When a patient walks into your office with a prescription for generic medications, what do you really think? Do you trust them? Do you worry? Or do you see them as a simple, smart way to cut costs without sacrificing care? For many providers, the answer isn’t straightforward. The science says generics work - but real-world experience tells a more complicated story.
They’re the Same… But Not Always
The FDA requires generic drugs to match brand-name drugs in active ingredients, strength, dosage form, and route of administration. More importantly, they must be bioequivalent: meaning they deliver the same amount of medicine into the bloodstream at the same rate. The acceptable range? 80% to 125% of the brand’s concentration. That’s not a guess - it’s a hard standard backed by pharmacokinetic studies measuring Cmax and AUC. For most drugs, this works perfectly. Statins like atorvastatin, blood pressure meds like lisinopril, and antidepressants like sertraline have been switched to generics for years. Providers report no difference in outcomes. In fact, studies show patients are more likely to stick with their meds when they’re cheaper. One analysis found 13% higher adherence for patients starting on generics versus brand-name versions. But here’s where it gets messy.The Drugs That Make Providers Wince
Not all medications play nice with substitution. For drugs with a narrow therapeutic index - where even small changes in blood levels can cause harm - providers are far more cautious. These include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Immunosuppressants like cyclosporine and tacrolimus
- Antiepileptic drugs like lamotrigine and phenytoin
Why Some Providers Still Hesitate
It’s not just about the science. It’s about control. Many providers feel blindsided when a pharmacist substitutes a generic without telling them - or worse, without telling the patient. In 24 U.S. states, pharmacists can switch a brand to a generic without notifying the prescriber. In 7 states and D.C., patient consent is required. That inconsistency creates confusion. A patient might get a different generic every refill - different pill color, different shape, different manufacturer. They start to think, “This isn’t the same.” And sometimes, they’re right. Not because the drug is unsafe, but because packaging and inactive ingredients vary. A patient with a rare allergy to a dye in one generic version might react, even if the active ingredient is identical. Or a patient with swallowing issues might struggle with a new tablet size. Providers who manage complex cases - like those on multiple chronic meds - often write “dispense as written” on prescriptions. It’s not about distrust. It’s about preventing chaos.
The Patient Perspective: Trust Is Everything
Patients don’t care about bioequivalence curves. They care about how they feel. And if they’ve had a bad experience - even if it was coincidental - they’ll blame the generic. A 2024 study in Greece found that 68% of women followed their doctor’s advice to switch to generics, compared to 64% of men. But only 30% of patients felt fully informed. Many didn’t know generics were the same drug. Some thought they were “cheap knockoffs.” That’s where education matters. A simple 30-second explanation - “This is the exact same medicine, just cheaper - no extra testing needed” - increases patient willingness to switch by 40%. Providers who involve patients in the decision report fewer complaints and better adherence. Pharmacists play a big role too. When they explain why a pill looks different - “This is the same levothyroxine, just made by a different company” - patients feel less anxious. But if they’re silent, fear fills the gap.Cost Savings Are Real - But Not Always Simple
