Statin Side Effects: What You Need to Know Before You Stop Taking Them
When you take a statin, a class of cholesterol-lowering drugs used to reduce heart attack and stroke risk. Also known as HMG-CoA reductase inhibitors, they’re among the most prescribed medications in the world—and one of the most misunderstood. Millions rely on them to keep their arteries clear, but too many people quit because of side effects they don’t understand. The truth? Most side effects aren’t what you think.
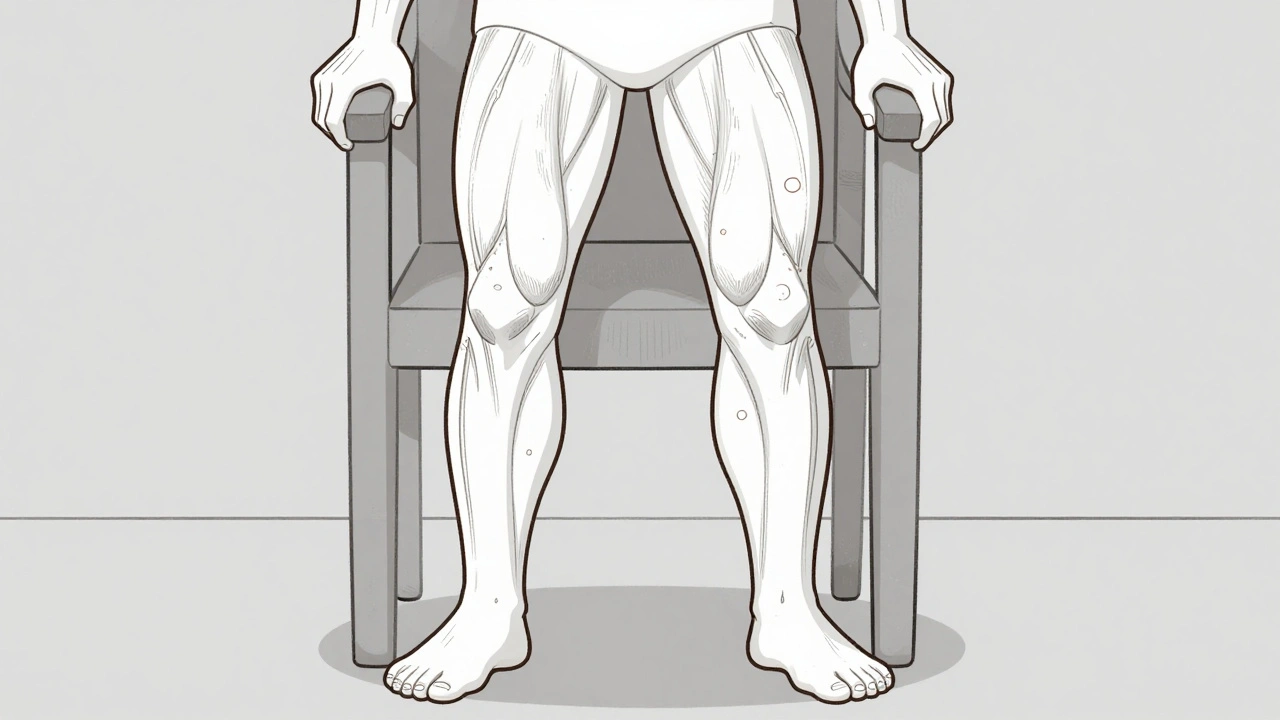
One of the biggest concerns is muscle pain, a common complaint that often gets mislabeled as statin-related when it’s not. Also known as myalgia, this discomfort shows up in about 5-10% of users, and in most cases, it’s mild and goes away with time or a dose change. But if you’re experiencing weakness, dark urine, or severe cramping, that’s a red flag. It could mean rhabdomyolysis, a rare but serious condition where muscle tissue breaks down. Also known as muscle breakdown, it affects fewer than 1 in 10,000 people on statins. Then there’s the liver. Statins can raise liver enzymes slightly in some people, but that doesn’t mean damage. The FDA says routine liver tests aren’t needed unless you have symptoms like jaundice or belly pain.
