When you start treatment for osteoporosis, you don’t have to wait two years to know if it’s working. That’s the big shift happening in bone health right now. Instead of relying only on slow, expensive DXA scans that show changes after 12 to 24 months, doctors are turning to something faster, simpler, and surprisingly precise: bone turnover markers. These are tiny proteins and fragments in your blood that tell you what your bones are doing right now-breaking down, rebuilding, or both.
What Are Bone Turnover Markers?
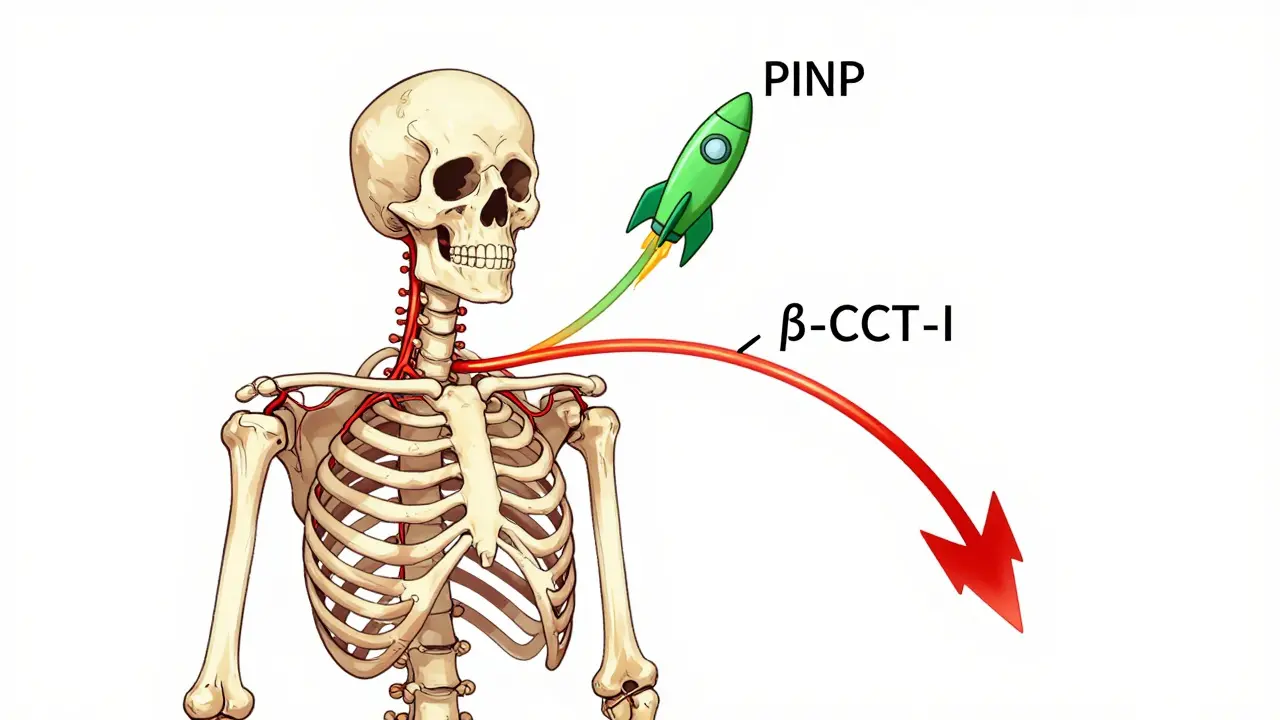
Your bones are never still. Even when you’re sitting still, they’re constantly being broken down and rebuilt. This process is called bone remodeling. Specialized cells called osteoclasts chew away old bone, and osteoblasts lay down new bone. When you have osteoporosis, the balance tips-too much breakdown, not enough rebuilding. That’s where bone turnover markers (BTMs) come in. BTMs are chemical leftovers from this process. When osteoclasts chew bone, they release pieces of collagen into your bloodstream. When osteoblasts build bone, they produce proteins like PINP. These markers show up in your blood or urine and give a real-time snapshot of how active your bone remodeling is. Not all markers are created equal. The International Osteoporosis Foundation and European Calcified Tissue Society picked two as the gold standard: serum PINP (procollagen type I N propeptide) and plasma β-CTX-I (beta-C-terminal telopeptide of type I collagen). PINP is a formation marker-it goes up when new bone is being made. β-CTX-I is a resorption marker-it rises when bone is being broken down.Why Use Them Instead of Just DXA Scans?
