Cognitive behavioral therapy isn’t just another talk therapy. It’s the most studied, most trusted, and most widely used psychological treatment in the world. If you’ve ever felt stuck in a loop of negative thoughts - like ‘I’m a failure,’ ‘Everyone thinks I’m weird,’ or ‘Things will never get better’ - CBT gives you real tools to break free. Unlike therapies that dig deep into childhood, CBT focuses on today: your thoughts, your behaviors, and how they’re keeping you stuck. And it works. Not just a little. Studies show 60-80% of people with anxiety or depression see major improvement after just 12 sessions.
How CBT Actually Works
CBT is built on three simple ideas. First, how you think affects how you feel. Second, your behaviors reinforce your thoughts. And third, you can learn new ways to think and act that change how you feel. It’s not about positive thinking. It’s about accurate thinking.
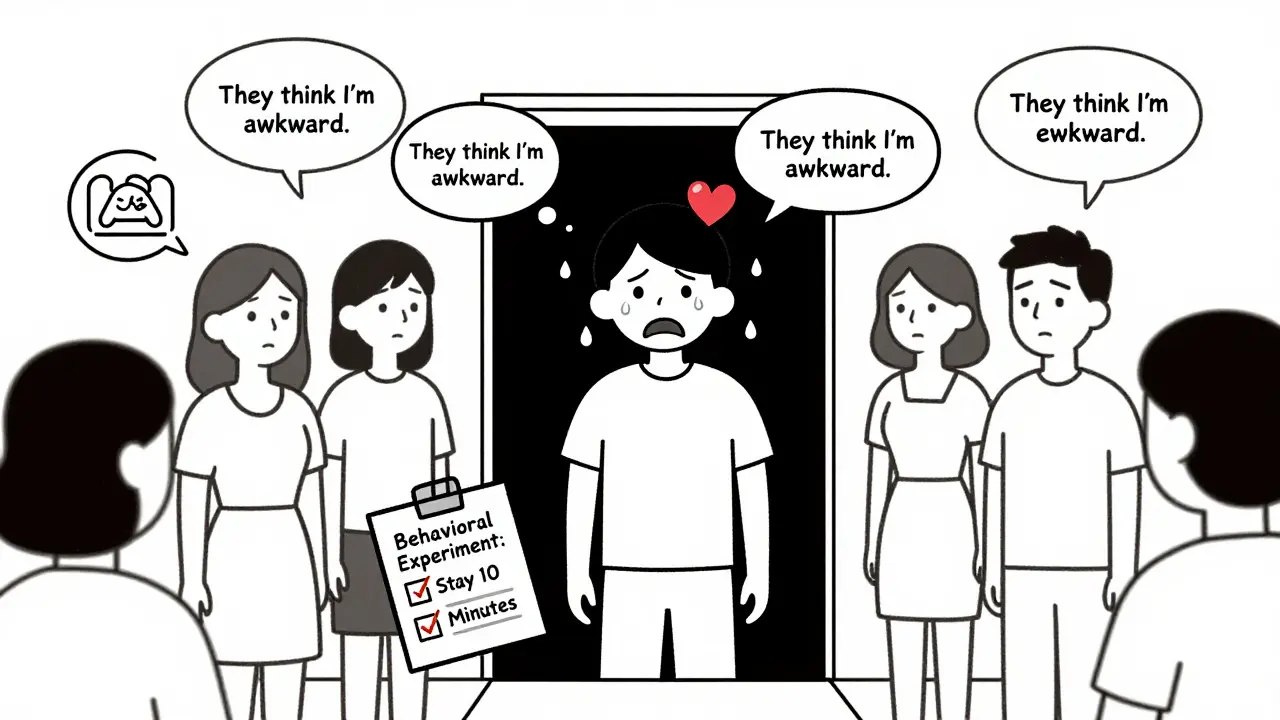
Take someone with social anxiety. They walk into a room, notice someone glancing their way, and think, ‘They think I’m awkward.’ That thought triggers physical symptoms - racing heart, sweating - and they leave early. The next time, they avoid parties altogether. Over time, the fear grows. CBT breaks this cycle. Instead of accepting ‘They think I’m awkward’ as truth, you learn to ask: ‘What’s the evidence? Could they just be looking at the door?’ You test it. You go to a party, stay for 10 minutes, and notice most people aren’t even looking at you. That’s a behavioral experiment. And it rewires your brain.
