When your liver starts storing too much fat-not from drinking alcohol, but from how your body handles sugar and fat-it’s not just a warning sign. It’s a full-blown condition called metabolic-associated fatty liver disease, or MASLD. Once known as NAFLD, this isn’t just about being overweight. It’s about insulin resistance, inflammation, and a liver struggling to keep up. Right now, about 1 in 3 adults worldwide have it. And if you’re carrying extra weight, especially around your middle, your risk jumps even higher. The good news? You can reverse it. Not with magic pills, but with real, proven changes-and one of the most powerful tools now available is a class of drugs called GLP-1 receptor agonists.
What Exactly Is MASLD?
MASLD isn’t just fatty liver. It’s fatty liver plus metabolic trouble. The diagnosis doesn’t rely on ruling out other causes anymore-it’s based on what’s present: fat in the liver (more than 5% of liver cells) and at least one metabolic issue like obesity (BMI over 30), type 2 diabetes, high blood pressure, or abnormal cholesterol. This shift, made official in 2023 by liver experts, means doctors are now looking for the root cause, not just the symptom.
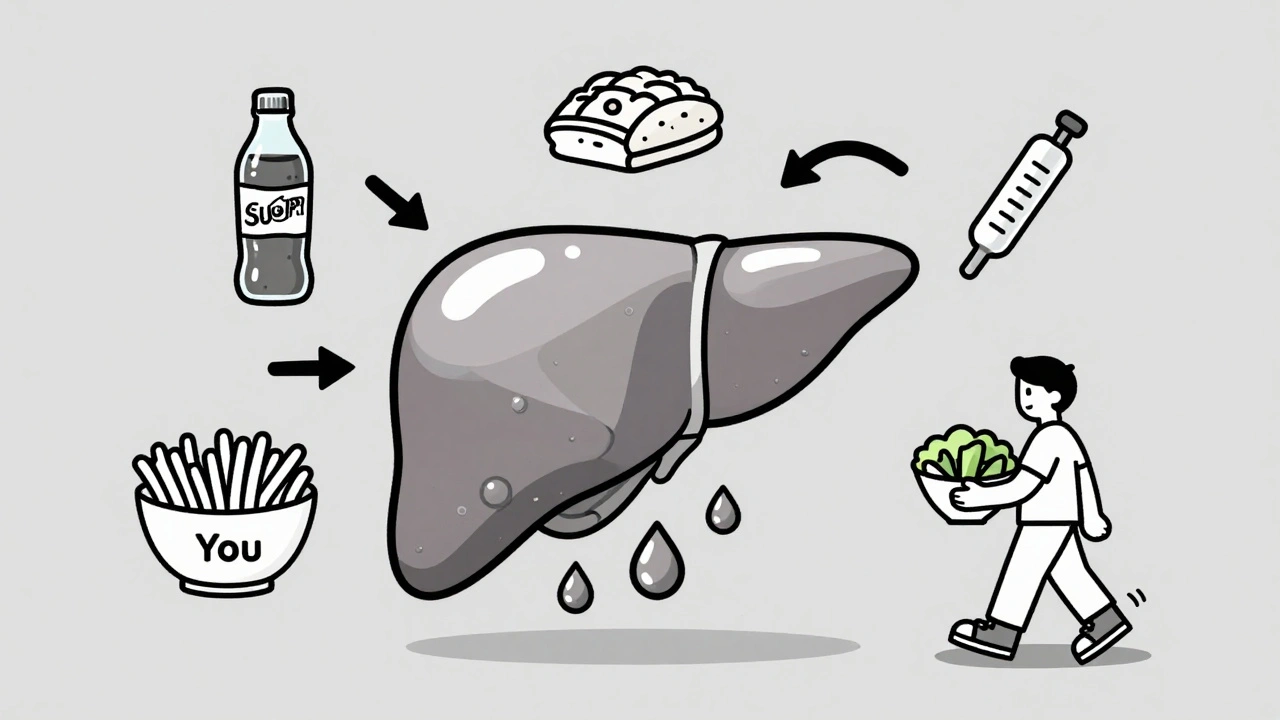
The liver doesn’t store fat by accident. About 59% of the fat that builds up comes from fat tissue breaking down too fast because of insulin resistance. Another 26% is made inside the liver from excess sugar-especially fructose from sodas and processed foods. Your liver also gets worse at burning fat and exporting it out. The result? Fat piles up, then triggers inflammation. That’s when it becomes MASH-metabolic dysfunction-associated steatohepatitis-which can lead to scarring, cirrhosis, or even liver cancer.