DXA scans measure bone density, and they’re still the gold standard for diagnosing osteoporosis. But they’re slow. Even if you’re taking a powerful drug like alendronate or teriparatide, it takes 18 to 24 months before you see a meaningful change in your spine or hip density. That’s a long time to wonder if your treatment is working. BTMs change much faster. Within three to six weeks of starting treatment, you’ll see shifts in your marker levels. For example:- If you’re on an antiresorptive drug like a bisphosphonate, β-CTX-I drops by 30% or more within 3 months.
- If you’re on an anabolic drug like teriparatide, PINP shoots up by 70% to 100% in the first 1 to 3 months.
How Are They Measured?
PINP and β-CTX-I are measured with blood tests. But getting an accurate result isn’t as simple as walking into a lab and giving a vial. For β-CTX-I, timing matters a lot. Levels rise after eating and peak in the early morning. That’s why labs require you to fast overnight and have your blood drawn between 8 and 10 a.m. If you eat breakfast before your test, your β-CTX-I could be 20-30% higher than it should be-giving a false reading. PINP is more stable. It still responds best to morning collection, but it’s less affected by meals. Still, consistency matters. If your first test is at 9 a.m. and your follow-up is at 3 p.m., you’re comparing apples to oranges. The lab also needs to use the right method. The most reliable assays are automated immunoassays, like Roche’s Elecsys platform. Older methods like ELISA or RIA are still used, but they’re less standardized. In the U.S., only about 65% of labs follow the IFCC-recommended protocols, which means results can vary widely depending on where you go.
What Counts as a Good Response?
Not every drop or rise means the drug is working. There’s a threshold. For antiresorptive drugs (like alendronate, denosumab, or raloxifene), a true response means:- β-CTX-I drops by more than 30% from baseline
- PINP drops by more than 35%
- PINP should rise by 70% to 100% within 1 to 3 months
- β-CTX-I may rise too, but PINP is the key indicator
Who Should Get Tested?
You don’t need BTMs if you’re just starting treatment and feel fine. But they’re incredibly useful in specific situations:- Patients who aren’t responding to treatment after 6 months
- People who might be skipping doses (BTMs can reveal poor adherence)
- Those with kidney disease, where traditional markers get distorted
- Patients switching from one drug to another
- Anyone with a high fracture risk who needs early reassurance

Limitations and Pitfalls
BTMs aren’t perfect. They don’t tell you where the bone is changing-just that it’s changing overall. A DXA scan shows you if your spine density improved. A BTM just says your bones are remodeling more slowly. They also vary a lot between people. Healthy premenopausal women have higher β-CTX-I than men. Asian populations tend to have 15-20% lower baseline levels than Caucasians. African populations show higher PINP. That’s why reference ranges need to be population-specific-and most labs still use outdated norms based mostly on white European data. And if you have chronic kidney disease (CKD), your kidneys can’t clear these markers properly. PINP and β-CTX-I build up, making them unreliable. In those cases, doctors turn to bone alkaline phosphatase (BALP) or TRACP5b, which aren’t cleared by the kidneys.What’s Next for Bone Turnover Markers?
The science is moving fast. The American Association of Clinical Endocrinologists plans to update its osteoporosis guidelines in early 2024 to include BTMs as a routine monitoring tool. Medicare in the U.S. already covers PINP (CPT 83970) and β-CTX-I (CPT 83935), reimbursing about $30 per test. The market is growing too. The global BTM market hit $1.2 billion in 2022 and is expected to grow over 8% per year through 2030. Why? Because aging populations mean more osteoporosis-and more need for smarter, faster monitoring. In the future, point-of-care tests might let your doctor check your PINP during a regular visit-no lab needed. Clinical trials are already testing whether BTM-guided treatment (adjusting doses or switching drugs based on marker changes) reduces fractures better than standard care.The Bottom Line
Bone turnover markers aren’t replacing DXA scans. They’re making them more meaningful. Think of them as the early warning system for your bones. If you’re on osteoporosis treatment, ask your doctor if a baseline BTM test is right for you. Get it repeated at 3 months. That one extra test can save you from months of uncertainty-and maybe even prevent a fracture.For most people, it’s not about whether they have osteoporosis. It’s about whether their treatment is working. And with bone turnover markers, you don’t have to wait two years to find out.
