Immunosuppressants keep transplanted organs alive but come with serious risks like infection, cancer, and organ damage. Learn how to take them safely, avoid rejection, and live longer with your transplant.
Anti-Rejection Drugs: What They Are, How They Work, and Who Needs Them
When someone gets a new organ—whether it’s a kidney, heart, or liver—their body doesn’t just welcome it. The immune system sees it as an invader and tries to attack. That’s where anti-rejection drugs, medications that suppress the immune system to prevent organ rejection after transplant. Also known as immunosuppressants, they’re not optional—they’re life-sustaining. Without them, most transplants fail within days or weeks. These drugs don’t cure anything. They just stop the body from destroying its own new organ.
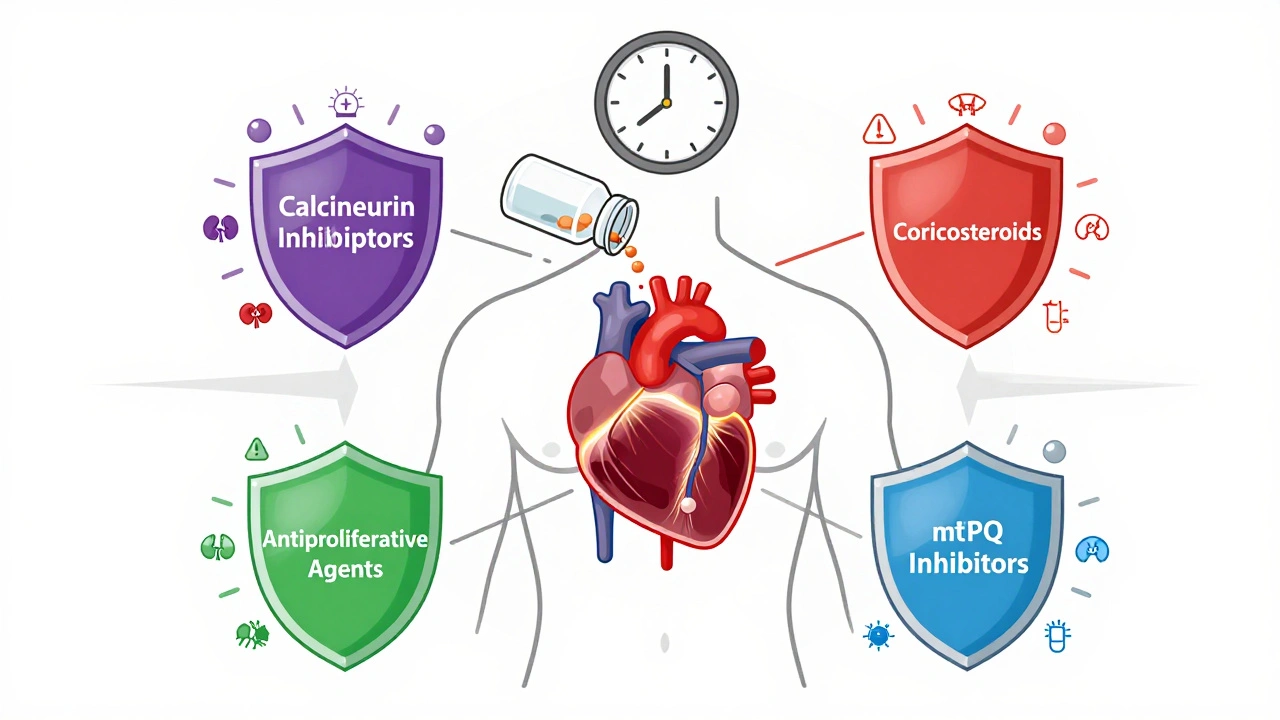
Anti-rejection drugs don’t work the same way. Some, like cyclosporine, a calcineurin inhibitor that blocks T-cell activation, target specific immune cells. Others, like mycophenolate, a drug that stops immune cells from multiplying, slow down the whole response. Then there’s steroids, like prednisone, used early after transplant to calm inflammation. Most patients take a mix—three or four drugs at once—to cover all the ways the immune system might try to reject the organ. It’s not magic. It’s science. And it’s messy. These drugs lower your defenses against infections, raise your risk of certain cancers, and can damage kidneys or raise blood pressure. But for transplant patients, the trade-off is worth it.
People don’t take these drugs for a few months. They take them for life. That’s why understanding side effects, managing costs, and knowing when to ask for help matters more than ever. You’ll find real stories here—not just textbook facts—about how people handle daily pills, deal with unexpected rashes, fight insurance denials, and balance the fear of rejection with the risk of infection. Some posts talk about how anti-rejection drugs interact with other meds, like statins or diabetes pills. Others show how patient assistance programs help when brand-name versions cost thousands. You’ll learn what tests doctors miss, why some people still reject organs despite taking their pills, and how new research is changing what we thought we knew about cancer risk after transplant.
This isn’t a list of drug names. It’s a guide for people living with the reality of transplants—the daily choices, the hidden struggles, the quiet wins. Whether you’re a patient, a caregiver, or just trying to understand what happens after the surgery ends, these posts give you the practical truth no brochure ever will.