Weight Loss Isn’t Just Helpful-It’s the Foundation
If you do nothing else, losing weight is the single most effective thing you can do. But not just any weight loss. Losing 5% of your body weight reduces liver fat. Losing 7-10%? That’s when inflammation starts to drop and fibrosis begins to improve. In one major study, people who lost 10% or more had a 45% chance of completely reversing MASH. That’s not a small number-it’s life-changing.
How does it work? When you shed weight, your fat tissue becomes less resistant to insulin. That means fewer free fatty acids flood into your liver. Your liver also slows down its own fat-making process by about 25-35%. At the same time, it gets better at burning fat for energy. Studies using MRI scans show liver fat can drop by half in just 6 months with consistent weight loss.
Experts recommend a mix of diet and exercise: 150 to 300 minutes of moderate activity per week (like brisk walking or cycling), and eating 1,200 to 1,800 calories a day, depending on your size. The Mediterranean diet-rich in vegetables, olive oil, fish, and whole grains-has shown the best results. Cut out sugary drinks. Reduce fructose. It’s not about starving yourself. It’s about eating better.
GLP-1 Drugs: The Game-Changer
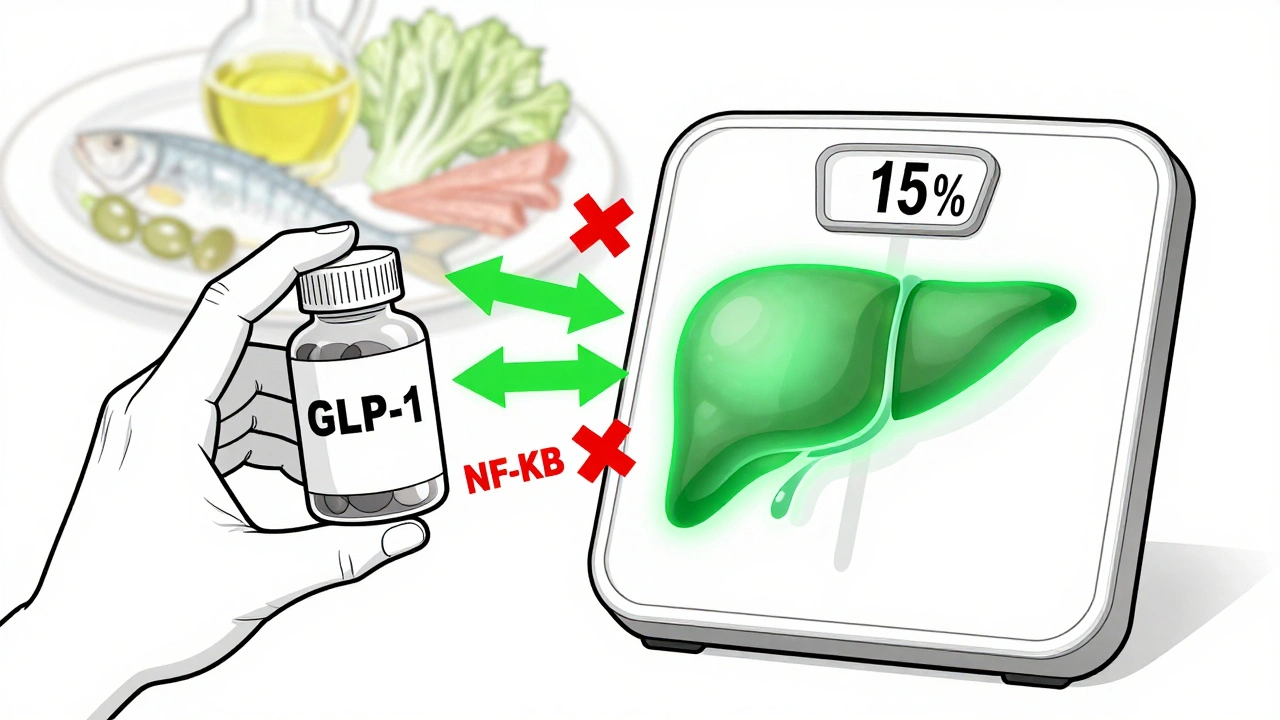
But what if you’ve tried diet and exercise and still can’t lose that last 10%? That’s where GLP-1 receptor agonists come in. These drugs-like semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda)-were originally designed for type 2 diabetes. Then they were found to cause massive weight loss. Now, they’re becoming first-line treatment for MASLD.
