Statins Diabetes Risk Calculator
Risk Assessment
Enter your health information to estimate your risk of developing diabetes while taking statins.
Many people take statins to lower cholesterol and protect their heart. But for some, these lifesaving drugs come with an unexpected side effect: higher blood sugar. It’s not a myth. It’s not rare. And it’s not something you should panic about - but you should know about it.
Statins Help Your Heart, But They Can Push Blood Sugar Up
Statins like atorvastatin, rosuvastatin, and simvastatin are among the most prescribed drugs in the world. Over 35 million Americans use them. They cut LDL (bad) cholesterol by 30% to 60%, reduce heart attacks, and lower stroke risk. That’s huge. But between 2010 and now, study after study has shown a small but consistent link: statins can raise blood sugar levels enough to push some people into diabetes.
This isn’t about everyone. It’s about people who are already at risk - those with prediabetes, obesity, high blood pressure, or a family history of type 2 diabetes. For them, statins can be the final nudge that crosses the line from normal to diabetic. Research from the Oxford Population Health team found that statins increase the chance of developing diabetes by 10% with low doses and up to 36% with high doses. That sounds scary - until you compare it to the benefit.
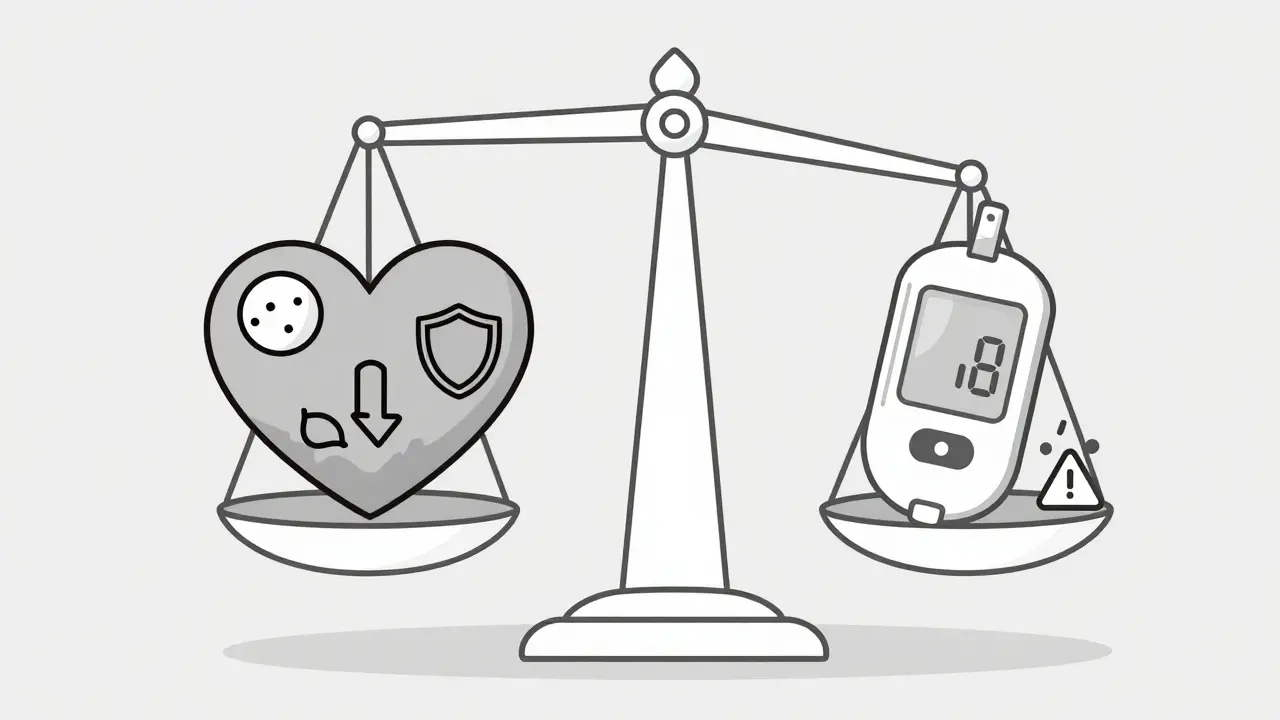
For every 100 people taking a high-intensity statin for five years, about 1.5 fewer will have a heart attack or stroke. Meanwhile, about 0.2 to 0.3 new cases of diabetes might appear. That’s 50,000 heart events prevented annually in the U.S. versus 2,000 to 3,000 extra diabetes cases. The math still favors statins.
