Most people think hemorrhoids are just an embarrassing annoyance-but they’re actually a common medical condition that affects 75% of adults at some point in their lives. The truth? You might already have them and not even know it. The real problem isn’t having hemorrhoids-it’s not knowing whether they’re internal or external, and what to do about them.
What Exactly Are Hemorrhoids?
Hemorrhoids aren’t some weird growth or infection. They’re normal blood vessels in your rectum and anus that help control stool passage. Think of them like little cushions that swell up when under too much pressure. When they get irritated or stretched out-thanks to constipation, pregnancy, sitting too long, or heavy lifting-they become painful or bleed. That’s when they turn from helpful structures into a problem. The key to treating them right is knowing where they are. There are two main types: internal and external. And they’re not just different in location-they feel completely different, need different treatments, and can be easily confused with other issues.Internal Hemorrhoids: The Silent Ones
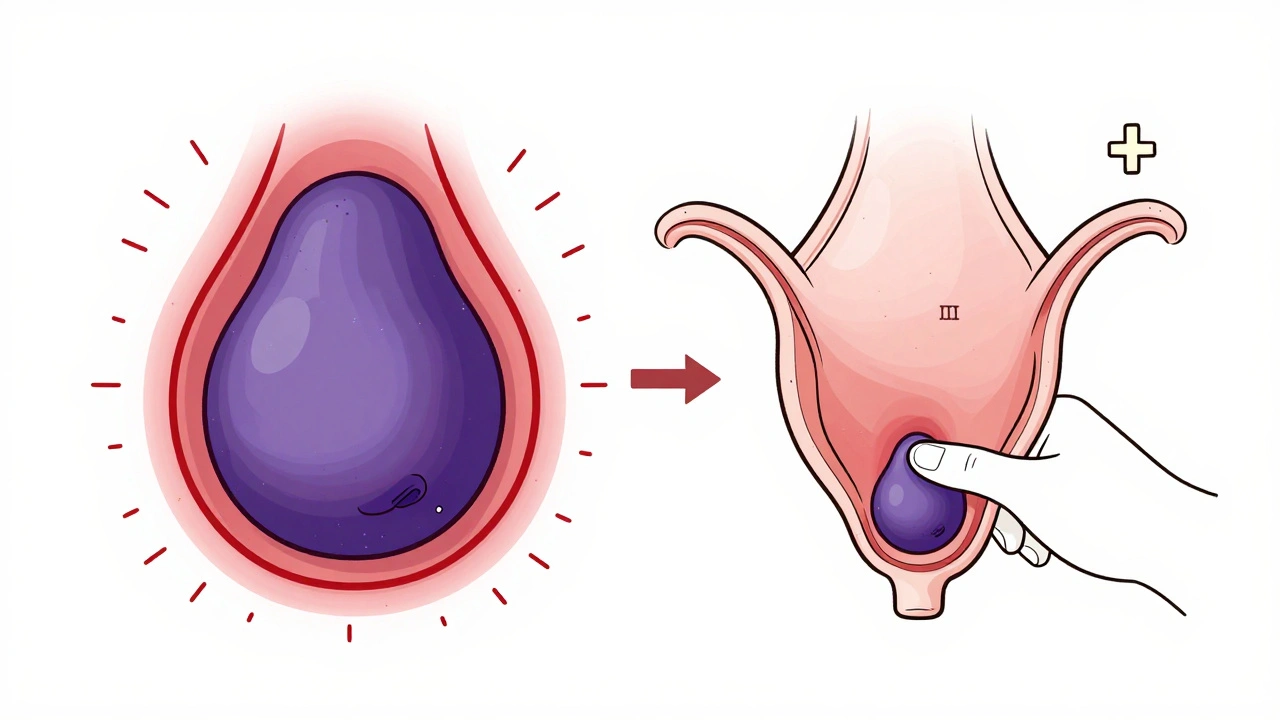
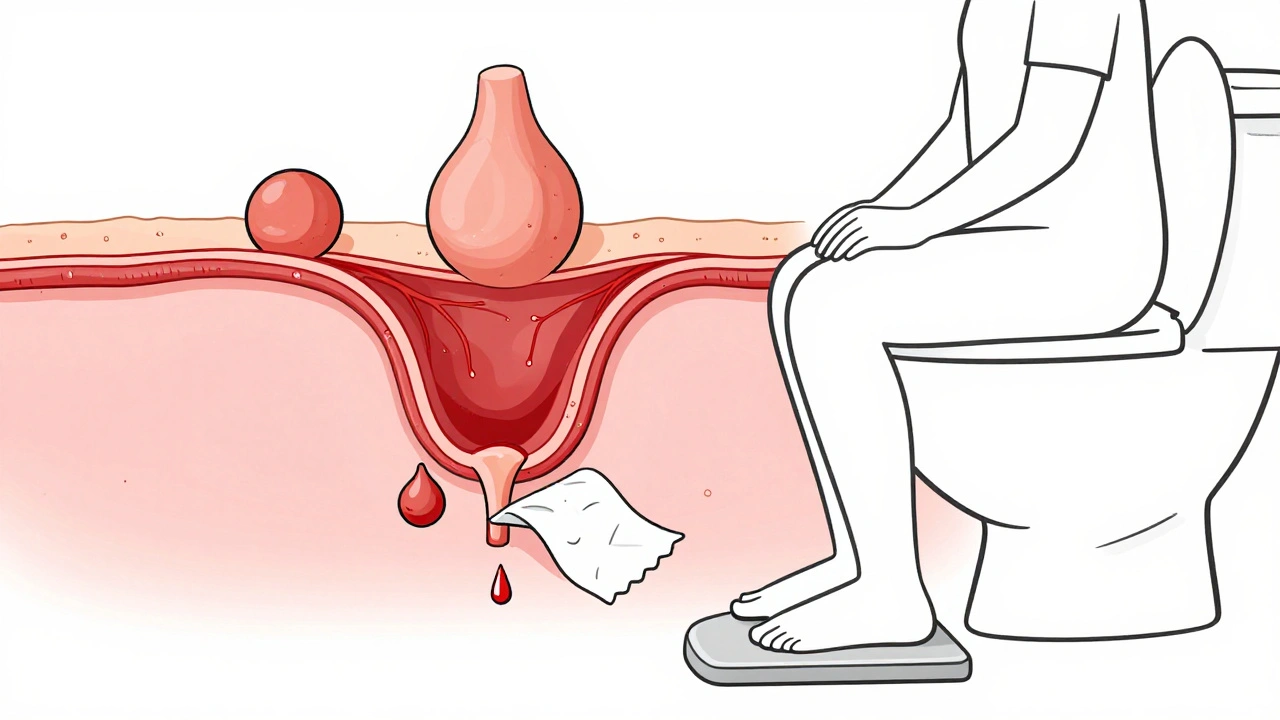