Semaglutide, at the 2.4 mg dose, helped people lose an average of 15% of their body weight in clinical trials. In those same trials, liver fat dropped by 55%. Liraglutide helped 39% of patients reverse MASH, compared to just 17% on placebo. Even the lower dose of semaglutide (1.0 mg), used for diabetes, led to a 52% MASH resolution rate over 72 weeks.
How do they work? They slow stomach emptying, so you feel full longer. They reduce cravings. But they also act directly on the liver: they cut down on fat production, improve insulin sensitivity, and reduce inflammation by blocking key signaling pathways like NF-κB. It’s not just weight loss doing the work-it’s the drug itself helping the liver heal.
The Real-World Challenges
These drugs aren’t magic. They’re powerful, but they come with hurdles. About 76% of people on semaglutide report nausea-some mild, some bad enough to quit. Around one in three stop within six months. That’s not failure. It’s biology. The side effects usually fade after a few weeks, but not for everyone.
Cost is another barrier. A month’s supply of semaglutide can cost over $1,300. Medicare covers it for obesity in about two-thirds of cases, but private insurance varies. Some people use meal replacement programs to stay on track-those who did saw 78% adherence, compared to just 52% with standard diet advice.
And here’s the catch: if you stop the drug, you often regain the weight-and the liver fat comes back. Long-term success requires ongoing support. That’s why clinics like Duke’s MASLD program pair medication with weekly dietitian visits, exercise coaching, and regular liver scans to track progress.
Who Benefits Most?
GLP-1 drugs work best for people with MASH and type 2 diabetes. If you’ve got both, you’re in the sweet spot. But if you have advanced scarring (stage F3 or F4 fibrosis), these drugs alone may not be enough. New drugs like resmetirom, approved in early 2024, are showing promise for advanced cases-and may one day be combined with GLP-1 therapy.
They’re not for everyone. People with a history of pancreatitis, thyroid cancer, or severe GI disorders need to be cautious. Your doctor will check your liver enzymes, kidney function, and overall health before starting.
What’s Next?
