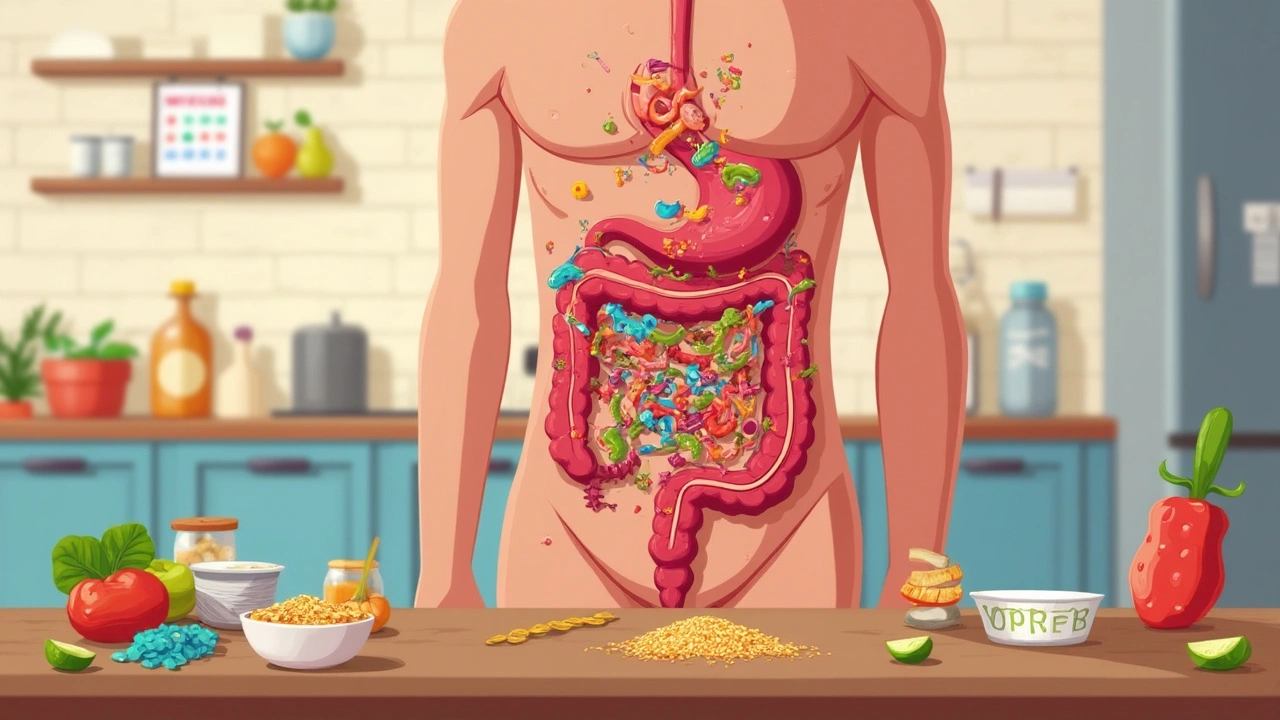
Did you know that more than 100 trillion bacteria live in your gut? It sounds wild, but this invisible community—known as your gut microbiome—handles way more than you might guess. These tiny bugs help you digest food, keep your immune system on track, and yes, they can have a massive impact on your bathroom habits, especially if you're stuck with chronic diarrhea.
Chronic diarrhea means you’re dealing with loose, urgent stools for more than four weeks. It’s not only about what you eat; sometimes, it’s about how those gut bacteria process your food. If you're wondering why your stomach won't settle down, your gut bugs could be sending signals you can’t see but definitely feel.
Curious how changing your diet or picking the right probiotic could actually make a difference? Or when that endless upset means you should call your doctor? Let’s get into what’s really going on inside your digestive system—and some no-nonsense tips that could help you get your routine (and your life) back on track.