Therapists use structured tools like the 5-Part Model: Situation → Thoughts → Emotions → Behaviors → Physical Sensations. You write these down. You see patterns. You challenge distortions like ‘catastrophizing’ (‘I’ll fail and my life is over’) or ‘mind reading’ (‘They all hate me’). It’s not magic. It’s practice.
What Conditions Does CBT Help With?
CBT isn’t a one-size-fits-all. It’s a toolkit. Different techniques are used for different problems, but the core stays the same.
- Depression: Targets the cognitive triad - negative views of self, world, and future. Behavioral activation gets you moving again, even when you don’t feel like it.
- Anxiety disorders: Includes exposure therapy. If you fear flying, you don’t just talk about it. You start by looking at plane photos, then videos, then sitting in an airport, then boarding a short flight. Slowly. With support.
- PTSD: Uses exposure and cognitive restructuring to reduce the power of traumatic memories. You don’t erase them. You change how they affect you.
- OCD: Exposure and Response Prevention (ERP) is the gold standard. You touch a doorknob and don’t wash your hands. At first, anxiety spikes. Then it drops. Your brain learns: ‘Nothing bad happened.’
- Eating disorders: Challenges distorted beliefs about body image and food. ‘If I eat this, I’ll gain weight’ becomes ‘What’s the evidence for that?’
- Insomnia: CBT-I (Cognitive Behavioral Therapy for Insomnia) is more effective than sleeping pills long-term. It fixes thoughts like ‘I’ll never sleep’ and habits like lying in bed awake for hours.
The National Institute for Health and Care Excellence (NICE) in the UK recommends CBT as a first-line treatment for all these conditions. That’s not a small endorsement. It’s based on over 2,000 clinical trials.
CBT vs. Other Treatments
Is CBT better than medication? Better than other therapies? Sometimes.
For depression, a major study (STAR*D) found CBT had a 52% remission rate after 12 months. Antidepressants? 47%. But here’s the kicker: relapse rates were half as high with CBT. When people stop meds, symptoms often come back. When they stop CBT, they use the skills they learned.
Compared to other talk therapies - like psychodynamic or humanistic - CBT shows stronger results in controlled trials. One meta-analysis of 269 studies found CBT had effect sizes of 0.77-1.14 for anxiety disorders. Other therapies? 0.58-0.89. That’s not a small difference. That’s clinically meaningful.
But CBT isn’t perfect. For severe trauma or borderline personality disorder, Dialectical Behavior Therapy (DBT) often works better. For chronic pain, Acceptance and Commitment Therapy (ACT), a newer branch of CBT, shows more promise. And for kids with behavioral issues, Parent-Child Interaction Therapy outperforms standard CBT.
CBT also doesn’t work well for people with severe cognitive impairment, active psychosis, or those who can’t engage with homework. It’s active. You have to do the work.
What Happens in a Session?
Each session lasts about 50 minutes. You meet weekly for 8 to 20 weeks, depending on the issue.
Session 1: You talk about what’s bothering you. The therapist listens, then explains how CBT works. You set a goal - ‘I want to stop avoiding social events.’
Session 2-4: You learn to spot automatic thoughts. You start a thought record. For example:
- Situation: My boss didn’t reply to my email.
- Thought: ‘She’s mad at me. I’m going to get fired.’
- Feeling: Anxiety, shame
- Behavior: Avoided talking to her, worked late to ‘prove I’m competent’
Then you challenge the thought. ‘What’s the evidence she’s mad? Maybe she’s busy. What’s the worst that could happen? Even if she’s annoyed, it doesn’t mean I’m fired.’
Session 5-10: You do behavioral experiments. You test your fears. You try small exposures. You track results. You notice: ‘When I spoke up in the meeting, no one laughed. My heart didn’t explode.’
