Steroid Side Effect Risk Calculator
Personal Risk Assessment
Personalized Risk Report
Short-Term Side Effects Risk
Long-Term Side Effects Risk
When you’re prescribed prednisone or prednisolone, it’s usually because something in your body is raging out of control - maybe your immune system is attacking your joints, lungs, or skin. These drugs are powerful. They calm inflammation fast. But they come with a price. The side effects aren’t just possible - they’re common. And knowing what to expect can make all the difference between managing your treatment and being blindsided by it.
How Prednisone and Prednisolone Work - and Why They’re So Similar
Prednisone and prednisolone are both synthetic corticosteroids, designed to mimic the body’s natural stress hormone, cortisol. They suppress the immune system and shut down inflammation at the cellular level. That’s why they work so well for conditions like rheumatoid arthritis, lupus, severe asthma, and allergic reactions.
The key difference? Prednisone is a prodrug. Your liver has to convert it into prednisolone before it becomes active. If your liver is healthy, that conversion happens smoothly. But if you have cirrhosis, hepatitis, or other liver issues, that process slows down - sometimes by more than two-thirds. In those cases, doctors skip prednisone entirely and prescribe prednisolone directly. It’s faster, more reliable, and avoids the risk of underdosing.
For most people, though, 5 mg of prednisone equals 5 mg of prednisolone in effect. Neither is stronger. Neither is safer. The choice often comes down to liver function, availability, or what your doctor is used to prescribing.
Short-Term Side Effects: What Happens in Days or Weeks
If you’re on these drugs for a few days or weeks - say, for a flare-up of asthma or a bad allergic reaction - you’re likely to notice some immediate changes. These aren’t rare. They’re expected. And they usually fade once you stop taking the medication.
- Insomnia: Nearly 7 out of 10 people report trouble sleeping. Steroids spike cortisol levels, which disrupts your natural sleep rhythm. Taking your dose before 2 p.m. cuts sleep problems by more than half.
- Increased appetite and weight gain: You might feel hungry all the time. This isn’t just cravings - it’s your brain being rewired by the drug. Many gain 5-10 pounds in the first two weeks, mostly from fluid retention and increased calorie intake.
- Mood swings: Some people feel euphoric. Others get irritable, anxious, or even depressed. A small percentage develop steroid psychosis - intense paranoia, hallucinations, or irrational fear. One Reddit user described calling 911 because he thought spiders were crawling on his walls. That’s real. It happens at doses above 40 mg daily.
- Fluid retention and swelling: Your face might puff up (called "moon face"), your ankles swell, and your clothes feel tighter. This is from sodium retention and water buildup. It’s temporary, but it’s also one of the most distressing side effects for parents of kids on these drugs.
- Headaches and dizziness: Blood pressure can rise. Vertigo is common. If you feel lightheaded, don’t ignore it.
These effects aren’t signs you’re doing something wrong. They’re signs the drug is working - and hitting your body harder than you expected. Most people find these symptoms ease up within a week or two after stopping the medication.