- Why Gut Bacteria Matter
- When Gut Balance Goes Wrong
- Signs Your Microbiome Needs Help
- How Diet Influences Gut Bugs
- Probiotics, Prebiotics, and Real-life Fixes
- When to See a Doctor
Why Gut Bacteria Matter
Your gut works a bit like a busy city filled with trillions of bacteria, known as your gut bacteria or microbiome. These tiny organisms do a lot more than just hang out in your belly—they help break down food, make vitamins, control inflammation, and even fight off the bad bugs that try to make you sick.
Think of gut bacteria as your body’s crew for keeping things running smoothly. When this system gets off-balance—let’s say after a round of antibiotics or from eating too much junk food—it can mess up your digestion in a big way. That’s where chronic diarrhea comes in. When certain bacteria start taking over, or helpful ones disappear, your gut can’t absorb water and nutrients like it should, and things get messy fast.
You might be surprised how much bacteria matter for more than just your bathroom schedule. Some gut bugs help keep your immune system strong, train your body not to freak out over harmless foods, and even send signals to your brain. When your microbiome is healthy, your whole system works better. But tip the balance, and all sorts of digestive symptoms—like diarrhea that just hangs on—can hit.
Check out how diverse your gut is compared to other parts of your body:
| Body Part | Approximate Number of Bacterial Species |
|---|---|
| Gut | Up to 1,000 |
| Skin | 200-500 |
| Mouth | 500-700 |
See that? Your gut is hands-down the most crowded and lively place in your body when it comes to bacteria. That means small changes—diet, stress, even travel—can create big shifts in your gut community and how you feel day to day.
When Gut Balance Goes Wrong
So, what actually messes up your gut bacteria and triggers chronic diarrhea? It’s all about balance. Your gut is home to both "good" and "bad" bugs. When everything’s even, digestion runs smoothly. But if the "bad" guys take over, that’s when trouble starts. This off-balance state is called dysbiosis, and it can hit you harder than you might think.
Let’s look at a few usual suspects that can throw your gut bacteria out of whack:
- Antibiotics: Wiping out bad bacteria often means the good ones get caught in the crossfire. Suddenly, you don't have enough friendly bacteria to keep things running right.
- Diet high in processed foods: Junk food and tons of added sugars feed the bad bugs, and starve the good ones that thrive on fiber and real food.
- Infections: Stomach bugs or food poisoning can wipe out the balance fast, leading to ongoing digestive issues even after you “recover.” One well-known culprit is C. diff bacteria, which can explode after antibiotics and cause severe, ongoing diarrhea.
- Chronic stress: Your gut actually “talks” to your brain. If you’re always stressed, it ramps up gut inflammation and can mess with your microbiome makeup.
Studies show that people with chronic diarrhea often have lower levels of key "good" bacteria, like Lactobacillus and Bifidobacterium. At the same time, there’s an increase in certain "bad" species that produce toxins or pump out irritating chemicals.
| Trigger | How it Affects Gut Bacteria |
|---|---|
| Antibiotic Use | Kills both good and bad bacteria, causing long-term imbalance |
| Poor Diet | Feeds harmful bugs, reduces beneficial species |
| Gut Infection | Can cause explosive growth of bad bacteria |
| Stress | Promotes inflammation and alters gut bug balance |
There’s also something called small intestinal bacterial overgrowth, or SIBO, where bacteria move into the wrong part of your gut and multiply. This can mess up digestion, trigger bloating, and cause—you guessed it—ongoing diarrhea.
If you keep getting flare-ups, it’s worth thinking back on your medical history: antibiotics, sickness, changes in diet, or extra stress. Finding the root cause can help you and your doctor figure out what to tackle first. The bottom line? When gut bugs go rogue, your bathroom schedule can get completely out of hand.
Signs Your Microbiome Needs Help
Your gut bugs aren't just sitting around—they're working full-time jobs to keep things moving smoothly. But when things go sideways in your gut bacteria world, your body starts dropping hints. So, how do you know when your microbiome is out of whack, especially if you’re wrestling with chronic diarrhea?