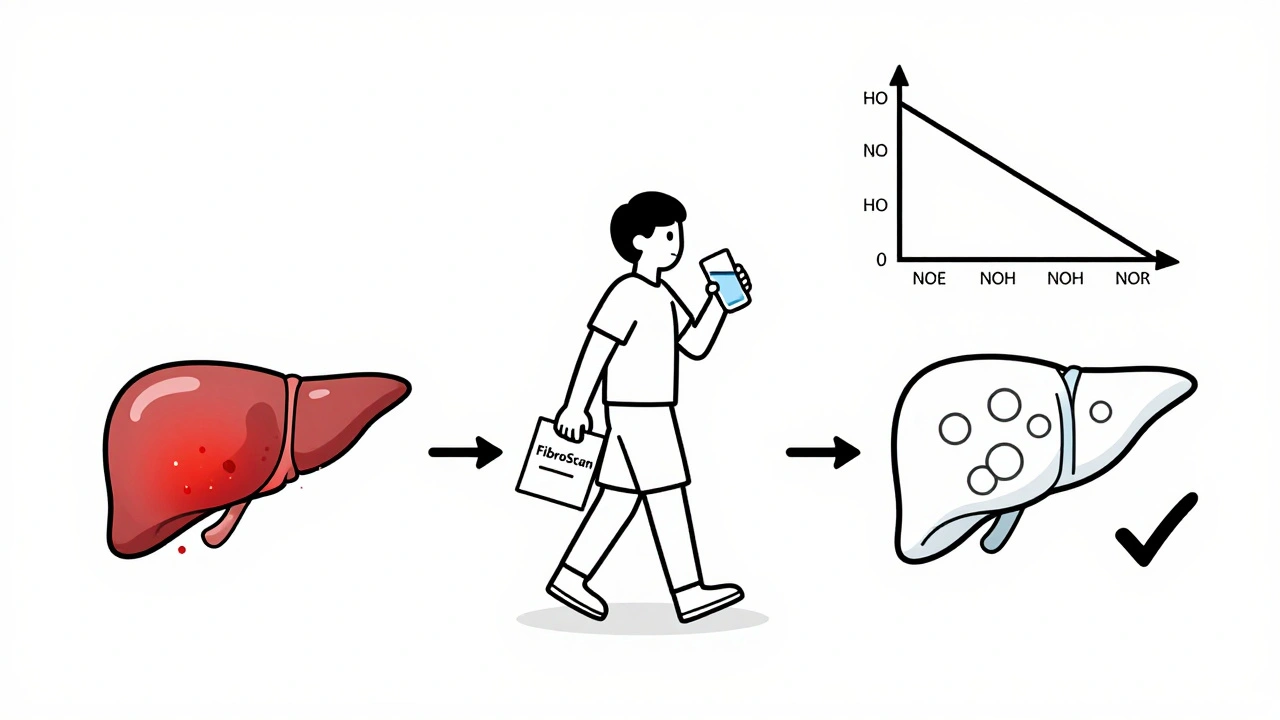
The MASLD market is exploding. It’s worth nearly $15 billion today and could hit $28 billion by 2030. Semaglutide leads the pack, but new drugs like tirzepatide (Mounjaro) are showing even better weight loss results. The FDA now accepts liver fat scans (MRI-PDFF) and FibroScan results as official measures in drug trials, which means faster approvals and better monitoring.
But the biggest shift isn’t in drugs-it’s in mindset. MASLD isn’t a side effect of being overweight. It’s a metabolic disease. And treating it means treating the whole system: diet, movement, insulin sensitivity, and inflammation. Weight loss is still the gold standard. But now, we have tools that make it possible for more people to reach it-and keep it.
What You Can Do Today
- Get a FibroScan or liver fat scan if you’re overweight or have diabetes-many primary care doctors can refer you.
- Track your waist circumference. Over 40 inches for men, 35 for women? That’s a red flag.
- Start cutting out sugary drinks. One soda a day can add 20% more liver fat over a year.
- Walk 30 minutes a day, five days a week. No gym needed.
- If you’re struggling to lose weight despite effort, ask your doctor about GLP-1 agonists. Don’t wait until your liver is scarred.
The path isn’t easy. But it’s clearer than ever. You don’t need to be perfect. You just need to start-and keep going.
Can you reverse fatty liver without losing weight?
It’s extremely rare. Fat in the liver is directly tied to excess calories and insulin resistance. Without weight loss-usually 7-10% of body weight-liver inflammation and scarring won’t improve significantly. Some medications can help reduce fat, but they work best when paired with weight loss. Lifestyle change is still the foundation.
How long does it take to see results with GLP-1 drugs for fatty liver?