Internal hemorrhoids sit inside the rectum, above a line called the dentate line. This area has no pain nerves, so even when they swell, you often won’t feel pain. That’s why many people don’t realize they have them until they see bright red blood on the toilet paper or in the bowl after a bowel movement. Doctors grade internal hemorrhoids on a scale from I to IV:- Grade I: Just swollen. Bleeds sometimes, but doesn’t pop out.
- Grade II: Protrudes during straining but pops back in on its own.
- Grade III: Comes out and stays out-but you can push it back in.
- Grade IV: Stays out permanently. Can’t be pushed back. Often very uncomfortable.
External Hemorrhoids: The Painful Ones
External hemorrhoids form under the skin around your anus. This area is packed with nerves, so even a small swelling can feel like a throbbing, burning, or stabbing pain. You’ll likely see or feel a soft, skin-colored lump near your anal opening. The worst kind? Thrombosed external hemorrhoids. This happens when a blood clot forms inside the swollen vein. It turns into a hard, purple or blue lump that feels like a marble under your skin. The pain hits fast and hard-often making sitting, walking, or even lying down unbearable. Unlike internal hemorrhoids, external ones rarely bleed. Instead, they cause itching, swelling, and sharp pain that gets worse when you sit or wipe. Many people delay seeing a doctor because they think it’s just a pimple or irritation. But thrombosed hemorrhoids need quick attention-especially within the first 72 hours.Can You Have Both at Once?