Here’s what to pay attention to:
- Stomach issues that won't go away—think bloating, constant gas, or painful cramps alongside that persistent diarrhea.
- Frequent, hard-to-control trips to the bathroom. If you’re running for the toilet several times a day, day after day, that's a red flag.
- Mysterious food sensitivities. Foods that used to be fine may suddenly turn against you and make symptoms worse.
- Unexplained fatigue or brain fog. It sounds odd, but gut issues can make you feel tired or fuzzy-headed. This link is real.
Your immune system also counts on the right gut bugs to keep germs in check. When the balance is off, people often notice they get sick more often or struggle to shake mild infections—like colds or sniffles—because their gut is distracted by inflammation caused by bacterial misfires.
| Common Sign | What It Might Mean |
|---|---|
| Persistent loose stools | Gut bacteria aren't breaking down food properly or are too few in number. |
| Bloating after eating | Certain bacteria may be overgrowing and producing extra gas. |
| Unexplained tiredness | Poor gut health may mess with energy levels and nutrient absorption. |
| More colds than usual | Weakened immune system due to unhealthy microbiome. |
One study out of Stanford looked at people with ongoing digestive issues and found a much lower variety of helpful gut bugs compared to healthy folks. So if you feel stuck with symptoms, your digestive health ecosystem might just need some extra attention.

How Diet Influences Gut Bugs
If you want to change your gut bacteria, your diet is your steering wheel. Everything you eat feeds either the good guys or the troublemakers in your gut. This means your food choices can be the difference between steady digestion and the endless cycle of chronic diarrhea.
Let’s break it down. Fiber is a superstar here. Foods like oats, beans, bananas, and even garlic feed your gut’s good bacteria. When these bugs munch on fiber, they make stuff called short-chain fatty acids. These help keep your gut lining strong and may calm inflammation that sometimes drives diarrhea.
On the flip side, diets heavy in sugar, greasy fried foods, or a lot of alcohol can stir up the bad bugs. Fast food or sugary snacks? These can throw your microbiome off, sometimes making diarrhea worse or sticking around longer.
There’s real science behind this. A study at Stanford found people who upped their fiber had more diverse gut bacteria within two weeks. That’s shorter than it takes to binge a TV show. Other research links too little fiber to more gut troubles and symptoms like bloating, gas, or runs to the bathroom.
So what should go on your plate? Here’s a quick starter list for your digestive health:
- Whole grains (brown rice, quinoa, whole oats)
- Veggies (especially leafy greens, carrots, and artichokes)
- Beans and lentils
- Low-sugar fruits (like berries and bananas)
- Fermented foods (think yogurt with live cultures, kefir, sauerkraut)
If you’ve had chronic diarrhea for a while, you might want to ease fiber in slowly. Too much at once can actually make things feel worse before they get better. Hydration is key, too; fiber pulls in water, so keep sipping to help things move smoothly.
Here’s a table for a quick look at how some common foods affect your gut bugs:
| Food | Gut Bug Impact | Tip for Sensitive Stomachs |
|---|---|---|
| Yogurt (with live cultures) | Boosts good bacteria | Choose plain, no added sugar |
| Fried foods | Feeds bad bacteria | Limit if experiencing symptoms |
| Whole grains | Supports microbiome diversity | Start with small portions |
| Soda & candy | Encourages harmful bug growth | Swap for fruit or water |
Takeaway: The microbes in your gut eat what you eat. Simple swaps at every meal can help turn things around. If you’re not sure what’s helping or hurting your gut, try tracking what you eat and how you feel for a week. Sometimes patterns pop up that make the mystery clearer—and solutions much easier.
Probiotics, Prebiotics, and Real-life Fixes
Let’s get straight to it—when you hear about probiotics and prebiotics, it’s not just health food hype. These are real tools that can actually shake up the balance of your gut bacteria and possibly help with chronic diarrhea.
