Learn how to prevent and treat capecitabine‑induced mouth sores with practical oral‑care steps, diet tips, topical medicines, cryotherapy, and when to seek medical help.
Capecitabine Mouth Sores – What You Need to Know
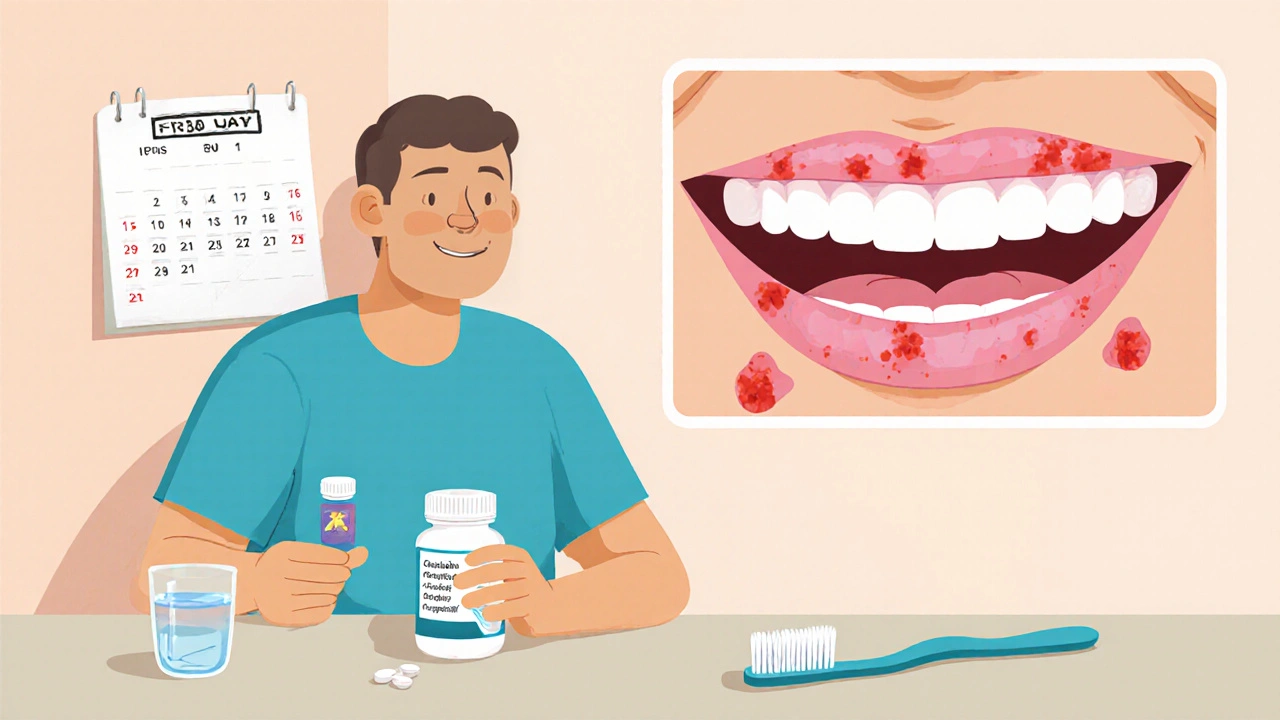
When dealing with capecitabine mouth sores, painful inflammation of the mouth lining caused by the chemotherapy drug capecitabine. Also known as capecitabine‑induced oral mucositis, it often shows up as red patches, ulcerations, or a burning sensation that can make eating and speaking difficult. The culprit, capecitabine, is an oral pro‑drug that converts to 5‑fluorouracil inside the body, targeting fast‑growing cancer cells but also affecting the lining of the gut and mouth. This side effect falls under the broader category of oral mucositis, a common challenge in chemotherapy treatment. Because the mouth’s mucosal barrier is thin, the drug’s metabolites can trigger inflammation, leading to the painful sores you may notice. Studies show that up to 40 % of patients on capecitabine develop some degree of oral mucositis, especially when the dose is high or treatment cycles are continuous. Age, poor oral hygiene, and pre‑existing gum disease raise the risk, making early detection a key step in preventing severe complications.
Practical Ways to Manage and Prevent the Sores
First, assess the severity using a standard grading scale – mild (grade 1) means soreness while eating, moderate (grade 2) adds ulceration, and severe (grade 3‑4) can force a treatment break. Nutrition is the next big piece: soft, non‑acidic foods, plenty of fluids, and supplements like whey protein can keep calories up while the mouth heals. Good oral hygiene is non‑negotiable; a soft‑bristle toothbrush, alcohol‑free fluoride rinse, and regular dental checks reduce bacterial load that could worsen inflammation. Topical agents such as benzydamine mouthwash, sucralfate suspension, or low‑dose corticosteroid gels provide direct pain relief and create a protective coating. Cryotherapy – sucking on ice chips for 30 minutes at the start of each capecitabine dose – has been shown to lower mucositis incidence by constricting blood flow and limiting drug exposure to the oral tissues. For patients who still struggle, low‑level laser therapy or photobiomodulation can accelerate healing. If sores reach grade 3 or higher, clinicians often pause the drug, reduce the dose, or switch to an alternative regimen, underscoring that supportive care is tightly linked to treatment continuity.
Understanding the link between capecitabine mouth sores and overall treatment success empowers you to act early. Keep a daily log of any tingling, redness, or difficulty swallowing and share it with your oncology team; they can adjust supportive measures before the problem spirals. Ask about prescription options like oral morphine‑based lozenges or gabapentin if pain becomes a barrier to nutrition. Remember that the same supportive strategies—rigorous oral hygiene, nutritional tweaks, and timely use of topical agents—also help with other chemotherapy‑related side effects, so mastering them pays off across your whole cancer journey. Below you’ll find a curated collection of articles that dive deeper into each of these topics, offering step‑by‑step guides, product comparisons, and expert advice to help you stay ahead of the sore‑inducing curve.