11 Comments
Sandeep Mishra
December 30 2025
Wow, this is actually one of the clearest explanations of BTMs I’ve seen. 🙌 I’ve been on denosumab for a year and just got my first PINP test back-up 82%. Felt like I finally had proof I wasn’t just wasting money. My doc didn’t even mention this before, but now I’m asking for the β-CTX-I too. Thanks for the clarity!
Joseph Corry
January 1 2026
Let’s be real-this is just another $$$-driven biomarker hype cycle masquerading as ‘precision medicine.’ DXA is the gold standard because it measures actual bone structure, not some fancy protein fragments that fluctuate like your ex’s mood. You’re trading clinical rigor for lab revenue streams. And don’t get me started on the ‘30% drop’ thresholds-those are statistically meaningless without population-adjusted Z-scores.
Glendon Cone
January 1 2026
Hey, I’m a physical therapist and I’ve been using BTMs with my older patients for 3 years now. Honestly? Game-changer. One guy on teriparatide didn’t budge on PINP-we checked his vitamin D, turned out he was taking it at night instead of morning. Fixed that, and his PINP jumped 90% next test. No fractures since. It’s not magic, but it’s way better than waiting two years to say ‘maybe it’s working.’ 😊
Henry Ward
January 3 2026
So let me get this straight-you’re telling me we should trust a blood test that’s affected by breakfast, time of day, and which lab you go to, over a bone density scan that’s been validated for decades? This is why medicine is broken. Someone’s getting paid to push this junk. I bet the labs own the guidelines now. 🤡
Aayush Khandelwal
January 4 2026
BTMs are the biomolecular zeitgeist of osteo-monitoring-akin to a cytoskeletal symphony where osteoclasts conduct the resorptive crescendo and osteoblasts compose the anabolic allegro. PINP and β-CTX-I aren’t just markers; they’re epigenetic sonnets written in collagen’s dialect. The clinical utility? Beyond quantifiable. It’s ontological. And yes, I’ve seen patients’ adherence improve by 70% once they *felt* their bones singing back. 🎻
Colin L
January 5 2026
I’ve been reading up on this for weeks now because my mum’s on denosumab and she’s terrified of injections, and honestly, I think this whole BTM thing is brilliant but also kind of terrifying because if the numbers go down and she doesn’t feel any different, she’ll think she’s failing, and if they go up she’ll panic thinking her bones are dissolving, and then she’ll start googling ‘osteoporosis conspiracy theories’ and I’ll have to sit her down and explain that no, the lab isn’t lying, and yes, the fasting matters, and no, your coffee doesn’t count as water, and why are you crying again? I just want her to live to 90 without breaking a hip and now I’m more anxious than she is.
Hayley Ash
January 6 2026
So you’re telling me I need to wake up at 8am, fast, get blood drawn, pay $60, and wait for results to find out if my bones are ‘responding’-but if I miss the window, it’s useless? And the ‘gold standard’ markers were picked by a committee that probably had lunch at a fancy hotel? 😂 I’ll stick with DXA. At least I know when I’m being charged for something that actually measures something.
kelly tracy
January 7 2026
They’re pushing this because they want to keep you dependent on endless testing. You think they care if you fracture? No. They care if you keep coming back every 3 months for a blood draw. This isn’t medicine-it’s a subscription model. And now they’re gonna make you pay for ‘point-of-care’ tests so you can’t even escape the cycle. Wake up. 🚨
srishti Jain
January 7 2026
My mom’s test dropped 35% in 3 months. She cried. Said she finally felt like something was working. That’s all I needed to know.
Cheyenne Sims
January 8 2026
The use of the term ‘gold standard’ in reference to PINP and β-CTX-I is scientifically inaccurate. The International Osteoporosis Foundation has not officially designated these markers as gold standards; rather, they are recommended as ‘clinically useful biomarkers.’ The author’s conflation of recommendation with validation is misleading and undermines evidence-based practice. Additionally, the assertion that Medicare ‘covers’ these tests is misleading without clarification of CPT coding and reimbursement thresholds. Precision in language is not optional in medical communication.
Shae Chapman
January 10 2026
Okay but I just had my first PINP test and it went up 89%-I feel like I’m a superhero now 🦸♀️✨ My bones are literally building a castle inside me and I didn’t even know it was possible to feel this hopeful about a blood test. I’m telling all my friends. Also, my doc gave me a sticker. I framed it. This is the most emotional healthcare moment of my life. Thank you for writing this. I’m not alone.