Liver fat begins to drop within 8-12 weeks of starting GLP-1 therapy. In clinical trials, significant improvements in liver inflammation and fibrosis were seen at 48-72 weeks. Most patients see noticeable changes on scans by 6 months. But the full benefit-like MASH resolution-takes a year or more, especially if combined with weight loss.
Are GLP-1 drugs safe for the liver?
Yes. In fact, they’re one of the few medications proven to improve liver health in people with MASLD. While some older diabetes drugs were linked to liver stress, GLP-1 agonists reduce liver fat, inflammation, and enzyme levels. Rare cases of acute pancreatitis have been reported, but the risk is very low-about 0.3% per year. Regular monitoring is advised, especially in the first few months.
Can I take GLP-1 drugs if I don’t have diabetes?
Yes. Semaglutide (Wegovy) and liraglutide (Saxenda) are FDA-approved specifically for weight management in people without diabetes. They’re now widely prescribed for MASLD even in patients who don’t have type 2 diabetes, as long as they meet criteria for obesity or metabolic dysfunction. Your doctor will evaluate your liver fat, metabolic markers, and overall risk before prescribing.
What’s the difference between MASLD and MASH?
MASLD is the broader term for fatty liver linked to metabolic dysfunction. MASH is the more serious form-when fat in the liver causes inflammation and damage to liver cells. Think of MASLD as the early stage and MASH as the progressed stage. Not everyone with MASLD develops MASH, but those who do are at higher risk for cirrhosis and liver cancer. Treatment goals shift from reducing fat (for MASLD) to reducing inflammation and scarring (for MASH).
8 Comments
Wendy Chiridza
December 4 2025
Just cut out the soda and start walking. That’s it. No magic pills needed. I lost 12% body fat in 5 months and my liver enzymes went back to normal. Simple. Consistent. No drama.
Mark Gallagher
December 4 2025
Wow, so you’re telling me the entire medical establishment got it wrong for decades and now we’re supposed to believe some pharmaceutical company’s marketing campaign is the real solution? GLP-1 drugs are just another way to monetize obesity. The real issue is processed food subsidies and corporate greed. If you want to fix fatty liver, ban high-fructose corn syrup and stop giving tax breaks to soda companies. Not prescribe billion-dollar injectables to poor people who can’t afford them.
And don’t even get me started on how they rebranded NAFLD to MASLD. Classic rebranding to make it seem like new science. Same disease, new label, higher price tag. Wake up.
I’ve seen this movie before. Remember when statins were supposed to be the cure-all for heart disease? Now we know diet and movement matter more. Same pattern. Same players. Same profit motive.
Don’t get me wrong-I’m not saying GLP-1s don’t work. They do. But they’re a Band-Aid on a gunshot wound. The real problem is our food system. We’re being poisoned by design. And now they want us to pay $1,300 a month to un-poison ourselves? That’s not healthcare. That’s extortion.
And the fact that Medicare covers it for some but not others? That’s not a policy failure. That’s systemic cruelty disguised as medicine.
If you’re telling people to walk 30 minutes a day and cut soda, you’re not being helpful-you’re being naive. Most people don’t have the time, energy, or resources to do that. They’re working two jobs, living in food deserts, and sleeping 4 hours a night. Telling them to ‘just lose weight’ is the height of privilege.
Stop romanticizing lifestyle change like it’s a moral victory. It’s not. It’s a structural failure. And until we fix that, no drug will save us.
Katey Korzenietz
December 5 2025
Anyone else notice how the article says ‘you can reverse it’ but then spends 80% of the time talking about $1300/month injections? Classic bait-and-switch. I’ve got a cousin who lost 20lbs on a 1200-calorie diet and zero meds-no GLP-1, no surgery, just food tracking and sleep. The real story is buried under pharma fluff.