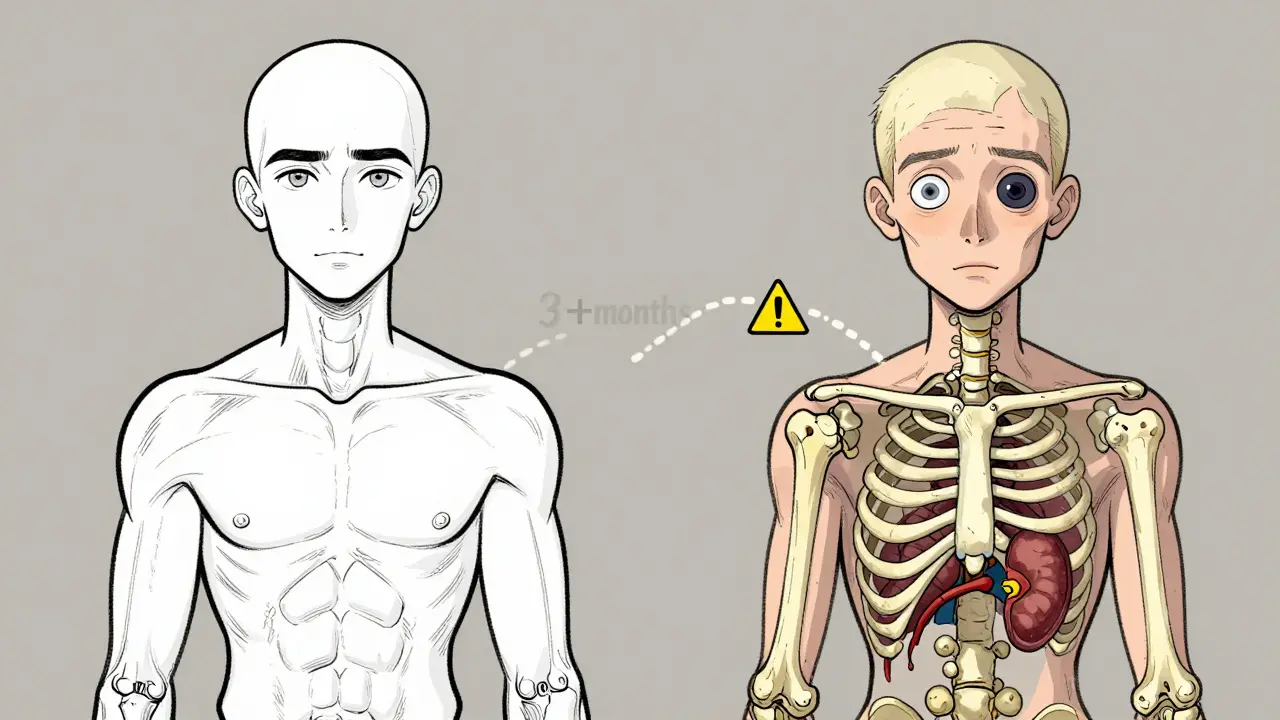
Long-Term Side Effects: The Hidden Costs of Months or Years
When you take prednisone or prednisolone for more than three months, the risks shift. The short-term annoyances fade. The real dangers begin to show up - and they can be permanent.
- Osteoporosis and bone fractures: After two years of use, more than 6 in 10 long-term users develop weakened bones. Steroids block bone formation and speed up bone loss. Even young people aren’t safe. Bone density scans are recommended if you’re on more than 5 mg daily for over three months.
- Cataracts and glaucoma: Your eyes are vulnerable. Up to 40% of people on long-term steroids develop cataracts. Glaucoma risk rises too. Regular eye exams aren’t optional - they’re lifesaving.
- Diabetes or worsening blood sugar: Steroids make your liver pump out more glucose and block insulin. About 54% of non-diabetics on doses above 20 mg daily develop high blood sugar. If you’re prediabetic, this can push you into full-blown diabetes.
- Adrenal insufficiency: Your body stops making its own cortisol because the drug is doing the job. If you stop suddenly, your body can’t catch up. That’s an adrenal crisis - low blood pressure, vomiting, confusion, even death. Tapering off slowly over weeks is non-negotiable.
- Muscle weakness and wasting: You might feel like you can’t climb stairs or lift your arms. Steroids break down muscle protein. This gets worse the longer you’re on them.
- Skin thinning and easy bruising: Your skin becomes paper-thin. A bump or scratch can leave a lasting mark. Wounds heal slowly. Infections take longer to clear.
- Peptic ulcers and pancreatitis: Steroids increase stomach acid and reduce the protective lining. That’s why doctors routinely prescribe proton pump inhibitors (like omeprazole) if you’re on more than 5 mg daily for over four weeks. Without it, ulcer risk jumps from 1% to over 8%.
These aren’t theoretical risks. The Autoimmune Registry tracked 1,204 long-term users. 63% developed osteoporosis. 41% needed cataract surgery. 37% ended up with permanent adrenal damage requiring lifelong hormone replacement.
