Immunosuppressants keep transplanted organs alive but come with serious risks like infection, cancer, and organ damage. Learn how to take them safely, avoid rejection, and live longer with your transplant.
Transplant Medication: What You Need to Know About Immunosuppressants and Long-Term Care
When you get a new organ, your body sees it as an invader. That’s where transplant medication, drugs that suppress the immune system to prevent organ rejection. Also known as immunosuppressants, it is the only thing standing between your new kidney, heart, or liver and your body’s natural defense system. Without these drugs, rejection can happen in days—or even hours. But taking them isn’t just about swallowing pills. It’s a lifelong commitment that affects your diet, your sleep, your risk of infection, and even your chance of developing certain cancers.
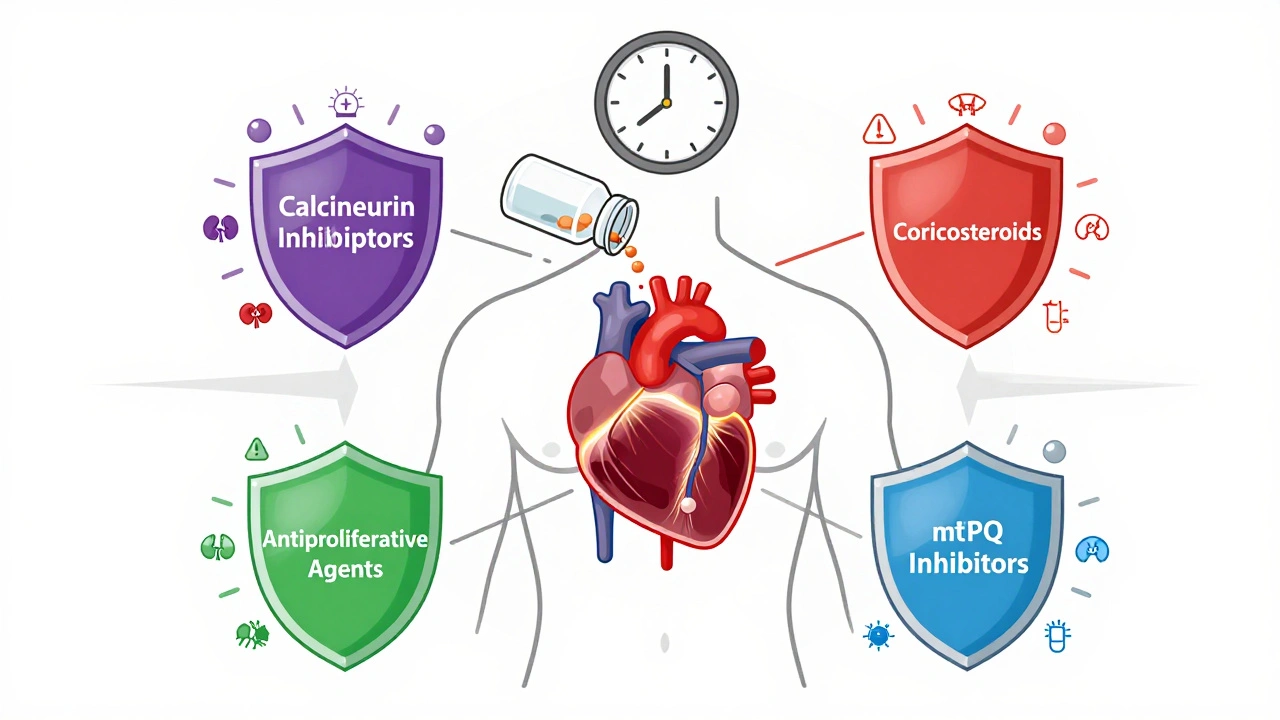
Immunosuppressants, a class of drugs that reduce immune system activity to prevent organ rejection after transplantation. Also known as anti-rejection drugs, it includes common names like tacrolimus, cyclosporine, mycophenolate, and sirolimus. Each one works differently. Some block signals that tell immune cells to attack. Others stop cells from multiplying. Doctors often mix them to get the best results with the least side effects. But they all share one big problem: they make you more vulnerable. A cold can turn into pneumonia. A small cut can get infected. And you can’t just stop taking them if you feel fine—rejection doesn’t always come with warning signs.
That’s why medication adherence, the practice of taking prescribed drugs exactly as directed, which is critical for transplant patients to avoid rejection. Also known as drug compliance, it is the single biggest factor in long-term transplant success. Miss a dose? You risk rejection. Take too much? You risk kidney damage, high blood pressure, or even diabetes. Many patients struggle with this. The pills are expensive. The side effects are real—tremors, weight gain, hair loss, nausea. And there’s no immediate reward for taking them. You don’t feel better when you take them. You just don’t get worse. That’s hard to stay motivated for. But studies show that even one missed dose per month doubles your chance of losing the transplant.
And then there are the drug side effects, unwanted physical reactions caused by transplant medications, including increased infection risk, kidney damage, and metabolic changes. Also known as medication complications, they vary by drug and person. Some people get high blood sugar. Others gain weight fast. Some develop high cholesterol or bone thinning. A few get skin cancers from years of sun exposure while on these drugs. That’s why regular blood tests, skin checks, and doctor visits aren’t optional—they’re survival tools. You can’t just rely on how you feel. Your numbers tell the real story.
You’ll find posts here that show you how to handle the daily grind: how to organize your pill schedule so you never miss one, what to do when you’re traveling and your meds are lost, how to talk to your pharmacist about cost, and how to spot early signs of rejection before it’s too late. You’ll learn how some patients use QR codes on their prescription bottles to get instant dosage reminders, how patient assistance programs can cut drug costs by 90%, and why some transplant survivors live longer than others—not because of luck, but because of how they manage their meds. This isn’t about theory. It’s about real people who stayed alive by being smart with their drugs. You can do it too.