Session 11-16: You build relapse prevention. ‘What will I do if I start feeling anxious again?’ You make a plan. You keep your thought records handy. You know this isn’t a cure. It’s a skill.
Real People, Real Results
People don’t just say CBT works. They show it.
One user on HealthUnlocked, after 16 sessions of CBT for social anxiety, went from having 15 panic attacks a week to 2. They didn’t just feel better. They started attending family dinners again.
A case study in the Journal of Clinical Psychology followed someone with severe OCD. They couldn’t touch doorknobs without washing their hands 20 times. After 18 sessions of ERP - a CBT technique - they touched a doorknob and walked away. No washing. No panic. They got a job.
On Reddit, 78% of posts about CBT were positive. People raved about ‘thought records’ and ‘behavioral experiments.’ But they also said it was hard. ‘I cried during exposure,’ one wrote. ‘But I’m glad I did.’
NHS England surveyed 15,000 people who had CBT. 68% reported significant improvement. 74% completed treatment. That’s high for mental health care.
Who Can Deliver CBT?
Not every therapist is trained in CBT. Look for someone certified. In the UK, therapists need 120-180 hours of training, 20 supervised cases, and often certification from the Academy of Cognitive Therapy.
CBT is available through the NHS. You can self-refer to IAPT (Improving Access to Psychological Therapies) services. Wait times vary, but it’s free.
Private therapists charge £60-£120 per session. Many offer sliding scales. Some employers provide EAP (Employee Assistance Programs) that include CBT sessions.
There are also digital options. Woebot, an AI chatbot cleared by the FDA, delivers CBT principles through a phone app. It’s not a replacement for a therapist, but it’s a good starter tool. Studies show it helps with mild anxiety and depression.

Challenges and Misconceptions
CBT isn’t easy. And it’s not for everyone.
Most people struggle with homework. Writing thought records takes time. Exposure feels scary. One study found 45% of clients resisted doing assignments. Good therapists don’t push. They explore why. ‘What’s stopping you?’ ‘Is it too much?’ ‘Do you think it won’t help?’
Some think CBT is ‘just positive thinking.’ It’s not. You’re not told to ‘think happy thoughts.’ You’re taught to think accurately. That can mean accepting that some things are uncomfortable - and still moving forward.
Others worry it ignores the past. It doesn’t. But it focuses on how past experiences shape your current thinking - not on reliving trauma. If you need to process deep trauma, CBT can be combined with other approaches.
And yes, it can feel emotionally raw. Exposure therapy brings up fear. Challenging beliefs can shake your identity. That’s normal. It’s part of the change.
The Future of CBT
CBT isn’t stuck in the 1980s. It’s evolving.
Third-wave CBT - like ACT and Mindfulness-Based Cognitive Therapy - adds acceptance and mindfulness. Instead of fighting thoughts, you learn to notice them without getting hooked. This helps with chronic pain, burnout, and emotional numbness.
Researchers are now using AI to analyze thought records in real time. Imagine a therapist app that flags when you’re catastrophizing and gently asks: ‘Is there another way to see this?’
The National Institute of Mental Health is working on ‘precision CBT’ - matching treatment to brain patterns, not just symptoms. In 5-7 years, you might get a CBT plan based on your neural activity, not just your self-report.
But the core stays the same: thoughts matter. Behavior matters. And you can change them.
Is CBT Right for You?
Ask yourself:
- Do you want a practical, time-limited approach?
- Are you willing to do homework and try uncomfortable things?
- Do you have the cognitive ability to reflect on your thoughts?
- Are you looking for change, not just understanding?
If you answered yes, CBT could be the most powerful tool you’ve ever tried. It’s not a quick fix. But it’s a lasting one.
Start with your GP. Ask for an IAPT referral. Or search for a CBT-certified therapist through the British Association for Behavioural and Cognitive Psychotherapies (BABCP). Try a session. See if it clicks. You’ve got nothing to lose - and everything to gain.
Is cognitive behavioral therapy the same as talk therapy?
