More than 1 in 3 adults over 60 are taking five or more prescription drugs. That’s not just common-it’s dangerous. Many people don’t realize that taking a few extra pills can turn into a silent crisis: dizziness that leads to a fall, confusion that looks like dementia, or a heart rhythm that suddenly goes haywire. The problem isn’t the medications themselves-it’s how they interact when stacked together. A polypharmacy risk checklist isn’t optional. It’s a lifeline.
What Exactly Is Polypharmacy-and Why Should You Care?
Polypharmacy means taking five or more medications at the same time. It’s not always bad. Someone with diabetes, high blood pressure, heart disease, and arthritis might need all those drugs. But when prescriptions pile up without a clear plan, risks skyrocket. Each extra pill increases the chance of a dangerous drug interaction by nearly 40%. That’s not a guess. It’s from a 2022 study of over 700 cancer patients. And it’s even worse if you’re older. The CDC found that 33% of people in their 60s and 70s are on five or more meds. By 2030, that number will jump 42%.The Top 5 High-Risk Medication Combos You Need to Know
Some combinations are like walking a tightrope without a net. Here are the most dangerous ones you’ll see in real clinics:- Warfarin + cranberry juice: Warfarin thins your blood. Cranberry juice makes it work too well. Result? Uncontrolled bleeding-even from a minor bump.
- Statins + grapefruit juice: Grapefruit blocks how your body breaks down statins. That leads to muscle breakdown (rhabdomyolysis), which can fry your kidneys.
- Blood pressure meds + decongestants (like pseudoephedrine): Decongestants spike your blood pressure. If you’re already on meds to lower it, this combo can trigger a stroke or heart attack.
- Acetaminophen + oxycodone + prochlorperazine: This trio shows up too often in ER visits. The painkiller and nausea drug both cause drowsiness. Add acetaminophen, and your liver gets hammered. Many patients don’t even realize they’re taking all three-because they’re in different pills.
- Benzodiazepines (like diazepam) + opioids: Both depress your breathing. Together, they’re a leading cause of accidental overdose in older adults.
These aren’t rare. A 2022 study found lisinopril, furosemide, and calcium supplements involved in over 70 drug interactions each. And don’t forget supplements. Nearly 40% of dangerous interactions in cancer patients came from over-the-counter vitamins, herbs, or minerals-not prescriptions.
The Beers Criteria: Your Secret Weapon Against Bad Prescriptions
The Beers Criteria, last updated in 2019, is the gold standard for spotting risky drugs in older adults. It’s not a list of banned drugs-it’s a warning system. Medications flagged include:- Anticholinergics (like diphenhydramine/Benadryl): These cause brain fog, dry mouth, constipation, and can trigger delirium.
- Benzodiazepines (like lorazepam): Linked to falls, memory loss, and addiction.
- α1-blockers (like doxazosin): Increase fall risk by messing with blood pressure control.
- Nonsteroidal anti-inflammatories (NSAIDs like ibuprofen): Can cause kidney failure, stomach bleeds, and worsen heart failure.
Doctors don’t always check the Beers list. But you can. Bring this checklist to every appointment. Ask: “Is this still necessary? Could it be replaced with something safer?”