In 2023, generics made up 90% of all prescriptions in the U.S. but only 23% of total drug spending. That’s over $130 billion saved annually. For Medicaid, Medicare Part D, and private insurers, generics are the backbone of affordability. A 2006-2007 Medicaid analysis showed that eliminating patient consent requirements for just three generics - atorvastatin, clopidogrel, and olanzapine - could have saved over $100 million in one year. That’s real money. Real relief for patients struggling to afford meds. But here’s the catch: forcing substitution without context backfires. States with strict consent laws had 25% lower generic use - meaning more people stayed on expensive brand drugs. That didn’t protect safety. It just cost more.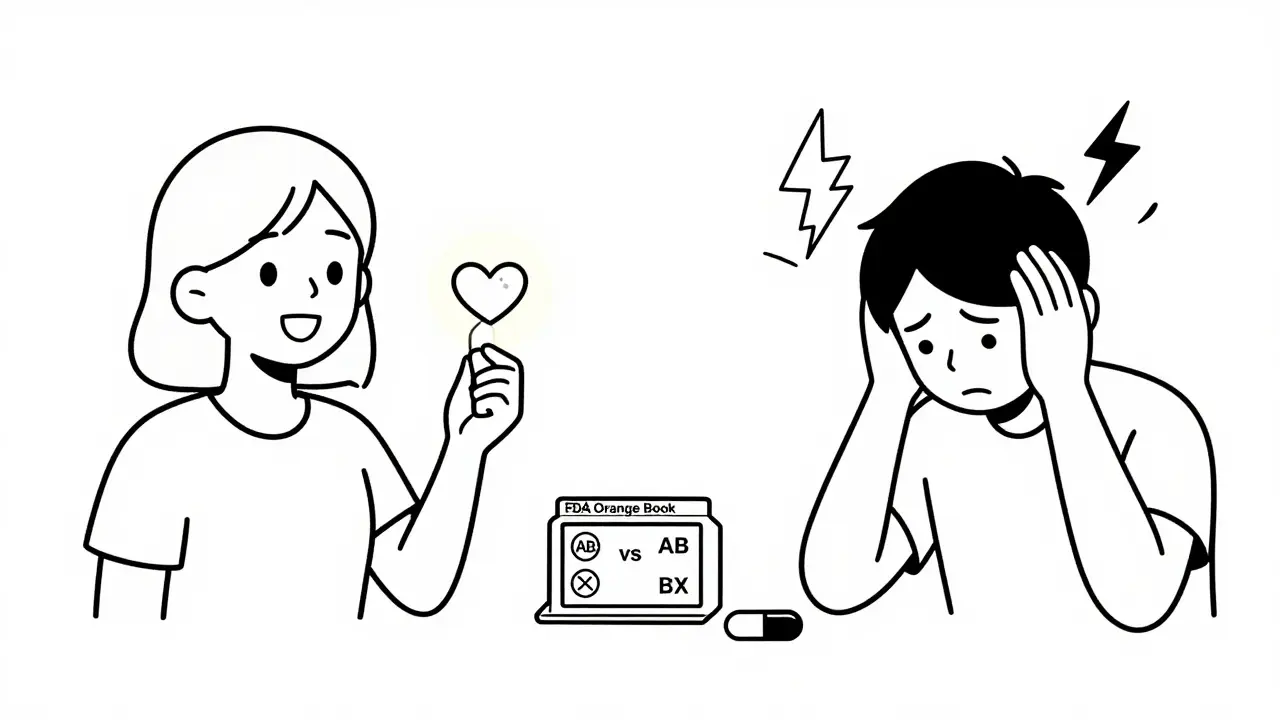
What Works in Practice
Providers who get the best results with generics follow a few clear patterns:- Check the Orange Book. Look for AB ratings. Avoid BX unless you’re sure.
- Know your high-risk drugs. Don’t substitute lamotrigine, warfarin, or tacrolimus without a conversation.
- Use EHR alerts. Many systems now flag narrow therapeutic index drugs - use them.
- Talk to patients. Explain why you’re switching - or why you’re not.
- Trust authorized generics. These are the brand-name drug sold under a generic label - same factory, same formula. Often the safest switch.
The Future: Smarter Substitutions
The FDA is now using real-world data - not just lab tests - to monitor generic performance. Their Sentinel Initiative tracks outcomes in millions of patients. Machine learning models are being trained to predict who’s likely to have issues with substitution based on age, comorbidities, and medication history. The Inflation Reduction Act of 2022 is pushing Medicare to favor generics even more. By 2025, generic use could rise another 5-7%. That’s good for the system - but only if providers are prepared. The bottom line? Generics aren’t the enemy. Poor communication and one-size-fits-all policies are. What works in one patient’s case might fail in another’s. The best providers don’t just prescribe - they listen, adapt, and protect.Are generic medications really as effective as brand-name drugs?
Yes - for most drugs. The FDA requires generics to prove bioequivalence, meaning they deliver the same active ingredient at the same rate and amount as the brand. Studies show no meaningful difference in outcomes for common medications like statins, blood pressure pills, or antidepressants. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or antiepileptics - some patients may respond differently to different formulations. That’s why providers often avoid automatic substitution in these cases.
Why do some patients have seizures after switching to generic lamotrigine?
While the active ingredient in generic and brand lamotrigine is identical, differences in inactive ingredients - like binders or coatings - can affect how the drug is absorbed in some people. In rare cases, this leads to lower blood levels, triggering breakthrough seizures in patients who were previously stable. Multiple case reports confirm this pattern. When patients are switched back to the brand, seizures typically stop. This is why neurologists recommend against automatic substitution for epilepsy meds without patient and provider consent.
