Muscle cramps on statins can be myopathy or neuropathy-two very different issues. Learn how to tell them apart, what tests to ask for, and how to protect your heart without sacrificing muscle health.
Statin Neuropathy: What It Is, Who It Affects, and How to Manage It
When you take a statin, a class of cholesterol-lowering drugs like atorvastatin or simvastatin used to reduce heart attack risk. Also known as HMG-CoA reductase inhibitors, they work by blocking a liver enzyme that makes cholesterol. But for some people, these drugs don’t just lower cholesterol—they can also damage nerves, leading to a condition called statin neuropathy, a type of peripheral nerve damage caused by long-term statin use. This isn’t muscle pain or cramps—it’s tingling, burning, or numbness in the hands and feet that doesn’t go away with rest.
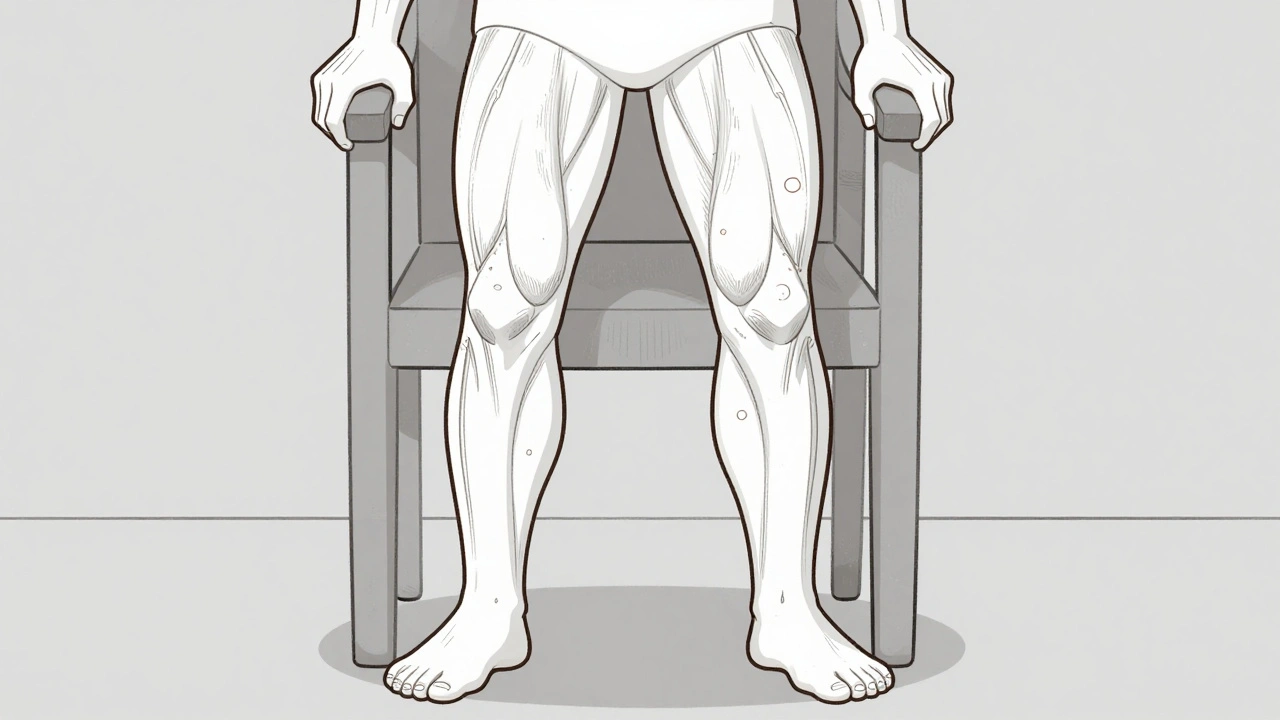
Statin neuropathy is rare, but it’s underdiagnosed. Many doctors assume any nerve pain in someone on statins is just aging or diabetes. But research shows that up to 10% of long-term users report unusual nerve sensations, and in some cases, symptoms improve after stopping the drug. The risk goes up with age, diabetes, kidney problems, or taking multiple medications. It’s not the same as statin myopathy (muscle damage), which is more common. Neuropathy affects the nerves, not the muscles. You might feel like your socks are bunched up, or your toes are asleep—even when you’re not standing. If you’ve been on a statin for over a year and notice new numbness, burning, or weakness in your limbs, it’s not normal. Don’t ignore it.
What makes this tricky is that statins also help prevent strokes and heart attacks, so stopping them isn’t simple. But you don’t have to choose between your heart and your nerves. There are alternatives: switching to a different statin, lowering the dose, adding CoQ10 supplements (some studies show it helps with nerve symptoms), or using non-statin options like ezetimibe or PCSK9 inhibitors. Physical therapy for nerve health, like gentle stretching and balance exercises, can also help manage symptoms. And if you’re worried about cost, remember that many of these alternatives are available as generics, just like statins.
The posts below cover real-world stories and science-backed advice from people who’ve dealt with this. You’ll find guides on how to track your symptoms, what tests your doctor might order, how to talk to your pharmacist about side effects, and what alternatives actually work. Some posts talk about how other drugs—like those for gout or diabetes—can make nerve damage worse. Others show how to use patient assistance programs if you need to switch to a pricier but safer medication. You’ll also learn how to spot early signs before the damage becomes permanent, and how to document your symptoms so your doctor takes you seriously. This isn’t about fear. It’s about knowing your body well enough to ask the right questions—and getting the care you deserve without guessing.