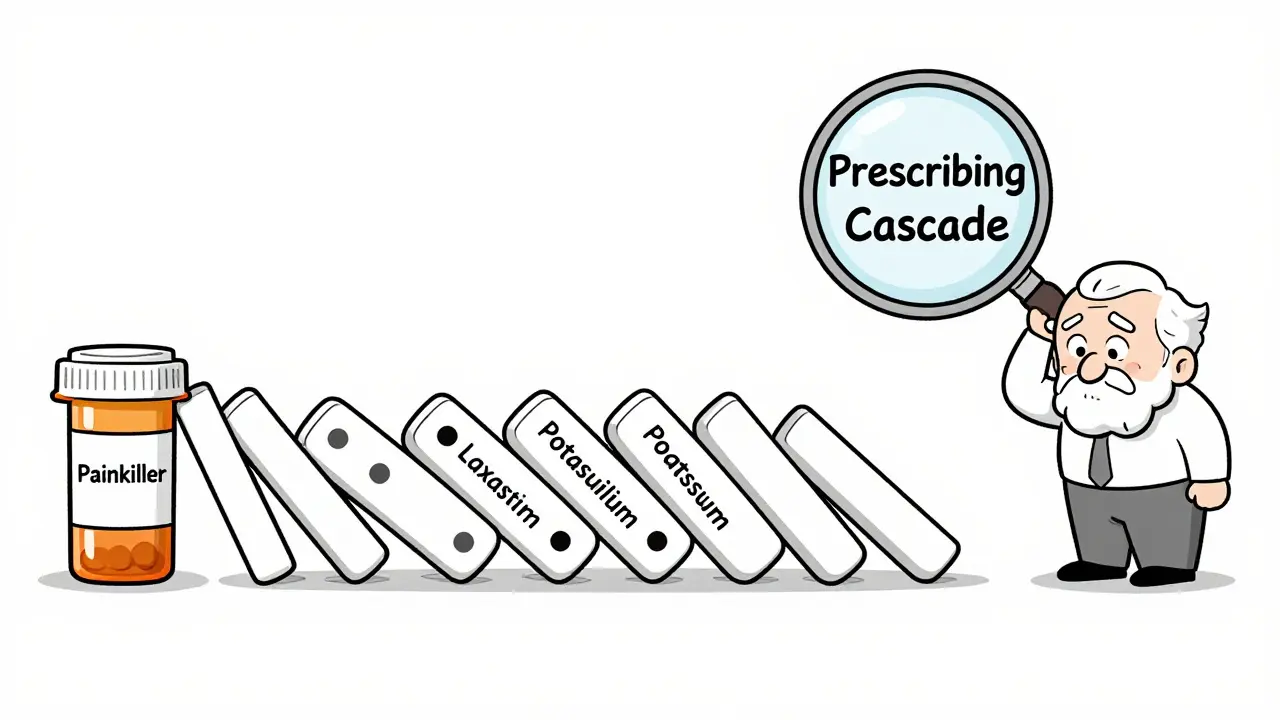
Prescribing Cascades: When One Drug Causes Another Problem
Here’s how it usually goes: You take a painkiller. It causes constipation. So your doctor prescribes a laxative. The laxative causes electrolyte imbalance. Now you need a potassium supplement. That messes with your heart meds. Suddenly, you’re on eight pills instead of two-and no one sees the chain.This is called a prescribing cascade. It’s one of the biggest reasons polypharmacy spirals out of control. A 2023 University of Rochester report called it “the silent epidemic.” There’s no quarterback in your care team. Your cardiologist doesn’t talk to your pain specialist. Your pharmacist isn’t in the loop. You’re left guessing.
Fix it by asking: “What problem is this drug solving? And what side effect might it cause?” If the answer is vague, push back.
Your Polypharmacy Risk Checklist: 7 Steps to Take Today
You don’t need a PhD to protect yourself. Here’s a practical, step-by-step checklist anyone can use:- Make a complete list: Write down every pill, patch, inhaler, vitamin, herb, and OTC drug you take-even aspirin or melatonin. Include doses and how often.
- Bring it to every appointment: Don’t rely on memory. Don’t let the doctor assume. Hand them the list. Say, “I want to make sure nothing here clashes.”
- Ask about the Beers Criteria: “Are any of these on the list of drugs to avoid for older adults?”
- Check for food interactions: Grapefruit, cranberry, alcohol, and even high-sodium foods can change how your meds work. Ask your pharmacist.
- Look for red flags: Are you dizzy? Confused? Falling? Feeling extra tired? These aren’t just “getting older.” They’re warning signs.
- Try the ARMOR method: Assess your meds. Review what’s necessary. Minimize what’s not. Optimize dosing. Reassess every 3-6 months.
- Get a pharmacist consult: Most pharmacies offer free med reviews. Use them. Pharmacists catch 60% more interactions than doctors do.

What Happens When You Don’t Act
The numbers are terrifying. Every year, 1.3 million older adults end up in the ER because of bad drug reactions. 350,000 are hospitalized. 27.8% of hospital admissions for people over 65 are linked to medications. And 60-70% of those cases involve polypharmacy.It’s not just about money. The CDC estimates polypharmacy costs seniors $37 billion a year in drug bills alone-before you add ER visits, rehab, or nursing home stays.