Yes. And it’s more common than you think. Many people have a mix: an internal hemorrhoid that’s prolapsed (sticking out) and an external one right next to it. This makes symptoms confusing. You might have bleeding from inside, plus pain and swelling from outside. That’s why self-diagnosis is risky. One patient I spoke with spent six months treating what he thought was an external hemorrhoid with creams and sitz baths. Turns out, it was an anal fissure-a small tear in the lining. The treatments were useless. He only got relief after a doctor did a visual exam.What Causes Hemorrhoids?
It’s not just “eating too little fiber.” While that’s a big part, other factors pile up:- Chronic constipation or diarrhea
- Straining during bowel movements
- Sitting on the toilet longer than 5 minutes
- Pregnancy (25-35% of pregnant women get them)
- Obesity
- Heavy lifting
- Aging (tissues lose support over time)
Home Treatments That Actually Work
For mild cases, you don’t need surgery. Start here:- Drink more water. Aim for 8-10 glasses a day. Dehydration hardens stool, which means more straining.
- Eat 25-30 grams of fiber daily. Oats, beans, apples, broccoli, chia seeds, and whole grains help. Most people get less than half that.
- Take sitz baths. Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation.
- Use witch hazel pads. They’re gentle, anti-inflammatory, and available over the counter.
- Avoid straining. If you don’t go after 5 minutes, get up. Try again later.
When You Need Medical Help
If home care doesn’t help in a week or two, or if symptoms get worse, it’s time to see a doctor. Here’s when to act:- Rectal bleeding that keeps coming back
- Pain so bad you can’t sit or walk
- A lump that won’t go away or gets bigger
- Dizziness, fatigue, or pale skin (signs of blood loss)
- Changes in bowel habits (new constipation, diarrhea, narrow stools)
Minimally Invasive Procedures
For internal hemorrhoids that don’t respond to lifestyle changes, doctors have several safe, office-based options:- Rubber band ligation: A tiny band is placed around the base of the hemorrhoid, cutting off blood flow. It shrinks and falls off in a few days. Works in 90% of cases for Grades I-III.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it.
- Infrared coagulation: Heat is applied to scar the tissue and shrink the vein.
Thrombosed External Hemorrhoids: The Emergency Fix
If you’ve got a sudden, hard, purple lump that’s throbbing with pain, don’t wait. See a doctor within 72 hours. The best treatment? A small incision to drain the clot. Done under local numbing, it takes 10 minutes and gives almost instant relief. Waiting longer than 3 days? The clot starts to harden and heal on its own-but the pain lasts for weeks. And you’re left with a skin tag that can cause ongoing irritation.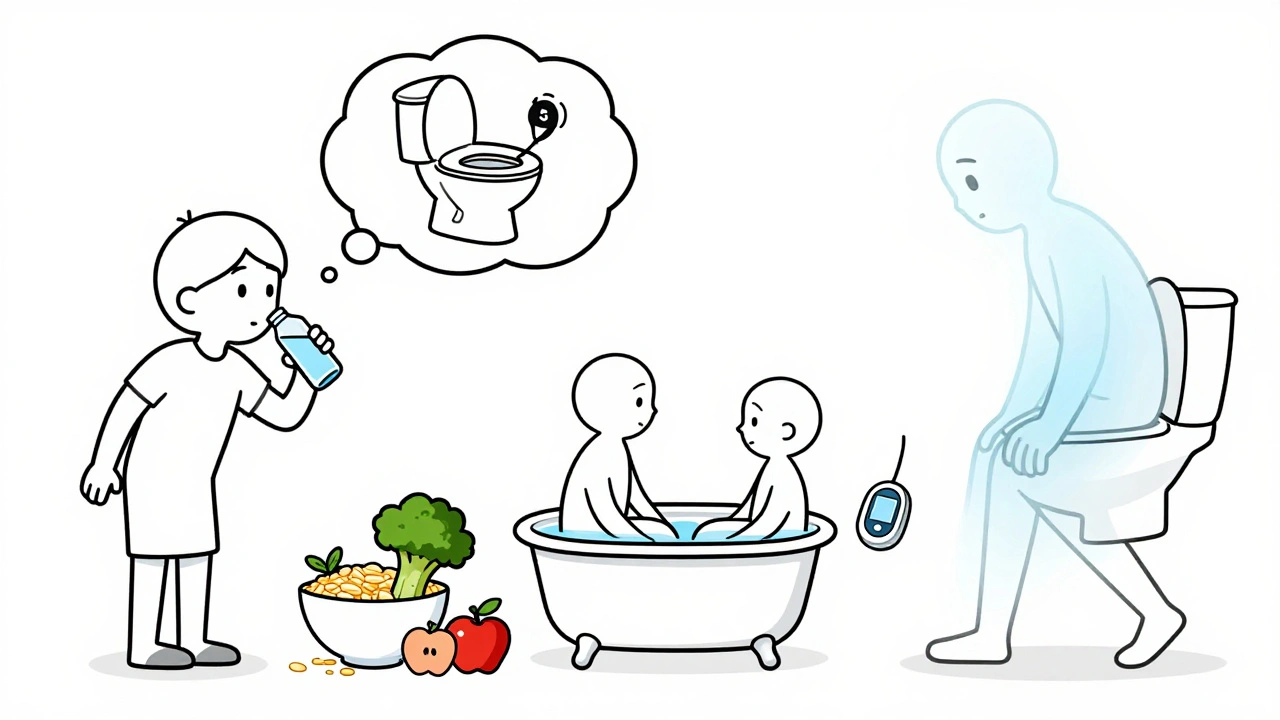
Surgery: Last Resort, But Effective
For severe, recurrent, or Grade IV hemorrhoids, surgery may be needed. Two main options:- Hemorrhoidectomy: The hemorrhoid is completely cut out. It’s the most effective method-95% success rate. But recovery takes 2-4 weeks. Pain is real, and you’ll need prescription painkillers.