Probiotics are live bacteria you can get from foods or supplements. You’ve probably seen them in yogurt, kefir, and fermented stuff like sauerkraut or kimchi. They mostly include strains from the Lactobacillus and Bifidobacterium families. When you add these ‘good bugs’ to your digestive system, you might be helping crowd out the troublemakers that set off your diarrhea in the first place. There’s evidence that certain probiotics, especially Saccharomyces boulardii and Lactobacillus rhamnosus GG, can cut down the number of episodes and the length of time you’re running to the bathroom.
Prebiotics aren’t bacteria—they’re special fibers and carbs that your body can’t digest, but your healthy gut bugs love them. You’ll find prebiotics in bananas (especially when they’re a little green), onions, garlic, leeks, and oats. When you eat these foods regularly, you’re basically feeding the good bacteria and helping them take over.
- Add a serving of plain yogurt or kefir to breakfast
- Throw a handful of sliced bananas or berries in your cereal
- Use onions or garlic in most home-cooked meals
- Try oatmeal instead of sugary cereal
- Snack on a little sauerkraut or kimchi if you’re feeling adventurous
If you want to supplement, look for probiotics with at least a few billion CFUs (colony-forming units) and make sure the label lists the strains, not just “probiotic.” Everybody’s gut is different, so it can take a couple of weeks to notice changes, and not every product works for every person. If you’ve got serious gut issues or a weakened immune system, run new supplements by a doctor.
Some folks find that cutting back on super processed foods and adding more fiber (think fruits, veggies, and whole grains) makes their gut bugs happier. But if you ramp up fiber too fast, you might get more gas or cramping—so increase slowly if you’re not used to it.
| Food | Type | Benefit for Gut Bacteria |
|---|---|---|
| Yogurt (with live cultures) | Probiotic | Adds good bacteria |
| Green banana | Prebiotic | Feeds healthy bacteria |
| Kimchi | Probiotic | Supports gut diversity |
| Onions | Prebiotic | Boosts beneficial bugs |
No single food or supplement is going to magically fix chronic diarrhea, but tackling it from different angles—like boosting your microbiome with the right foods and habits—gives you a real shot at dialing down symptoms for good.
When to See a Doctor
There’s only so much home remedies and yogurt can do if your gut’s in turmoil. When chronic diarrhea hangs around for weeks, it’s not just annoying—it can signal bigger health issues that need real answers, not guesswork.
If you notice any of the red flags below, it's time to stop googling and get checked out:
- Diarrhea lasts longer than four weeks
- You see blood, mucus, or pus in your stool
- Unexplained weight loss, persistent cramping, or severe bloating
- Signs of dehydration, like dry mouth, extreme thirst, less peeing, or dizziness
- Fever above 101°F (38.3°C) or severe weakness
Doctors usually want to rule out infections, digestive health conditions like Crohn’s or colitis, or even issues with your gut bacteria. Sometimes they’ll suggest stool tests to check for bugs, blood work to catch signs of inflammation, or breath tests that actually measure how your microbiome is working.
People over 60, kids, or anyone with a weak immune system shouldn’t wait things out, either. Quick medical care can keep things from snowballing into dangerous territory (like severe dehydration or kidney issues).
Here’s a quick look at when getting checked is crucial:
| Warning Sign | Why See a Doctor? |
|---|---|
| Blood in stool | Could be infection, inflammation or something more serious |
| High fever | May point to aggressive infections needing antibiotics |
| Lasts over 4 weeks | Chronic diarrhea may reveal treatable conditions |
| Severe dehydration | Dangerous if not treated; can lead to hospitalization |
If something feels off or your gut just won’t get back to normal, don’t tough it out. Most causes of chronic diarrhea are manageable with the right care—and figuring out if your gut bacteria are the real culprit is often step one to getting your life (and your bathroom schedule) back in order.