How Do Statins Raise Blood Sugar?
It’s not just one thing. Statins mess with your body’s insulin system in multiple ways.
First, they make your muscles and fat cells less responsive to insulin - a condition called insulin resistance. A 2023 study tracking nearly 9,000 people found that those on statins had a 24% drop in insulin sensitivity. That means your body needs more insulin to do the same job.
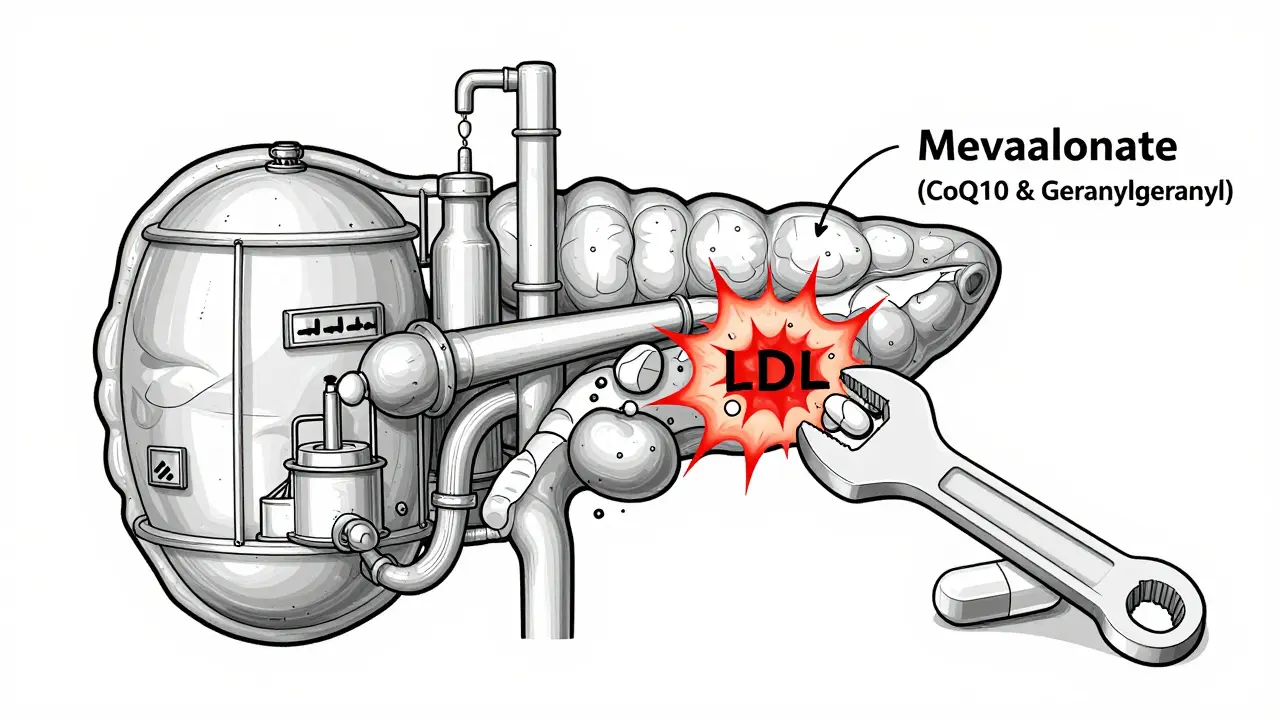
Second, statins reduce insulin production. Your pancreas has beta cells that release insulin when blood sugar rises. But statins interfere with a key metabolic pathway called the mevalonate pathway. This cuts down on molecules like CoQ10 and geranylgeranyl pyrophosphate that beta cells need to function properly. One study showed insulin secretion dropped by 12% in statin users.
