When you pick up a prescription, you might see two options on the receipt: the name you recognize from TV ads, or a simpler, cheaper version with a strange chemical name. You might wonder - is the cheaper one just as good? The answer isn’t as simple as it seems, but the facts are clear: generic drugs work the same as brand-name medications for most people, most of the time. But not always. And knowing when it matters could save you money - or even your health.
What Exactly Makes a Drug Generic?
A generic drug isn’t a copy. It’s the exact same medicine, legally required to contain the same active ingredient, in the same strength, and delivered the same way. If your doctor prescribes lisinopril for high blood pressure, the generic version has no extra ingredients that make it work better or worse. It’s designed to do the same thing as the brand-name version, which in this case might be Zestril. The U.S. Food and Drug Administration (FDA) doesn’t approve generics lightly. To get the green light, a generic manufacturer must prove the drug delivers the same amount of active ingredient into your bloodstream at the same speed as the brand-name version. This is called bioequivalence. The FDA’s acceptable range is 80% to 125% - meaning the generic can be slightly faster or slower to absorb, but not enough to change how it works in your body. A 2016 study in the Journal of the American Medical Association looked at over 2,000 bioequivalence tests. The average difference in absorption between generics and brand-name drugs was just 3.5%. That’s less than the natural variation your body has from day to day.Why Are Generics So Much Cheaper?
Brand-name drugs cost a fortune to develop. The FDA estimates it takes an average of $2.6 billion and over a decade to bring a new drug to market. That includes years of research, clinical trials, and regulatory paperwork. Once approved, the company has a patent - usually 20 years - to be the only one selling it. During that time, they charge high prices to recoup their investment. Generics skip all that. Once the patent expires, another company can make the same drug. They don’t need to repeat expensive safety trials because the original drug’s safety and effectiveness are already proven. All they need to show is bioequivalence. That cuts their costs dramatically. The result? Generics cost 80% to 85% less. GoodRx found an average savings of 82.5% in 2022. For example, the brand-name cholesterol drug Lipitor (atorvastatin) cost around $130 a month before generics hit the market. Five years later, the generic version was under $1 a month. From 2007 to 2016, generic drugs saved the U.S. healthcare system $1.67 trillion. Medicare saved $77 billion. Medicaid saved $37.9 billion. That’s not just a convenience - it’s a lifeline for millions.Are Generics Just as Safe?
Yes. The FDA holds generic manufacturers to the same standards as brand-name companies. Same quality checks. Same factory inspections. Same rules for purity, strength, and stability. The FDA inspects over 3,500 manufacturing plants worldwide each year - whether they make brand-name or generic drugs. You might notice the pill looks different. It’s a different color. Maybe it’s oval instead of round. That’s because trademark laws prevent generics from looking exactly like the brand-name version. But that’s just the filler - the inactive ingredients like dyes, binders, or preservatives. These inactive ingredients don’t affect how the drug works. But they can matter to some people. If you’re allergic to a certain dye or have a rare sensitivity to lactose, you might react to one generic version but not another. That’s why it’s important to check the label or ask your pharmacist if you have known allergies.
When Generics Might Not Be the Same