- Stapled hemorrhoidopexy: The prolapsed tissue is pulled back up and stapled into place. Less pain than removal, but higher chance of recurrence.
Prevention Is the Real Cure
The biggest mistake people make? Treating the symptom, not the cause. Hemorrhoids come back if you don’t change your habits. Studies show that people who stick to high-fiber diets and drink enough water have only a 5-10% chance of recurrence. Those who go back to bad habits? Up to 50% get them again. Here’s what works long-term:- Make fiber a daily habit-not just when you’re bleeding.
- Move your body. Even a 20-minute walk daily helps bowel function.
- Don’t sit on the toilet reading or scrolling. Set a timer.
- If you’re pregnant, sleep on your left side. It reduces pressure on pelvic veins.
- Ignore online “miracle cures.” No cream, oil, or supplement cures hemorrhoids. Only evidence-based treatments do.
Frequently Asked Questions
Can hemorrhoids turn into cancer?
No, hemorrhoids do not turn into cancer. But rectal bleeding-a common symptom of hemorrhoids-can also be a sign of colorectal cancer. That’s why any new or persistent bleeding needs evaluation by a doctor. Never assume it’s just hemorrhoids.
Are hemorrhoids more common in men or women?
They affect both genders equally overall. But women are more likely to develop them during pregnancy due to increased pressure on pelvic veins. Men are more likely to develop them from heavy lifting or chronic constipation from poor diet.
Can I use ice packs for external hemorrhoids?
Yes, but only for short-term relief. Wrap an ice pack in a towel and apply for 10-15 minutes at a time. It reduces swelling and numbs pain. But don’t use it long-term-it won’t shrink the hemorrhoid. Sitz baths and fiber are what actually help heal it.
Will hemorrhoids go away on their own?
Mild ones can improve within a few days with home care. But they rarely disappear completely unless the root cause-like constipation or sitting too long-is fixed. Without lifestyle changes, they’ll likely come back.
Is it safe to pop a hemorrhoid?
Never. Popping a hemorrhoid can cause infection, severe bleeding, or scarring. Thrombosed hemorrhoids should only be drained by a doctor in a sterile setting. DIY methods are dangerous and ineffective.
12 Comments
Katherine Chan
December 8 2025
I had no idea hemorrhoids were so common! I thought I was the only one dealing with this after my second kid. Sitz baths saved my life. Seriously, try them. Warm water, 15 minutes, no phone. It’s like a spa day for your butt. You’ll thank me later.
Also, fiber isn’t just for grandmas. I started eating chia seeds in my oatmeal and my bowel movements went from 'battle' to 'smooth ride'.
Tim Tinh
December 9 2025
omg i legit thought i had a pimple for 3 weeks. turned out to be a thrombosed external. went to urgent care and they just cut it open like it was nothing. 10 mins. no surgery. instant relief. why do people wait??