Third, statins increase LDL cholesterol uptake in pancreatic cells. That sounds backwards - you take statins to lower LDL, but in the pancreas, it’s the opposite. Excess LDL builds up in beta cells, triggering inflammation and making them less efficient at releasing insulin.
And here’s the twist: your body tries to compensate. When insulin resistance goes up, your pancreas works harder and pumps out more insulin - at least at first. But over time, the cells burn out. That’s when blood sugar climbs past the diabetes threshold.
Not All Statins Are the Same
Some statins are more likely to raise blood sugar than others. High-intensity statins - like atorvastatin (40-80 mg) and rosuvastatin (20-40 mg) - carry the highest risk. Moderate-intensity ones like pravastatin or fluvastatin have much lower or even negligible effects.
A 2023 review in the Cleveland Clinic Journal of Medicine found that atorvastatin had the strongest association with rising HbA1c levels in people with existing diabetes. If you’re already diabetic, switching from atorvastatin to pravastatin might help stabilize your numbers.
But here’s the catch: if you have very high cholesterol or a history of heart attack, your doctor might still recommend the stronger statin. The goal isn’t to avoid statins - it’s to pick the right one for your profile.
Who’s Most at Risk?
If you’re wondering whether you’re in the danger zone, look at these factors:
- Prediabetes (fasting glucose 100-125 mg/dL or HbA1c 5.7-6.4%)
- Body mass index (BMI) over 30
- Waist circumference over 40 inches for men or 35 inches for women
- High triglycerides or low HDL
- High blood pressure
- History of gestational diabetes
- Family history of type 2 diabetes
- Being over age 65
People with these traits are more likely to see their blood sugar rise on statins. But even among high-risk individuals, not everyone develops diabetes. Genetics play a role too. A 2023 study in Nature Medicine found that people with certain variants in the SLCO1B1 gene are more sensitive to statin-induced glucose changes. We’re not testing for this routinely yet - but we will be soon.
What Should You Do?
Don’t stop your statin. That’s the most important thing. The risk of heart attack or stroke is far greater than the risk of developing diabetes.
But do this:
- Get your fasting blood sugar and HbA1c checked before starting a statin - and again at 3 and 6 months after starting.
- If you’re already diabetic, monitor your levels more closely. Some people need to adjust their diabetes meds after starting statins.
- Ask your doctor if a lower-intensity statin could work for you - especially if you’re at high diabetes risk.
- Focus on lifestyle. Losing 5-10% of your body weight, walking 150 minutes a week, and cutting added sugar can reduce your diabetes risk by over 50%. These changes also make statins work better.
- Don’t take supplements like CoQ10 hoping to block the side effect. There’s no solid proof they help with blood sugar.
Some patients report their blood sugar improves after stopping statins. But again - don’t quit without talking to your doctor. The cardiovascular protection doesn’t vanish overnight.
What Experts Say
The American Heart Association, the American Diabetes Association, and the CDC all agree: don’t avoid statins because of diabetes risk. The benefits win.
Dr. Steven Nissen from Cleveland Clinic puts it plainly: "The risk is real, but it’s small and manageable. The alternative - not taking a statin when you need one - is far worse."
The FDA has required statin labels to include a warning about blood sugar increases since 2012. But most patients never see it. That’s why this information matters.
What’s Next?
Scientists are working on ways to make statins safer. One idea: develop new cholesterol drugs that work like statins but don’t block the mevalonate pathway. Another: use genetic testing to match patients with the statin least likely to affect their blood sugar.
For now, the message is simple: if you need a statin, take it. But get your blood sugar checked. Stay active. Eat well. And talk to your doctor. You’re not choosing between heart health and diabetes prevention - you’re managing both.