There’s a small group of drugs where even tiny differences can cause problems. These are called narrow therapeutic index (NTI) drugs. They have a very small window between a dose that works and a dose that’s dangerous. Examples include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin and carbamazepine (anti-seizure meds)
What Do Real People Experience?
Patient reviews tell a mixed story. On Drugs.com, out of 250,000 reviews for common drugs like metformin and lisinopril, 87% of users said they couldn’t tell the difference between generic and brand-name versions. But for thyroid meds like Synthroid, that number drops. About 13% of users reported side effects - fatigue, weight gain, heart palpitations - after switching to a different generic brand. Many of them went back to the brand-name version and felt better. On Reddit’s r/Pharmacy community, one user saved $450 a month switching from Humira (a biologic) to its biosimilar. Another user said switching generics for levothyroxine made them feel like they were “constantly sick.” The pattern? For most drugs - antibiotics, blood pressure pills, statins, antidepressants - generics work fine. For NTI drugs, some people notice a difference. It’s not about quality. It’s about individual biology.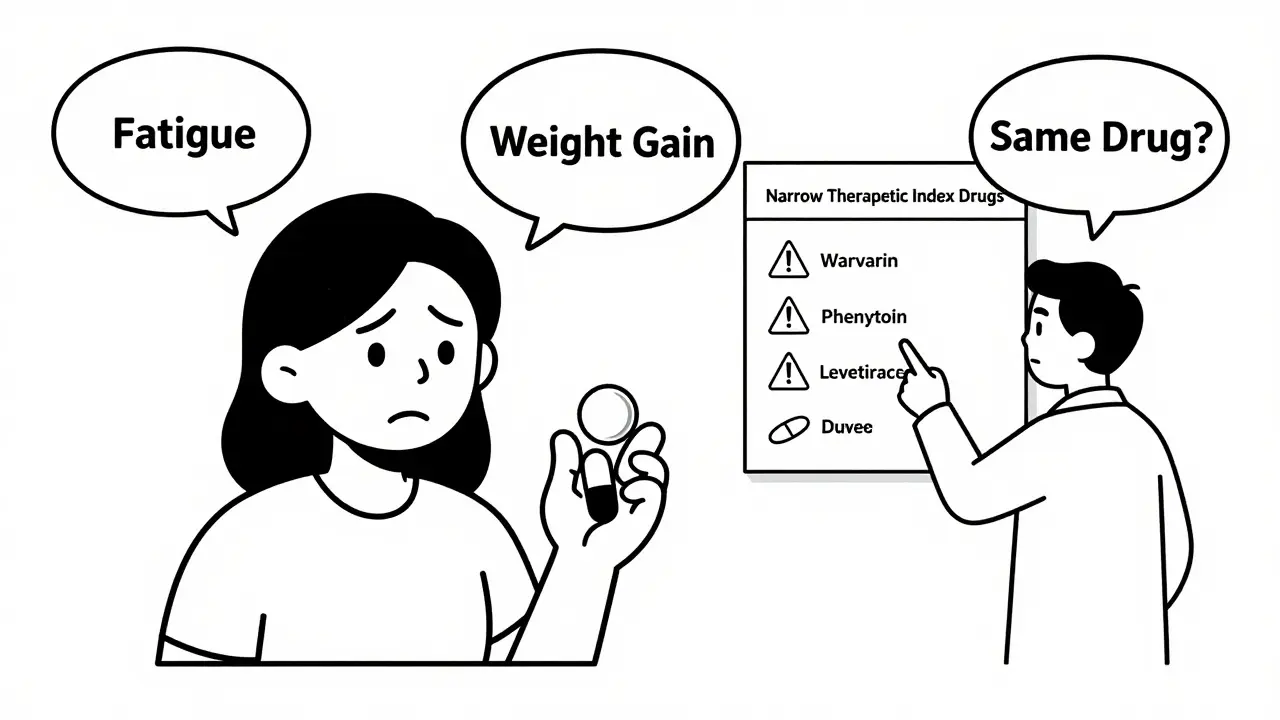
How to Use Generics Wisely
You don’t need to avoid generics. But here’s how to use them safely:- Ask your doctor: For most prescriptions, generics are the best choice. But if you’re on a narrow therapeutic index drug, ask if switching is safe.
- Stick with one manufacturer: If you find a generic that works for you, keep using it. The FDA’s Orange Book lists which generics are approved and which manufacturers make them.
- Check the pill: If your pill looks different, ask your pharmacist if it’s the same drug. Don’t assume a new shape or color means it’s a different medicine.
- Use price tools: GoodRx and SingleCare compare prices across pharmacies. Sometimes the brand-name version is cheaper than a generic at a different store.
- Know your rights: In 49 states, pharmacists can swap a brand-name drug for a generic unless your doctor writes “dispense as written.” You can always ask for the brand if you prefer - but you’ll pay more.
The Bigger Picture: Why This Matters
The U.S. spends more on prescription drugs than any other country. Brand-name drugs make up only 11% of prescriptions, but 74% of total drug spending. Generics make up 90% of prescriptions but only 26% of spending. That gap is shrinking. As more blockbuster drugs like Humira lose patent protection, biosimilars - the generic version of complex biologic drugs - are starting to enter the market. In 2022, biosimilars saved $3.2 billion in the U.S. alone. The FDA is also working on faster approvals for complex generics - like inhalers and creams - which used to take years to develop. In 2022, they approved 12 complex generics. Five years ago, it was just three. But challenges remain. Over 170 generic drugs were in shortage in 2022, mostly because manufacturing issues or raw material shortages. Many generics are made overseas, and inspections show 18% of foreign plants had compliance issues - compared to 8% in the U.S. Still, the trend is clear: generics are the future of affordable medicine. The World Health Organization predicts global generic use will rise from 56% to 70% of all prescriptions by 2030.Final Takeaway
For 9 out of 10 prescriptions, generic drugs are just as safe and effective as brand-name ones - and dramatically cheaper. If you’re on a common medication like metformin, atorvastatin, or sertraline, there’s no reason not to use the generic. But if you’re on a drug that needs precise dosing - like warfarin, levothyroxine, or an anti-seizure medicine - don’t switch without talking to your doctor. Consistency matters. If you feel different after a switch, speak up. Your body might be telling you something. The goal isn’t to avoid generics. It’s to use them smartly. You deserve affordable care. And you deserve care that works.Are generic drugs as effective as brand-name drugs?
