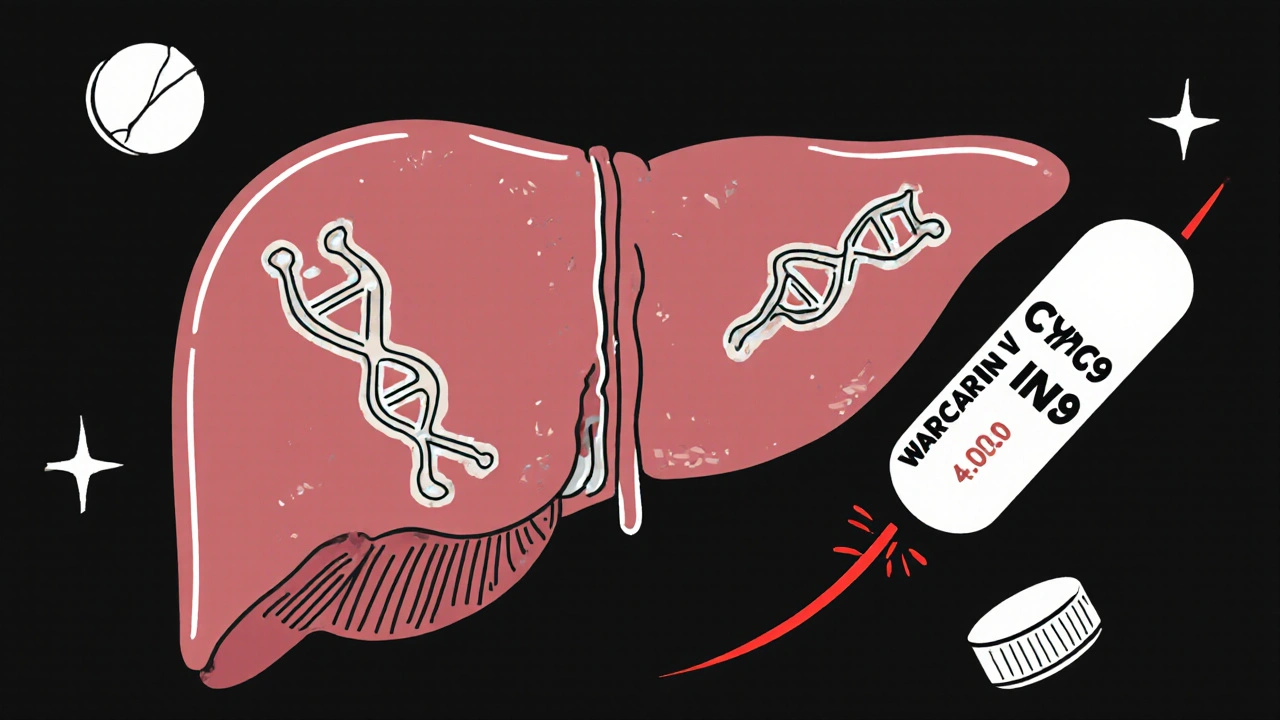
CYP2C9 and VKORC1 gene variants significantly affect warfarin dosing and bleeding risk. Genetic testing can reduce dangerous side effects by up to 32% in the first 90 days of therapy.
Pharmacogenetic Testing: How Your Genes Affect Medication Response
When you take a pill, your body doesn’t treat it the same way everyone else does. That’s because your pharmacogenetic testing, the science of how your genes influence how your body processes drugs. Also known as genetic drug testing, it helps explain why one person needs a low dose of a drug to feel better, while another needs triple that amount—or has a dangerous reaction just from a normal dose. This isn’t science fiction. It’s happening right now in clinics across Canada and the U.S., helping doctors pick the right drug and the right dose before you even take your first pill.
Pharmacogenetic testing looks at specific genes that control how your liver breaks down medications, how your body absorbs them, and how your cells respond. For example, if you have a variation in the CYP2D6 gene, you might process antidepressants, painkillers like codeine, or beta-blockers way too fast—or way too slow. Too fast, and the drug doesn’t work. Too slow, and it builds up to toxic levels. This is why some people get sick from standard doses of tramadol or warfarin, while others need higher doses just to feel relief. The same goes for chemotherapy drugs like capecitabine—some patients develop severe mouth sores because their genes make them extra sensitive. gene-drug interaction, the biological link between your DNA and how a medication behaves in your body is the core idea behind all of this.
It’s not just about avoiding side effects. It’s about getting results faster. If your doctor knows your genetic profile, they can skip the trial-and-error phase. No more weeks of trying different blood pressure pills until one sticks. No more guessing if your anxiety meds will make you nauseous. This is especially helpful for older adults managing multiple prescriptions—like those following the Beers Criteria, a list of medications that pose higher risks for seniors—because your genes can make even safe drugs dangerous if you’re a slow metabolizer. And when you’re on long-term meds for diabetes, heart disease, or chronic pain, getting it right the first time saves money, prevents hospital visits, and reduces stress.
Pharmacogenetic testing doesn’t replace your doctor or pharmacist. It gives them better tools. You still need to talk about your symptoms, your other meds, and your history. But now, your genes are part of the conversation. And with more than 95% of drug reactions linked to individual differences in metabolism, ignoring your genetic profile is like driving blindfolded. The posts below show how this science connects to real-world issues: why some people get rashes from common antibiotics, how QR codes on prescriptions help track side effects, why certain drugs cause insomnia, and how to avoid dangerous interactions with tools like WebMD checkers. Together, they paint a clear picture: your DNA isn’t just about ancestry—it’s your personal drug manual.