15 Comments
Jennifer Grant
April 28 2025
When we contemplate the bustling metropolis that is our gut, it becomes evident that the microbiome functions less like a random assortment of microbes and more like an interdependent civilization whose collective actions dictate the harmony of our entire organism; each bacterial strain, from Lactobacillus to Bifidobacterium, occupies a niche akin to a skilled artisan contributing to the grand tapestry of digestion, immune modulation, and even neurochemical signaling. The chronic diarrhea many experience can be interpreted as a civil unrest within this micro‑society, where the equilibrium has been shattered by external invasions such as indiscriminate antibiotics or the relentless flood of processed sugars that feed the rogue factions. Historically, scholars have noted that humans co‑evolved with these microorganisms, forging a symbiotic pact that allowed for the extraction of nutrients otherwise inaccessible, a pact now jeopardized by modern dietary habits. In the same way that a city's infrastructure crumbles without proper maintenance, our intestinal lining suffers when the protective short‑chain fatty acids produced by fiber‑fermenting bacteria dwindle, leading to increased permeability and fluid loss that manifests as diarrheal episodes. Furthermore, the gut‑brain axis, a bidirectional communication highway, transmits inflammatory signals that can amplify the urgency and frequency of bowel movements, reinforcing a vicious cycle of dysbiosis. Clinical studies underscore that patients with prolonged loose stools frequently exhibit reduced microbial diversity, suggesting that the loss of keystone species removes essential metabolic pathways. Recolonization strategies, such as targeted probiotic supplementation, aim to reintroduce beneficial strains, but their efficacy hinges upon the existing environmental conditions within the gut, much like planting seeds in barren soil will not flourish without amendment. Incorporating prebiotic fibers acts as a fertilizer, encouraging the growth of resident good bacteria and restoring the delicate balance disturbed by dietary excesses. The importance of hydration cannot be overstated, as water serves as the medium for microbial fermentation and the transport of nutrients, yet excessive fluid loss without adequate replacement exacerbates electrolyte imbalances, compounding the problem. In practice, a gradual increase in soluble fiber-through foods like oats, legumes, and bananas-can ameliorate symptoms over weeks, while abrupt spikes may provoke transient bloating before benefits emerge. It is also prudent to monitor for potential pathogen overgrowth, such as Clostridioides difficile, which can dominate after broad‑spectrum antibiotic courses and precipitate severe, refractory diarrhea. When such red flags appear, medical intervention becomes indispensable to avoid systemic complications. Ultimately, the path to recovery rests upon a holistic appreciation of the gut ecosystem, recognizing that nurturing our internal microbial city through diet, lifestyle, and, when necessary, clinical support can transform chronic diarrhea from a relentless nuisance into a manageable condition. This perspective invites us to view our bodies not as solitary machines but as collaborative habitats where tiny inhabitants wield outsized influence.
Kenneth Mendez
May 7 2025
America's food labs are cooking up the real cure, not these foreign probiotic gimmicks.
Gabe Crisp
May 17 2025
One must acknowledge that personal responsibility plays a central role; constantly consuming processed snacks without regard for gut health reflects poor moral choices. The body is a temple, and neglecting it invites needless suffering. While medical interventions exist, they are no substitute for disciplined eating habits. In addition, the spread of misinformation about quick fixes undermines genuine progress. Therefore, each individual bears the duty to cultivate a balanced microbiome through mindful consumption.
Paul Bedrule
May 26 2025
From a systems‑theoretic perspective, the gut microbiome operates as a complex adaptive network, wherein perturbations-such as antibiotic-induced dysbiosis-propagate nonlinear cascades that destabilize homeostatic set‑points. The ensuing phenotypic manifestation, namely chronic diarrhea, can be modelled via differential equations that incorporate microbial turnover rates, substrate fluxes, and host immune feedback loops. Intervention protocols thus require a multi‑modal approach integrating prebiotic substrate provisioning, targeted probiotic strain inoculation, and immunomodulatory support to recalibrate the network dynamics toward a resilient attractor state.
yash Soni
June 4 2025
Wow, look at all these "science" tricks. Just stop eating junk and drink water, simple.
