. It’s negligence. And it’s preventable.
Betty Kirby
February 24 2026
People still don’t get it. Vitamin A isn’t just ‘supplements’. It’s in every damn multivitamin marketed to teens. ‘For glowing skin!’ ‘For immune support!’ ‘For healthy hair!’ Yeah, and also for crushing your optic nerve. If you’re taking more than 5,000 IU daily and you have headaches? You’re playing Russian roulette with your vision. Stop. Now. And get your eyes checked. No, ‘I feel fine’ isn’t good enough. Your optic nerve doesn’t care how you feel.
Josiah Demara
February 24 2026
Oh wow, another ‘medical mystery’ that’s been known for decades. The real scandal? No one’s sued. No one’s held accountable. Where are the class actions? Where are the lawsuits against the manufacturers who knew? They didn’t just fail to warn - they actively buried studies. Look up the 2017 internal Merck memo on isotretinoin and CSF pressure. It was redacted. That’s not an accident. That’s criminal. And yet, we’re still prescribing it like candy. This isn’t negligence. It’s corporate malfeasance. And we’re all complicit by not demanding justice.
Kaye Alcaraz
February 25 2026
Thank you for sharing this vital information. It’s critical that we all become advocates for our own health. If you’re on any of these medications, please prioritize your vision. Schedule an eye exam. Document your symptoms. Speak up. You deserve to be heard. Your health is worth the extra step.
Sarah Barrett
February 26 2026
The most chilling part isn’t the drugs - it’s how quietly this unfolds. No sirens. No emergency rooms. Just a girl staring at her phone, wondering why her peripheral vision feels… off. A guy shrugging off headaches as ‘stress’. A teen thinking ‘double vision’ means she needs new glasses. We’ve normalized the erosion of perception. And that’s the real tragedy. Not the medicine. The silence.
Erica Banatao Darilag
February 27 2026
i had this too. i was on minocycline for 4 months. started gettin headaches every night. i thought i was just tired. then i started seeing black spots when i stood up. i told my doc. she said 'maybe you need more sleep'. i went to a different doc. they did the lumbar puncture. pressure was 270. i cried. i was so scared. i stopped the med. took diamox. vision got better. headaches took 3 months. but i can see. please. if you're on these drugs and have ANY weird vision stuff. go. don't wait. don't be polite. your eyes are irreplaceable.
Charlotte Dacre
February 27 2026
So let me get this straight - we’re okay with teenagers going blind because we’re too lazy to check CSF pressure? Brilliant. Just brilliant. Next up: mandatory brain scans before giving out ibuprofen. At this rate, we’ll be prescribing helmets with IV drips just to walk to the fridge.
Esha Pathak
February 28 2026
Every time I see someone say 'just stop the drug', I think: what if you're a 14-year-old with severe acne and your parents can't afford alternatives? What if you're on steroids for lupus? What if you're a single parent with no insurance? Medicine isn't just about science - it's about access. We can't just say 'stop' and walk away. We need better systems. Cheaper tests. Real support. Otherwise, awareness is just another privilege.