But here’s the hopeful part: One 72-year-old cancer patient reduced her meds from 12 to 7 using the ARMOR tool. No loss of effectiveness. Just fewer side effects. She felt like herself again.
What’s Next? The Future of Safe Med Use
New tools are coming. Some hospitals now use AI heatmaps to predict which drug combos are most likely to cause hospitalization. Smart pill bottles track if you’re taking your meds. Wearables detect early signs of dizziness or irregular heartbeat. Pharmacogenomics-testing your genes to see how you process drugs-is starting to show up in clinics.But none of that matters if you don’t start with the basics. No algorithm replaces asking: “Why am I on this? Is it still helping? What could go wrong?”
The system is broken. But you don’t have to be a victim. Take control. Use the checklist. Talk to your pharmacist. Say no to the next pill unless you know why you need it.
What’s the most dangerous drug combination for seniors?
The most dangerous combo is benzodiazepines (like Valium or Xanax) with opioids (like oxycodone or hydrocodone). Together, they slow breathing to dangerous levels and are a leading cause of accidental overdose in older adults. Other top risks include warfarin with cranberry juice and statins with grapefruit juice.
Can over-the-counter meds cause polypharmacy risks?
Absolutely. Studies show that nearly 40% of dangerous interactions in older adults involve OTC drugs or supplements-not prescriptions. Common culprits include diphenhydramine (Benadryl), ibuprofen, melatonin, fish oil, and herbal products like St. John’s wort. Always include them on your med list.
How often should I review my medications?
At least every 3 to 6 months, or anytime you start or stop a drug-even something small like a new vitamin. The WHO recommends regular reviews for anyone on five or more medications. Many pharmacies offer free med reviews; use them.
What’s the ARMOR tool and how do I use it?
ARMOR stands for Assess, Review, Minimize, Optimize, and Reassess. Start by listing every medication you take. Then review each one: Is it still needed? Can it be lowered? Is there a safer alternative? Remove what’s unnecessary. Optimize dosing. Reassess every few months. It’s a simple process used successfully by cancer patients to cut their meds from 12 to 7 safely.
Should I stop a medication if I think it’s causing side effects?
Never stop cold turkey. Some meds, like blood pressure or antidepressant drugs, can cause dangerous withdrawal. Instead, write down your symptoms-dizziness, confusion, fatigue-and bring them to your doctor or pharmacist. Ask: “Could this be from one of my meds?” Then work together on a safe taper plan.
Do electronic health records help prevent bad drug combos?
They’re supposed to, but they often fail. A 2021 study found doctors override 96% of drug interaction alerts because they’re too frequent and not personalized. If your doctor doesn’t check your full med list manually, don’t rely on the system. Bring your own list to every visit.

9 Comments
josh plum
January 5 2026
Look, I don't care how many studies you cite - big pharma and the FDA are in bed together. They want you dependent on pills because it's more profitable than curing anything. That 'Beers Criteria'? A joke. They don't even update it to reflect real-world data. I've seen people get weaned off 10 meds and feel 20 years younger. But nope - doctors keep prescribing like they're playing Tetris with your organs. And don't even get me started on supplements being labeled 'natural' - that's just a loophole for poison with a smiley face.
They're poisoning us slowly and calling it 'standard care.' Wake up.
PS: Grapefruit juice isn't the enemy. The system is.
Jason Stafford
January 5 2026
Let me tell you what they don't want you to know: every single one of those 'dangerous combos' was engineered to keep you coming back. The warfarin-cranberry thing? That's not an accident - it's a trap. Cranberry juice is cheap, accessible, and people think it's 'healthy.' But the moment you start taking it, you're a walking lawsuit waiting to happen. And who benefits? The insurance companies who get to bill for ER visits. The hospitals who charge $12,000 for a blood test. The drug companies who sell you the next pill to fix the last pill's side effects.
This isn't medicine. It's a pyramid scheme with stethoscopes.