Philippa Barraclough
December 10 2025
The grading system for internal hemorrhoids is clinically useful but rarely discussed outside medical circles. It's worth noting that Grade II and III often respond well to outpatient procedures like rubber band ligation, which has a 90% success rate and minimal downtime. What's concerning is how many patients delay care due to embarrassment, mistaking bleeding for 'just hemorrhoids' when it could be colorectal pathology. The dentate line's innervation pattern explains why internal hemorrhoids are painless until they prolapse or thrombose, which is why clinical examination remains indispensable. Self-diagnosis via internet forums is a dangerous practice that frequently leads to mismanagement.
Olivia Portier
December 11 2025
I used to sit on the toilet scrolling for 20 mins like it was my job. Then I got a little footstool. Changed everything. My body just knows how to go when my knees are higher than my hips. No more straining. No more burning. I feel like a genius. Also, drink water like it’s your job. I carry a bottle everywhere now. No more 'oh I'll just wait till I get home'. Just go. Your butt will thank you.
And no, ice packs don't fix it. They just numb it. Fiber and sitz baths? That's the real magic.
Asset Finance Komrade
December 12 2025
I don't know why people are so shocked. Everyone gets hemorrhoids. It's like getting a pimple. But instead of treating it like a normal bodily thing, we turn it into this huge shame thing. Like it's a moral failure. It's not. It's biology. You sit too long, you eat too little fiber, you strain - boom. Happens to everyone. Stop acting like it's a personal failure. Just fix the habits. Easy.
om guru
December 14 2025
Hemorrhoids are a natural physiological phenomenon that arises due to increased venous pressure in the anorectal region. Prevention through dietary fiber intake and adequate hydration remains the cornerstone of management. Medical intervention is indicated only when conservative measures fail. Avoidance of prolonged sitting and proper toileting posture are non-negotiable for long term relief. The emphasis on lifestyle modification cannot be overstated.
Jennifer Blandford
December 14 2025
I cried in the bathroom for an hour last week because I thought I was dying. Turned out it was a Grade II internal. I did the sitz baths, started eating lentils like they were candy, and now I’m basically a hemorrhoid whisperer. I tell everyone. If you’re bleeding, don’t Google it. Don’t wait. Just go to a doctor. It’s not embarrassing. It’s just your body asking for help. You wouldn’t ignore a sprained ankle. Don’t ignore your butt.
Raja Herbal
December 14 2025
Oh so now we're blaming sitting on the toilet? What about the fact that 90% of people in India eat rice and lentils daily and still get hemorrhoids? Fiber doesn't fix everything. Maybe it's the climate. Maybe it's the squat toilets. Maybe it's the fact that your body just decides to rebel one day. I've had them since I was 19. No amount of chia seeds helped. I just learned to live with it. And yes, I still sit on the toilet reading. I don't care.
Brianna Black
December 15 2025
I’m a nurse and I’ve seen so many patients delay care because they were too embarrassed. One woman waited 18 months because she thought it was 'just a pimple'. She ended up needing surgery. Hemorrhoids are not a personal failing. They’re a medical condition. Period. Please don’t wait. See a doctor. You’re not alone. And no, ice packs won’t cure it. Fiber and hydration will. Your body deserves better than shame.
Tiffany Sowby
December 16 2025
Ugh. Another article telling me I’m lazy because I sit too long. Like I don’t already feel guilty enough. My job is 10 hours a day at a desk. I have two kids. I don’t have time to sit in warm water for 20 minutes. And no, I’m not eating more fiber. I don’t like broccoli. Deal with it. Maybe the real problem is that doctors keep shaming people instead of offering realistic solutions.
Ryan Brady
December 17 2025
I tried the footstool. Didn’t work. I just started standing up to poop. Like, full on standing. No toilet. Just over the bowl. It’s weird but it works. No straining. No pain. No more hemorrhoids. I’ve been doing it for 6 months. No one talks about this. Why? Is it because Americans are too soft? 🤔
Stacy Tolbert
December 18 2025
I had a thrombosed one last year. The doctor drained it and I cried because it hurt so much. But then I felt like a new person. I wish I’d gone sooner. I spent three weeks thinking I was going to die. It was just a clot. So simple. So fixable. Why do we make everything so dramatic?