What does an AB rating mean on the FDA’s Orange Book?
An AB rating means the generic drug is therapeutically equivalent to the brand-name reference drug. It has passed bioequivalence testing and is considered interchangeable. This is the gold standard for substitution. A BX rating means the FDA has identified potential issues - like inconsistent absorption - and does not consider it interchangeable. Always check the Orange Book before substituting, especially for high-risk drugs.
Should I always write “dispense as written” on prescriptions for generics?
No - only when necessary. For most medications like atorvastatin or metformin, substitution is safe and encouraged. Use “dispense as written” only for drugs with a narrow therapeutic index - such as warfarin, cyclosporine, or levothyroxine - or when a patient has had a bad reaction to a previous generic. Overusing this instruction can block cost savings and limit access. Be intentional, not automatic.
Why do some pharmacists say generics cause more side effects?
Some pharmacists believe this due to anecdotal reports or patient complaints - not science. The active ingredient is the same, so side effects should be identical. But patients often blame the generic when they notice a change in pill appearance, size, or color. This is a perception issue, not a safety issue. Good communication from pharmacists - explaining that the drug is the same, just made by a different company - reduces fear and improves outcomes.
Are authorized generics better than regular generics?
Authorized generics are made by the original brand-name manufacturer and sold under a generic label. They’re identical to the brand in every way - same factory, same formula, same inactive ingredients. Regular generics are made by other companies and may have different fillers or coatings. For patients sensitive to formulation changes - especially on narrow therapeutic index drugs - authorized generics are often the safest option. They offer the cost savings of generics without the variability risk.
How do state laws affect generic substitution?
State laws vary widely. In 19 states, pharmacists must substitute generics unless the prescriber says otherwise. In 7 states and D.C., patient consent is required before substitution. In 24 states, pharmacists aren’t protected from liability if a substitution causes harm. This patchwork creates confusion for providers and patients. Always know your state’s rules - and when in doubt, communicate clearly with your patients.

8 Comments
Joe Bartlett
December 17 2025
Generics are fine for most stuff, but warfarin? No thanks. I’ve seen people bleed out because some pharmacist thought ‘same drug’ meant ‘same effect.’
Anu radha
December 19 2025
My grandma switched to generic thyroid medicine and felt so tired. She cried when she went back to brand. It’s not about money-it’s about feeling okay.
Kaylee Esdale
December 21 2025
My doc told me generics are like different brands of toilet paper-same function, different texture. Some brands make you itch. Know your brand.
Jigar shah
December 21 2025
The FDA’s AB/BX classification system is critical but underutilized. Many prescribers and pharmacists are unaware of its existence, leading to unnecessary clinical instability. Standardized EHR integration of Orange Book data could mitigate this significantly.
Philippa Skiadopoulou
December 23 2025
Authorized generics are the quiet heroes of cost-effective therapy. Identical to brand, no formulation surprises, and still priced for the masses. Why aren’t they promoted more?
Brooks Beveridge
December 24 2025
Hey everyone-this is such a nuanced topic and you’re all saying the right things. I’ve worked with patients who swore their generic seizure med didn’t work, and when we switched back? Life changed. It’s not about distrust. It’s about listening. Every pill tells a story. Let’s not ignore it.
Nishant Desae
December 25 2025
You know what’s wild? I had this cousin in Mumbai who was on generic lamotrigine for 8 years and never had a hiccup. But then his sister in Ohio switched and had a seizure. Same drug, same dose, different body, different result. It’s not the generic’s fault-it’s the system. We treat meds like widgets but our bodies are living, breathing, weirdly unique snowflakes. Maybe we need to stop thinking in bulk and start thinking in individuals. Also, I think pharmacists should get a badge if they explain the pill color change. Like ‘I’m a Pill Whisperer’ or something. 😊
Chris Van Horn
December 26 2025
Let’s be honest-this entire debate is a distraction. The real issue is pharmaceutical monopolies and the FDA’s abysmal oversight of generic manufacturers. The 80–125% bioequivalence window is a joke. It’s a regulatory loophole that lets subpar manufacturers peddle dangerous variants under the guise of ‘cost savings.’ This isn’t medicine-it’s corporate roulette. And don’t get me started on the fact that 24 states allow substitution without consent. That’s not healthcare-it’s negligence dressed in a white coat.