Yes, for most drugs. The FDA requires generics to have the same active ingredient, strength, and bioequivalence as the brand-name version. Studies show they work the same in 90% of cases. The only exceptions are narrow therapeutic index drugs like warfarin or levothyroxine, where even small changes in absorption can affect outcomes.
Why do generic pills look different?
By law, generic drugs can’t look exactly like the brand-name version - that’s to avoid trademark infringement. Differences in color, shape, or size come from different inactive ingredients like dyes or fillers. These don’t affect how the drug works, but they can cause confusion. Always check the label or ask your pharmacist if you’re unsure.
Can I switch between different generic brands?
For most medications, yes. But for narrow therapeutic index drugs - like thyroid meds, blood thinners, or seizure drugs - switching between manufacturers can cause problems. If you notice changes in how you feel after switching, talk to your doctor. You may need to stick with one brand or request the original brand-name version.
Why are some generic drugs more expensive than others?
Price varies based on how many manufacturers make the drug. When a patent first expires, only a few companies make the generic, so prices stay high. Over time, more companies enter the market, and prices drop - sometimes to pennies per pill. If one generic is expensive, try another pharmacy or use a price-comparison tool like GoodRx.
Is it safe to take generics made overseas?
Yes. The FDA inspects all manufacturing facilities - whether in the U.S., India, China, or elsewhere - using the same standards. About 18% of foreign plants had compliance issues during inspections in 2022, compared to 8% in the U.S. But that doesn’t mean the drugs are unsafe. The FDA still approves them only if they meet quality and safety requirements. If you’re concerned, ask your pharmacist where the drug is made.

13 Comments
Stephen Rock
January 21 2026
Look, I don't care what the FDA says. I switched my levothyroxine to a generic and spent three weeks feeling like a zombie. My TSH went nuts. They call it 'bioequivalence' like it's magic. It's not. Your body isn't a lab rat.
Amber Lane
January 21 2026
I used to be skeptical too. Then I saved $400/month on my blood pressure med and didn't feel a thing. Sometimes simple works.
Andrew Rinaldi
January 22 2026
It's funny how we treat medicine like it's one-size-fits-all. We accept that people have different tastes in coffee or music, but when it comes to pills, we assume biology should conform to a spreadsheet.
Gerard Jordan
January 24 2026
Generics saved my dad’s life 💙 He’s on 5 meds now, all generic, and he’s hiking at 78. The system ain’t perfect, but it works for most. Don’t let fear stop you from saving money 🙌
Samuel Mendoza
January 25 2026
You're all idiots. The FDA is corrupt. Generic manufacturers bribe inspectors. I read a blog that said 70% of them use talc from China that's laced with asbestos.
Glenda Marínez Granados
January 27 2026
Ah yes, the classic 'I feel different' argument. Next you'll say your aura changed when the pill turned from blue to white. 😏
Coral Bosley
January 27 2026
I switched to generic sertraline and went from feeling like I could breathe to crying in the shower for no reason. I didn't want to be that person who's 'too sensitive'... but my therapist said my blood levels were all over the place. They don't talk about this enough.
MAHENDRA MEGHWAL
January 28 2026
In India, generic medications are the cornerstone of public health. We rely on them for millions. The manufacturing standards are stringent, and the cost-effectiveness is unparalleled. It is a matter of both science and social responsibility.
Dee Monroe
January 29 2026
I used to think generics were just cheaper versions of the same thing... until I realized they're not just cheaper-they're revolutionary. They let a single mom in rural Ohio afford her insulin. They let a veteran in Texas get his heart meds without choosing between pills and groceries. This isn't about chemistry. It's about dignity. And if you're worried about a 3% absorption difference when your life depends on it? Maybe you've never had to choose between rent and refills. The system isn't perfect, but these pills? They're hope in capsule form.
Ben McKibbin
January 30 2026
The FDA’s 80–125% bioequivalence window is mathematically sound, but it ignores pharmacokinetic variability across populations. For NTI drugs, even a 5% shift in Cmax can be clinically significant. That’s why neurologists and endocrinologists push back. This isn't anti-generic-it's pro-precision.
Melanie Pearson
January 30 2026
Foreign manufacturing? 18% non-compliance? That’s unacceptable. We should ban all overseas generics. American jobs. American standards. American safety. This isn't a debate-it's a betrayal.
Rod Wheatley
February 1 2026
If you're on warfarin? DON'T SWITCH WITHOUT TALKING TO YOUR DOCTOR!! I'm a pharmacist-I've seen people end up in the ER because they got a different generic and their INR spiked. Same pill, different filler, different results. Ask your doc for the brand if it works. No shame in that. And if you're on levothyroxine? Stick with one brand. Period. Your thyroid doesn't care about your budget.
Jerry Rodrigues
February 2 2026
I’ve been on the same generic metformin for 8 years. No issues. Pill looks different every time. Doesn’t matter. I take it. I feel fine. Sometimes the simplest answer is the right one.