Emily Jozefowicz
June 13 2025
Ah, the glorious parade of fermented foods-kefir, kimchi, sauerkraut-like tiny superheroes donning capes of lactic acid, battling the villainous overgrowth of bad bugs. Yet, some folks think a spoonful of yogurt will instantly banish the chaos; reality prefers a slow, steady march. Adding a dash of prebiotic fiber is like giving those good bacteria a gourmet buffet, encouraging them to multiply and fortify the gut walls. Remember, moderation is key; overdoing the fiber can backfire with gas and cramping.
Franklin Romanowski
June 23 2025
I totally get how frustrating chronic diarrhea can be, especially when it feels like your body is betraying you. It helps to think of your gut as a garden that needs the right balance of soil, water, and sunlight-fiber, hydration, and low‑sugar foods give it the conditions to thrive. Starting with small changes, like swapping white bread for whole‑grain or adding a spoonful of plain yogurt, can make a real difference over a few weeks. Also, keep track of how you feel after meals; patterns often emerge that point to specific triggers. If symptoms persist, a chat with a healthcare provider can rule out infections or deeper issues. Hang in there, the body has an amazing capacity to heal when given the right tools.
Brett Coombs
July 2 2025
Everyone keeps preaching “just eat more fiber” like it’s a universal fix, but what about the folks who can’t tolerate it? Some people get bloated, crampy messes from even a little bran. Maybe the real issue is hidden pathogens, not just diet.
John Hoffmann
July 11 2025
Grammar check: The article correctly notes that probiotics must contain specific strains; however, many commercial products lack proper labeling, which can mislead consumers. Also, the claim about short‑chain fatty acids improving gut barrier function is well‑supported by peer‑reviewed studies. It would be helpful to cite the exact journal for the fiber‑diversity correlation mentioned.
Shane matthews
July 20 2025
Interesting points about hydration but maybe add that electrolytes matter too when diarrhea lasts weeks.
Rushikesh Mhetre
July 30 2025
Hey folks! If you’re battling chronic runs, start with a simple three‑day log-track what you eat, when you go, and any extra symptoms. Then, gradually add a serving of fermented food; watch for improvements. Remember to sip water constantly, and if you feel dizzy, add a pinch of salt or an oral rehydration solution. Keep the momentum, and you’ll see the gut settle down!
Sharath Babu Srinivas
August 8 2025
👍 Probiotics can be great, but don’t expect miracles-consistency is 🔑. Also, watch out for added sugars in flavored yogurts, they can fuel bad bugs 😬.
Halid A.
August 17 2025
For those seeking a structured approach, consider the following protocol: (1) Conduct a stool analysis to identify dysbiosis patterns; (2) Implement a low‑FODMAP diet for two weeks to reduce fermentable substrates; (3) Introduce a high‑quality probiotic containing Lactobacillus rhamnosus GG and Bifidobacterium longum at a dosage of at least 10⁹ CFU daily; (4) Gradually increase dietary fiber sources such as oats and legumes while monitoring tolerance; (5) Re‑evaluate symptoms and repeat microbiome testing after six weeks to assess shifts. This evidence‑based sequence maximizes the likelihood of restoring microbial equilibrium and alleviating chronic diarrhea.
Brandon Burt
August 26 2025
Well, after reading all that, I guess we’ve got a whole cookbook of gut fixes-fiber, yogurt, water, doctors-pretty much everything you’d expect. Not sure why people think there’s a mystery, but ok.
Gloria Reyes Najera
September 5 2025
Honestly, all this “science” stuff is just a way for foreign companies to sell you pills, we should stick to good old home remedies.