Do statins cause diabetes?
Statins don’t cause diabetes in most people. But they can raise blood sugar enough to push some at-risk individuals over the diagnostic threshold. This happens in about 0.1-0.3% of users per year. The risk is higher with high-dose statins and in people with prediabetes, obesity, or metabolic syndrome.
Which statin is least likely to raise blood sugar?
Pravastatin and fluvastatin have the lowest association with increased blood sugar. Atorvastatin and rosuvastatin - especially at high doses - carry the highest risk. If you’re at risk for diabetes, your doctor may choose a lower-risk statin, but only if it still lowers your cholesterol enough to protect your heart.
Should I stop taking statins if my blood sugar goes up?
No. Stopping statins increases your risk of heart attack and stroke far more than the risk of developing diabetes. Instead, work with your doctor to adjust your diabetes treatment, switch to a different statin, or improve lifestyle habits. Most people can manage both conditions safely.
Can lifestyle changes reduce the risk of statin-induced diabetes?
Yes. Losing weight, exercising regularly, and cutting out sugary drinks and processed carbs can reduce your risk of developing diabetes by more than half - even while taking statins. These changes also improve how well statins work to lower cholesterol.
Do I need to check my blood sugar if I’m on statins?
If you have prediabetes, obesity, high blood pressure, or a family history of diabetes, yes. Get a fasting glucose and HbA1c test before starting statins, then again at 3 and 6 months. If you’re already diabetic, monitor your levels more closely - statins can make control harder.
Are there alternatives to statins that don’t raise blood sugar?
Yes - but only for some people. Ezetimibe and PCSK9 inhibitors (like evolocumab) lower cholesterol without affecting blood sugar. But they’re more expensive and usually reserved for those who can’t tolerate statins or need extra lowering. For most, statins remain the best first option.
9 Comments
evelyn wellding
January 16 2026
Just started my statin last month and got my HbA1c checked last week-up from 5.6 to 6.1 😳 But I’m not panicking! My doc said it’s common and I’m still way better off than if I skipped it. Started walking 30 mins a day and cutting soda-already feel lighter! 💪❤️
Chelsea Harton
January 17 2026
statins are just another way pharma makes money off fear
Corey Chrisinger
January 17 2026
It’s wild how medicine keeps giving us trade-offs like this. We’re not curing disease anymore-we’re just negotiating with biology. 🤔 Statins protect your heart but nudge your pancreas toward burnout. Kinda like driving a car with a faulty fuel line-still gets you there, but you gotta check the tank more often. Not evil. Just complex.
Bianca Leonhardt
January 18 2026
Of course your blood sugar went up. You’re 60, overweight, and eat donuts for breakfast. Stop blaming the medicine and take responsibility. This isn’t rocket science.
Travis Craw
January 18 2026
hey i had the same thing happen last year. switched from atorvastatin to pravastatin and my numbers stabilized. just wanted to say it’s possible to find a middle ground. no need to freak out.
Christina Bilotti
January 19 2026
Wow. Someone actually read the entire 2,000-word post and didn’t just scroll to the headline? Congrats. You’ve unlocked the ‘Not a Social Media Zombie’ achievement. 🎮 Now go drink some water and stop Googling your symptoms.
brooke wright
January 19 2026
I’ve been on rosuvastatin for 3 years and my fasting glucose went from 92 to 118. I didn’t know until my sister, who’s a nurse, asked why I was suddenly drinking so much water. I didn’t even connect it. So please, if you’re on statins, get tested. Even if you feel fine. I’m lucky I caught it early.
Henry Ip
January 20 2026
Good breakdown. The real win here is knowing your numbers and staying active. Losing even 10 pounds can undo half the statin-related insulin resistance. And walking after meals? Game changer. Keep doing the work-you’re not fighting the statin, you’re working with your body.
Kasey Summerer
January 22 2026
Statins: because nothing says ‘I love my heart’ like making your pancreas work overtime. 🇺🇸🇺🇸🇺🇸