Commercial drivers must follow strict DOT medication rules to stay safe and legal. Learn which prescriptions are banned, how to get approved for safe alternatives, and what happens if you're caught using prohibited drugs.
FMCSA Medication Guidelines: What Drivers and Clinicians Need to Know
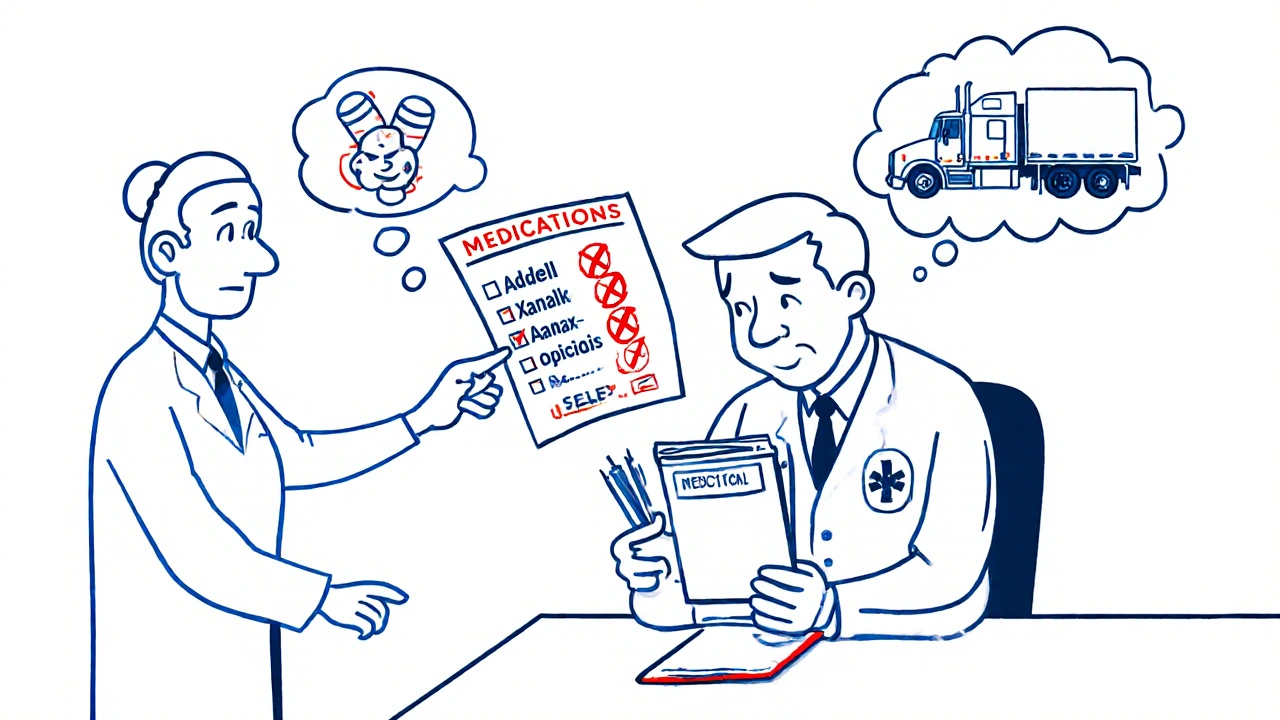
When you're behind the wheel of a commercial truck or bus, your medication choices aren't just personal—they're regulated by the FMCSA medication guidelines, federal rules set by the Federal Motor Carrier Safety Administration to ensure commercial drivers are fit for duty and not impaired by drugs. Also known as DOT drug regulations, these rules define exactly which medications are allowed, which are banned, and when a driver needs a medical exemption to stay on the road. These aren’t suggestions. They’re legal requirements that can mean the difference between keeping your job and losing your CDL.
The FMCSA medication guidelines, a set of federal standards governing drug use for commercial motor vehicle operators are tightly linked to the DOT drug policy, the Department of Transportation’s framework for drug testing and medical certification. If a driver takes a medication that causes drowsiness, dizziness, or slowed reaction time—even if it’s prescribed—it’s flagged. Common culprits include opioids like tramadol, certain antidepressants, sedatives, and even some allergy meds. The guidelines don’t ban all meds, though. Many drivers safely use blood pressure pills, thyroid meds, or insulin as long as their condition is stable and they’re cleared by a medical examiner.
What many drivers don’t realize is that the FMCSA medication guidelines, federal rules set by the Federal Motor Carrier Safety Administration to ensure commercial drivers are fit for duty and not impaired by drugs require full disclosure. Hiding a prescription can get you disqualified. But so can refusing to use a necessary drug. The system isn’t about punishment—it’s about balance. A driver with controlled diabetes on insulin can keep driving. A driver on a sleep aid that causes next-day grogginess cannot. Medical examiners use a checklist based on FDA labels, drug interaction databases, and clinical evidence to make these calls. And yes, that means your pharmacist’s advice matters just as much as your doctor’s.
These rules also affect how clinics and pharmacies work with commercial drivers. A doctor prescribing a new medication to a trucker has to check if it’s on the FMCSA’s prohibited list. Pharmacies need to flag interactions—like mixing tramadol with antidepressants—that could trigger seizures or drowsiness. That’s why so many of the posts below focus on real-world medication risks: drug interactions, medication side effects, and medication safety aren’t just general health topics—they’re job-safety issues for drivers.
Below, you’ll find practical guides on how to manage medications safely while staying compliant. From understanding why certain painkillers are off-limits, to learning how to use visual dosing tools to avoid mistakes, to knowing when a generic drug is just as safe as a brand name—every article here ties back to one goal: helping drivers stay healthy, legal, and on the road.