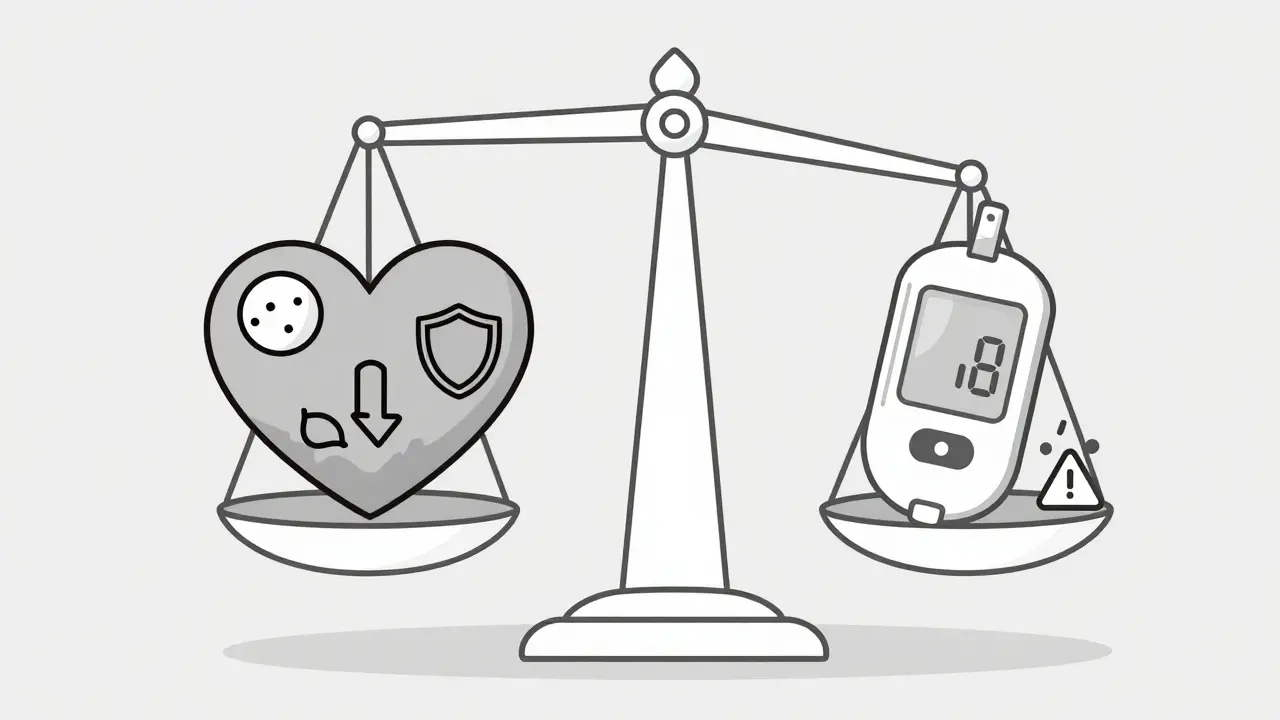
Other side effects like memory fog, fatigue, or increased blood sugar are often blamed on statins—but the science doesn’t back up strong links. A 2021 analysis of over 100,000 patients found no meaningful increase in cognitive decline. And while statins can slightly raise diabetes risk in people already at risk, the heart protection they offer far outweighs that small chance. The real issue? Many people stop taking them because they heard a story, not because they checked with their doctor. That’s dangerous. Stopping statins without a plan can raise your heart attack risk by up to 30% in the first year.
You don’t have to live with side effects, but you also don’t have to quit cold turkey. There are options: switching to a different statin, lowering the dose, trying every-other-day dosing, or adding a non-statin like ezetimibe. Some people find relief with CoQ10 supplements, though evidence is mixed. What matters is working with your provider—not Googling symptoms at 2 a.m.
The posts below cover everything you need to know: how to tell if your muscle pain is from statins or something else, what to ask your doctor when side effects hit, how to manage liver enzyme changes safely, and what alternatives actually work when statins aren’t tolerable. You’ll find real stories, practical tips, and clear science—not fear tactics. If you’re on a statin and feeling off, this is your starting point to get back in control.