No. While CBT is a type of talk therapy, it’s much more structured. Traditional talk therapy might explore childhood or emotions in depth. CBT focuses on current thoughts and behaviors, uses specific techniques like thought records and exposure, and has clear goals and homework. It’s action-oriented, not just insight-oriented.
How long does it take to see results from CBT?
Most people start noticing changes in 4-6 weeks. For anxiety or depression, significant improvement often happens by session 8-12. Some, like those with OCD or PTSD, may need 16-20 sessions. It’s not instant, but it’s faster than most other therapies.
Can CBT help with stress, even if I don’t have a diagnosed disorder?
Absolutely. CBT isn’t just for clinical conditions. Many people use it to manage work stress, relationship tension, or perfectionism. Learning to challenge ‘I have to be perfect’ or ‘If I make a mistake, I’m a failure’ can transform daily life - even without a diagnosis.
Do I need to believe in CBT for it to work?
You don’t need to believe in it - you just need to try it. Many people are skeptical at first. But when they start writing down thoughts and testing them, they see patterns they never noticed. The evidence comes from doing, not believing.
What if I can’t afford CBT?
In the UK, you can get free CBT through the NHS via IAPT services - just ask your GP or self-refer online. There are also low-cost options through charities, universities, and online platforms like SilverCloud or Big White Wall. Free CBT workbooks are available from NAMI and the Beck Institute. Digital tools like Woebot can also help as a starting point.
Is online CBT as effective as in-person?
For mild to moderate anxiety and depression, online CBT can be just as effective - especially when guided by a therapist. But for severe symptoms, complex trauma, or when you need deep support, in-person therapy tends to work better. A 2024 meta-analysis found app-based CBT was 22% less effective than face-to-face. Choose based on your needs.

8 Comments
christian Espinola
January 18 2026
CBT is just corporate brainwashing dressed up as therapy. They don’t want you to feel better-they want you to shut up and keep working. The ‘thought records’? That’s just surveillance with a clipboard. Next thing you know, they’ll be tracking your dopamine levels via app and billing you for ‘cognitive optimization.’
And don’t get me started on ‘behavioral experiments.’ Sounds like a lab rat with a journal. You’re not fixing your brain-you’re being conditioned to tolerate oppression. Wake up.
NHS recommends it? Of course they do. It’s cheap. They’d rather give you a workbook than a real human who listens. You think your trauma is a ‘cognitive distortion’? No. It’s systemic. But hey, at least you can log your ‘irrational thoughts’ while your rent doubles.
And Woebot? An AI telling you to ‘challenge your beliefs’? That’s the dystopia we’re living in. Next they’ll replace therapists with chatbots trained on Reddit threads. Brilliant.
CBT doesn’t heal. It pacifies. And that’s the whole point.
Chuck Dickson
January 20 2026
Hey-I get why some folks are skeptical, but I’ve seen CBT change lives. I was stuck in a loop of ‘I’m not good enough’ for years. Thought records? Yeah, they felt stupid at first. But writing down ‘My boss didn’t reply → I’m fired’ and then asking ‘What’s the actual evidence?’? That changed everything.
I started small: said hi to a coworker. Didn’t die. Went to a coffee shop alone. Didn’t get laughed at. Took a 5-minute walk when I felt depressed. And guess what? The world didn’t end.
It’s not magic. It’s muscle. You build it. And yeah, it’s hard. But so is living in your own head all day. I’d rather sweat through exposure than sweat through panic attacks. If you’re even a little curious-try one thought record. Just one. You’ve got nothing to lose but the weight you’ve been carrying.
Dayanara Villafuerte
January 20 2026
OMG YES 😭 I did CBT for anxiety and it was like someone handed me a flashlight in a dark cave I didn’t even know I was in.
My ‘catastrophizing’ was wild-I’d text my friend ‘u up?’ and if they didn’t reply in 20 mins, I was convinced they hated me and were planning my funeral. 🕯️
Therapist had me write it down: Situation → Thought → Emotion → Behavior. Then we asked: ‘What’s the evidence they’re plotting your death vs. maybe they’re just asleep?’