Who’s Most at Risk - and What You Can Do About It
Not everyone gets hit the same way. Certain groups face higher risks:
- Children: Growth slows by 1.2 cm per year for every 0.2 mg/kg/day of prednisolone. Height checks every three months are standard for kids on long-term therapy.
- Older adults: Bone loss and muscle wasting happen faster. Falls become more dangerous.
- People with diabetes or high blood pressure: Steroids make both worse. Close monitoring is essential.
- People with liver disease: Prednisone may not convert properly. Prednisolone is safer.
There are ways to fight back:
- Take the lowest dose possible: The risk of serious side effects jumps sharply above 7.5 mg daily for more than three weeks. If you’re on 20 mg, ask if you can drop to 10 mg.
- Take it early in the day: Before 2 p.m. to avoid insomnia and cortisol disruption.
- Protect your bones: Get a DEXA scan. Take calcium and vitamin D. Do weight-bearing exercise - walking, lifting weights. Studies show this preserves 22% more bone density.
- Watch your diet: Limit sodium to under 2,000 mg a day. Eat potassium-rich foods like bananas, spinach, and sweet potatoes to fight fluid retention and low potassium.
- Use a pill tracker: Missing a dose can trigger adrenal crisis. Doubling a dose can cause toxicity. Apps that remind you to take your pill and log your symptoms improve adherence by 37%.
When to Call Your Doctor - Red Flags You Can’t Ignore
Not every side effect needs panic. But some do.
Call your doctor immediately if you experience:
- Sudden, severe headache or vision changes (possible glaucoma or stroke)
- Extreme mood swings, hallucinations, or thoughts of self-harm
- Swelling in your legs, chest pain, or trouble breathing (heart failure or fluid overload)
- Unexplained fever, chills, or sore throat (signs your immune system is too suppressed)
- Severe abdominal pain (possible pancreatitis)
- Signs of adrenal crisis: nausea, vomiting, dizziness, low blood pressure, confusion
And never, ever stop these drugs cold. Even if you feel fine. Tapering is mandatory. Your doctor should give you a clear plan before you start.

The Bigger Picture: Are They Worth It?
These drugs are dangerous. But they’re also lifesaving.
In giant cell arteritis, prednisone improves symptoms in 92% of patients - compared to 58% with placebo. In severe lupus flare-ups, they prevent kidney failure. In asthma attacks, they stop hospitalizations.
A 2023 survey of 500 rheumatologists found 94% still consider prednisone and prednisolone indispensable. Why? Because nothing else works as fast or as well for acute inflammation.
The key isn’t avoiding them. It’s using them wisely. Short-term, with clear goals. Long-term, only if absolutely necessary. And always, always with monitoring.
These aren’t pills you take and forget. They’re tools. And like any tool, they’re powerful when used correctly - and dangerous when misused.
Can prednisone and prednisolone be used interchangeably?
Yes, at equal doses - 5 mg prednisone equals 5 mg prednisolone - if your liver is healthy. But if you have liver disease, prednisone won’t convert properly, and you’ll need prednisolone directly. Your doctor will choose based on your liver function, not preference.
How long do side effects last after stopping?
Short-term effects like insomnia, appetite changes, and mood swings usually fade within 1-2 weeks after stopping. Fluid retention and weight gain drop quickly too. But long-term damage - like osteoporosis, cataracts, or adrenal insufficiency - can be permanent. That’s why tapering and monitoring matter.
Is there a safer alternative to prednisone?
For long-term use, yes - biologics like tocilizumab or rituximab can replace steroids in conditions like rheumatoid arthritis, cutting steroid dependence by nearly a third. But for acute flare-ups - sudden asthma attacks, severe allergic reactions, or autoimmune crises - nothing matches the speed and power of prednisone or prednisolone. They’re still the first-line defense.
Can I take prednisone if I have diabetes?
Yes - but with extreme caution. Steroids raise blood sugar significantly. If you’re diabetic, your doses may need adjustment. If you’re not diabetic but on more than 20 mg daily, you’re at high risk of developing steroid-induced diabetes. Blood sugar monitoring is required.