Pamela Mae Ibabao
December 6 2025
Okay but let’s be real-nobody’s gonna lose 10% of their body weight without help. I tried. I failed. Twice. Then I got on semaglutide. Lost 18% in 8 months. My FibroScan went from F2 to F0. My doctor cried. I cried. My liver is happy now. And yes, I had nausea at first. But it faded. And yes, it’s expensive. But I’m alive. And my kids don’t have to bury me at 52. So yeah, I’ll pay for it. And if you think this is just ‘pharma greed,’ you haven’t seen what happens when your liver starts failing. It’s not pretty.
Also, the Mediterranean diet? Yes. But try eating olive oil and fish when you’re working 12-hour shifts and your kid has soccer practice at 7pm. Real life isn’t a food blog.
Erik van Hees
December 7 2025
GLP-1s are great but they’re not the whole story. You know what else helps? Fasting. Not just intermittent, but 36-hour fasts 2x a week. I did it for 6 months. Liver fat dropped 40% without any meds. And I didn’t even lose much weight. Insulin sensitivity improved dramatically. Also, avoid all seed oils. They’re worse than sugar. Seriously. Look up the omega-6 to omega-3 ratio. Your liver hates it.
And if you think walking 30 minutes a day is enough, you’re kidding yourself. You need resistance training. Muscle burns fat. No exceptions. And sleep. 7+ hours. Cortisol ruins everything. You think this is just about calories? It’s about hormones. Always has been.
Also, fructose isn’t the only villain. High glycemic carbs are just as bad. Bread, rice, pasta-they all spike insulin and turn to fat in your liver. Cut them. Not just soda. Everything.
And yes, I’ve been on Ozempic. But I’m off it now. I don’t need it anymore. Because I learned how to eat. And I’m not going back.
Kevin Estrada
December 9 2025
ok so i just found out my liver fat is 25% and i’m 32 and i thought i was fine because i ‘look healthy’?? like wtf?? also why does everyone keep saying ‘just lose weight’ like i’m lazy?? i’ve tried everything. keto, intermittent fasting, gym 5x a week, i even stopped eating carbs for 3 months and nothing. then i started semaglutide and boom-15lbs in 8 weeks. my doctor said my liver looks ‘normal’ now. so yeah. i’m not ashamed. if a pill fixes your liver, why is that bad?? also i still eat pizza. just less. and i drink water now. so sue me.
Chris Jahmil Ignacio
December 9 2025
Let me guess-this article was written by a pharma rep with a medical degree. GLP-1 drugs are not a cure. They’re a dependency engine. The liver doesn’t heal because of the drug-it heals because you stop eating garbage. The drug just makes it easier to stop. But if you go back to your old habits, the fat comes back. That’s not medicine. That’s a leash.
And the rebranding from NAFLD to MASLD? That’s not science. That’s a legal maneuver to get these drugs approved faster. Same drug. Same liver. New name. New price. Same old playbook.
Did you know the FDA approved resmetirom based on a 12-week trial? Twelve weeks. That’s not a cure. That’s a marketing window. And now they’re calling it ‘breakthrough.’
Meanwhile, the real solution-whole foods, movement, sleep, stress reduction-isn’t patentable. So it gets ignored. Again.
And the fact that people are being told to ‘ask their doctor’ about these drugs? That’s not empowerment. That’s surrender. You’re being sold a solution that requires ongoing spending. A lifelong subscription to your own health.
Don’t get me wrong-I’m glad people are getting help. But don’t confuse convenience with healing. You can’t out-drug a broken system.
Gerald Nauschnegg
December 10 2025
Bro I just wanna say-this post is FIRE. I’ve been on Wegovy for 6 months. My liver fat is down 60%. I’m not ‘cured’ but I’m not dying anymore. And yeah I get nauseous sometimes but I just drink ginger tea and push through. Also I started doing bodyweight workouts at home. No gym. Just pushups and squats. And I stopped drinking energy drinks. That was my big one. Now I’m down 22lbs and my wife says I look like I’m 25 again. I’m not some genius. I just listened. And I didn’t give up. You can do it too.