I did an experiment: waited 2 hours. They replied: ‘Sry, fell asleep after 3 hrs of Zoom.’ 🤦♀️
My brain literally rewired. Now I say ‘they’re probably napping’ and move on. No more panic. No more crying into my cereal.
It’s not positive thinking. It’s *realistic* thinking. And honestly? It’s the most empowering thing I’ve ever done. 🙌
Andrew Qu
January 21 2026
For anyone saying CBT is ‘just positive thinking’-you’re missing the point entirely. It’s not about pretending everything’s fine. It’s about noticing when your brain is lying to you.
Like when you think ‘I messed up that presentation → I’m a failure.’ CBT asks: ‘Is that true? Or is it ‘I messed up one part’? And ‘failure’ is a label, not a fact.
I used to avoid calling my mom because I thought she’d say I’m ‘not living up to potential.’ Turns out? She just wanted to hear my voice. The thought was the problem, not her.
It’s not easy. But it’s the closest thing to self-empowerment I’ve found in mental health. You’re not broken. You’re just using faulty software. Time for an update.
Jay Clarke
January 21 2026
CBT is a Band-Aid on a gunshot wound. You think challenging thoughts fixes generational trauma? Poverty? Racism? The fact that your job pays $15/hour and you’re expected to be ‘emotionally resilient’?
They don’t want you healed. They want you functional. Productive. Quiet.
And don’t even get me started on ‘homework.’ Like I have time to write thought records between my two jobs and caring for my sick parent.
CBT is capitalism’s favorite therapy. It tells you the problem is in your head, not in the system that’s crushing you. You’re not broken. The world is. But hey-here’s a worksheet.
Next they’ll sell you a CBT app subscription. $9.99/month to fix the pain they created.
Selina Warren
January 22 2026
You’re all missing the deeper truth: CBT works because it forces you to confront the lie you’ve been living. The lie that your thoughts are facts. That your fear is prophecy.
I used to believe ‘If I’m not perfect, I’m worthless.’ That wasn’t a thought-it was a religion. CBT didn’t give me peace. It gave me war. And I needed it.
Exposure therapy? I stood in front of a mirror and said ‘I am enough’ 50 times. I cried. I screamed. I wanted to quit.
But then I realized-I wasn’t breaking my mind. I was freeing it.
This isn’t about ‘techniques.’ It’s about rebellion. Against the voice inside that’s been lying to you since you were 8.
Do the work. Even if it hurts. Because the alternative? Living as a ghost in your own life. And that’s worse than any panic attack.
Robert Davis
January 23 2026
Interesting article. Very well-structured. But I noticed something: they cite NICE guidelines and STAR*D, but don’t mention the 2018 Cochrane review that found CBT’s effect sizes shrink significantly when publication bias is accounted for.
Also, the 60-80% improvement rate? That’s based on clinician ratings, not patient-reported outcomes. And many studies use ‘treatment as usual’ controls-which often includes no therapy at all. Not exactly a fair comparison.
And let’s not forget: CBT’s efficacy drops sharply for people with comorbid personality disorders or chronic illness. The data is cherry-picked.
It’s not that CBT doesn’t help-it’s that the hype ignores the limits. And that’s dangerous. People stop meds, switch to CBT, and crash because they weren’t told it’s not a panacea.
Just saying. I’ve read the meta-analyses. You should too.
Eric Gebeke
January 25 2026
Look. I tried CBT. I did the worksheets. I did the exposure. I even bought the workbook. And you know what? It made me feel worse.
Because every time I wrote ‘I’m not good enough’ and tried to challenge it, I just felt more ashamed. Like I was failing at fixing myself.
And now I’m supposed to believe that my trauma is just ‘cognitive distortion’? That my childhood abuse is just ‘irrational thinking’?
They don’t tell you that CBT can retraumatize. That the pressure to ‘do the homework’ makes people feel broken for not being ‘fixed’ fast enough.
I’m not saying it doesn’t work for some. But for people like me? It felt like being told to smile while your house burns down.
And now they’re pushing it on kids in schools. Next thing you know, they’ll be giving CBT worksheets to grieving children.
It’s not therapy. It’s emotional labor disguised as healing.