Why do I need to take prednisone with food?
Taking it with food reduces stomach irritation and lowers the risk of ulcers. It’s also a good habit to avoid nausea. But more importantly, if you’re on long-term therapy, your doctor will likely prescribe a proton pump inhibitor (PPI) like omeprazole to protect your stomach lining - especially if you’re on more than 5 mg daily for over four weeks.
Is it safe to drink alcohol while on prednisone?
It’s not recommended. Alcohol increases your risk of stomach ulcers, liver damage, and high blood pressure - all of which are already heightened by prednisone. It can also worsen mood swings and sleep problems. If you drink, limit it heavily - and talk to your doctor.
What Comes Next?
If you’re starting prednisone or prednisolone, treat it like a mission - not just a prescription. Track your symptoms. Know your numbers - blood pressure, blood sugar, weight. Stick to your taper plan. Ask questions. Don’t assume side effects are normal just because everyone gets them.
These drugs save lives. But they also change them. The goal isn’t to avoid them - it’s to use them with your eyes wide open. Because when you understand the risks, you’re not just taking a pill. You’re making a smart, informed choice.

12 Comments
Alvin Bregman
January 13 2026
Man i took this stuff for a bad flare up last year and woke up looking like a balloon animal
Anna Hunger
January 14 2026
Thank you for this comprehensive breakdown. As a healthcare provider, I see too many patients unaware of the long-term risks. This should be mandatory reading for anyone prescribed corticosteroids beyond a two-week course.
Jason Yan
January 14 2026
It’s wild how something so effective can also be so cruel to the body. I think we need to reframe how we talk about these drugs-not as ‘miracle pills’ but as high-stakes tools. Like using a chainsaw to trim a hedge. It works, but you better know what you’re doing, wear the gear, and have an exit plan.
I’ve seen friends lose their vision, their bones, their sense of self to this stuff. And the worst part? No one warns you until it’s too late. Doctors say ‘it’s temporary’ like that’s enough. But temporary doesn’t mean harmless.
And the tapering… people think they can just quit because they ‘feel fine.’ That’s like unplugging a nuclear reactor because the lights are back on. The reactor’s still hot. Your adrenal glands are still asleep.
I wish there was a standard pamphlet handed out with the script. Not just ‘take with food’ but ‘your body will forget how to be itself.’
It’s not just medical-it’s existential. You’re borrowing your own biology and the interest is brutal.
That said, I’m grateful it exists. I’ve watched people go from wheelchair to walking because of it. But gratitude shouldn’t blind us to the cost.
Maybe the real question isn’t ‘should I take it?’ but ‘what am I willing to lose to keep living?’
says haze
January 16 2026
Interesting how the medical establishment treats these drugs as neutral instruments when they’re essentially chemical coercion. The body doesn’t ‘adapt’-it’s hijacked. Cortisol isn’t a switch you flip; it’s a symphony, and prednisone doesn’t conduct-it obliterates the orchestra.
And yet, we glorify the ‘miracle drug’ narrative while ignoring the collateral damage. It’s capitalism in pill form: fix the symptom, ignore the system. The patient becomes a data point in a clinical trial, not a human being learning to live with a body that no longer belongs to them.
They call it ‘tapering’ like it’s a gentle descent. It’s not. It’s withdrawal from a chemical identity crisis.
And let’s not pretend the ‘liver conversion’ distinction is just technical-it’s a class issue. Prednisolone costs more. Your access to safer care depends on your insurance tier.
It’s not medicine. It’s survival theater.
Henry Sy
January 17 2026
Y’all act like prednisone’s some devil drug but honestly? It’s the only thing that kept me alive during my lupus flare. I gained 20 lbs, looked like a cartoon, couldn’t sleep, and my mood swung like a pendulum in a hurricane. But I could breathe again. I could walk again. I didn’t die.
Yeah, the side effects suck. But so does dying. So does watching your kidneys fail. So does watching your kid’s face swell up because you couldn’t stop the inflammation.