I've stopped trusting doctors since my aunt got prescribed 17 pills and died from a 'drug interaction.' They didn't even look at her supplement list. They didn't care. They just kept writing prescriptions like it was a video game.
Cassie Tynan
January 6 2026
Oh wow, another article that treats older people like walking pharmacy catalogs. Let me guess - the next step is mandatory DNA testing before you're allowed to take aspirin?
Look, I get it. Polypharmacy is a mess. But here's the real problem: we treat aging like a disease to be managed, not a natural process to be lived. Why is it that when a 25-year-old takes three pills, it's 'self-care'? But when a 70-year-old does the same, it's 'a silent crisis'? We've turned vulnerability into a medical emergency.
Also, the ARMOR method sounds like a superhero training program. Can we get a T-shirt? 'I survived the Beers Criteria and all I got was this lousy life.'
But seriously - pharmacists are the unsung heroes here. If your pharmacist doesn't know your meds better than your doctor does, you're doing it wrong.
Rory Corrigan
January 6 2026
It's funny how we've turned medicine into a ritual. We don't just take pills anymore - we perform them. Morning routine: coffee, blood pressure med, statin, vitamin D, omega-3, melatonin, calcium, and a prayer.
But here's the truth no one wants to say: we're not just overdosing on drugs - we're overdosing on control. We want to outsmart aging, outmaneuver death, out-engineer entropy. But the body isn't a machine. It's a story. And sometimes, the best thing you can do is stop adding chapters.
I watched my grandfather reduce his meds from 11 to 4. He didn't live longer. But he lived better. He sat on the porch. He talked to the birds. He didn't need a pill to feel peace.
Maybe the real risk isn't the drugs. It's forgetting that life doesn't come in 500mg tablets.
Stephen Craig
January 7 2026
Pharmacists catch more interactions because they're the only ones paid to actually read the labels.
Bring your list. Ask the questions. Do it every six months.
Simple. Not easy. But simple.
Connor Hale
January 8 2026
I’ve been on five meds for five years. I didn’t realize how foggy I was until I skipped one by accident - and suddenly remembered what it felt like to wake up without dread.
My doctor was shocked I hadn’t mentioned it. Turns out, I thought the dizziness was just ‘getting old.’
Now I review everything every six months. No drama. No panic. Just questions.
And yeah - I told my pharmacist about the fish oil. He said it’s probably fine. Good enough for me.
Roshan Aryal
January 8 2026
Western medicine is a colonial project disguised as science. You think these 'drug interactions' are accidental? They're manufactured. The Beers Criteria? A Western-centric list that ignores Ayurveda, Traditional Chinese Medicine, and indigenous healing systems that have managed elders for millennia without polypharmacy.
And yet, here you are, bowing to American pharmaceutical guidelines like they're sacred texts. You think grapefruit juice is dangerous? Try telling a Punjabi grandmother that her turmeric and ashwagandha are 'risky supplements.' She'll laugh and feed you chai.
Stop trusting a system built to profit from your fear. Start trusting your body - and your culture.
Also, your 'checklist' is just another way to make you feel like you need permission to live. You don't.
Jack Wernet
January 9 2026
Thank you for this comprehensive and well-researched piece. The data on polypharmacy-related ER visits and hospitalizations is both sobering and actionable. I particularly appreciate the emphasis on pharmacist consultations - they are often underutilized but critically positioned to identify interactions that clinicians may miss due to time constraints or fragmented records.
It is also important to note that while the Beers Criteria is a vital tool, its implementation requires cultural and systemic support. Clinicians must be trained not just to consult the list, but to engage in shared decision-making with patients - especially those who may be hesitant to question authority figures in healthcare.
Empowering patients with clear, practical steps - like maintaining a written medication list - is not just good practice; it is ethical care.
bob bob
January 9 2026
My grandma took 14 pills a day. She was always tired, confused, and kept falling. We took her to a geriatric pharmacist - she cut it to 6. Now she bakes cookies, plays with her grandkids, and remembers my birthday.
It wasn’t magic. It was just someone actually listening.
Bring your list. Talk to your pharmacist. Don’t wait for a crisis.
And yeah - grapefruit juice is fine if you’re not on statins. But if you are? Skip it. Easy.