Don’t demonize the tool because the fight is ugly. The enemy isn’t the pill. The enemy is the disease that makes you choose between your body and your life.
I’d take moon face every day if it meant I could still hug my daughter without wheezing.
Sarah Triphahn
January 17 2026
Anyone else notice how no one talks about the emotional manipulation? You’re told you’re ‘lucky’ to be on this drug. But you’re also made to feel guilty when you complain. Like your suffering is the price of being ‘strong.’
I cried every night for three weeks because I didn’t recognize myself. My husband said I was ‘overreacting.’ Guess what? I was on 60mg. That’s not ‘mood swings.’ That’s neurochemical warfare.
And don’t get me started on how doctors dismiss psychosis as ‘stress.’ No. It’s pharmacological psychosis. It’s real. It’s terrifying. And it’s not rare.
Vicky Zhang
January 17 2026
To anyone starting this: you’re not weak for struggling. You’re not lazy for gaining weight. You’re not crazy for feeling like you’re losing your mind.
This drug is a beast. It doesn’t care if you’re ‘strong.’ It doesn’t care if you ‘should be grateful.’ It just does its job-by breaking you down to rebuild you.
Drink water. Walk every day. Eat bananas. Take your calcium. Write down every mood swing. Tell someone-anyone-when you feel like you’re falling apart.
You’re not alone. And you’re not broken. You’re just fighting a war inside your body. And you’re still standing. That’s courage.
Andrew Freeman
January 18 2026
Most of this is hype. I’ve been on prednisone for 5 years at 5mg and I’m fine. No cataracts, no diabetes, no osteoporosis. My doctor says I’m lucky. Maybe it’s genetics. Maybe it’s not that bad. Stop scaring people.
shiv singh
January 19 2026
They don’t want you to know the truth. Prednisone is a government tool to control the masses. The side effects are exaggerated to make you fear it. But the real reason they push it? To keep you dependent. Think about it. Who profits? Pharma. Who gets sick? You. Coincidence? I think not.
And why do they say ‘taper’? Because they need you to keep coming back. The system is rigged. Your body was never meant to be chemically manipulated like this.
Go natural. Turmeric. Ginger. Cold showers. You don’t need their poison.
Sarah -Jane Vincent
January 21 2026
Anyone else notice that the FDA never approved prednisone for long-term use? It’s off-label! That’s why they don’t warn you enough. It’s illegal to prescribe it like this. Someone should sue. And why do they even make prednisolone if they’re just going to lie about equivalence? It’s all a scam.
I did my own research. The liver conversion myth is propaganda. They just want you to buy the more expensive version. I’ve been taking prednisone for 8 years with no issues. I’m 32. My bones are fine. My eyes are fine. My liver? Perfect. They’re just trying to sell you fear.
Robert Way
January 21 2026
so i took this stuff for my eczema and i swear i started seeing things like tiny people living in my walls and i called 911 and they came and i was like ‘they’re crawling’ and the paramedic just looked at me and said ‘you on steroids?’ and i said yes and he said ‘oh cool’ and left
so yeah
Dylan Livingston
January 22 2026
How touching. A well-researched, clinically accurate, and deeply human account of a drug that’s been saving lives for decades-only to be met with the same old performative outrage and virtue signaling from people who’ve never actually had to choose between breathing and breaking.
You all treat prednisone like a villain in a Netflix documentary, but let’s be honest: if you’re the one lying in the ER gasping for air while your lungs collapse, you won’t care about moon face. You’ll be begging for the next pill.
It’s not about ‘fear-mongering.’ It’s about responsibility. And the fact that you’d rather rant about ‘pharma conspiracies’ than help someone understand the real trade-offs? That’s the real tragedy.
For every comment here that says ‘I’m fine,’ there’s someone else in the dark, tapering alone, scared to tell their doctor they’re hallucinating because they think they’ll be labeled ‘crazy.’
This isn’t about being ‘too sensitive.’ It’s about being human.